Korean J Radiol.
2003 Mar;4(1):46-53. 10.3348/kjr.2003.4.1.46.
Thymic Epithelial Tumors Classified According to a Newly Established WHO Scheme: CT and MR Findings
- Affiliations
-
- 1Department of Diagnostic Pathology, Department of Medicine Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. melon2@samsung.co.kr
- 2Department of Radiology and Center for Imaging Science, Department of Medicine Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Department of Thoracic Surgery, Department of Medicine Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Division of Pulmonary and Critical Care Medicine, Department of Medicine Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 754042
- DOI: http://doi.org/10.3348/kjr.2003.4.1.46
Abstract
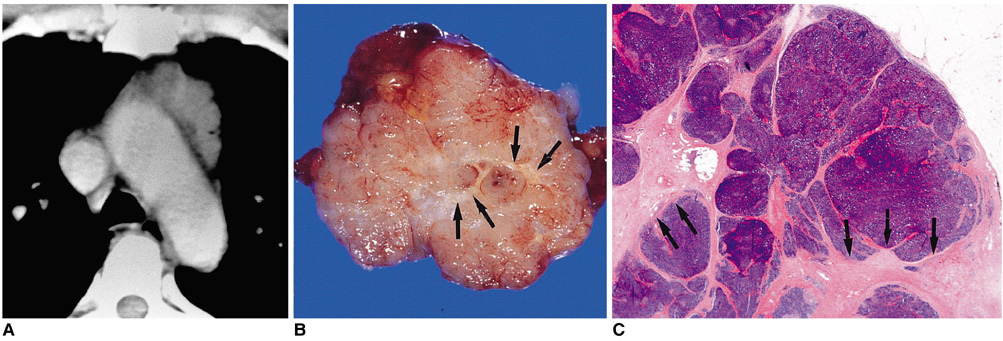
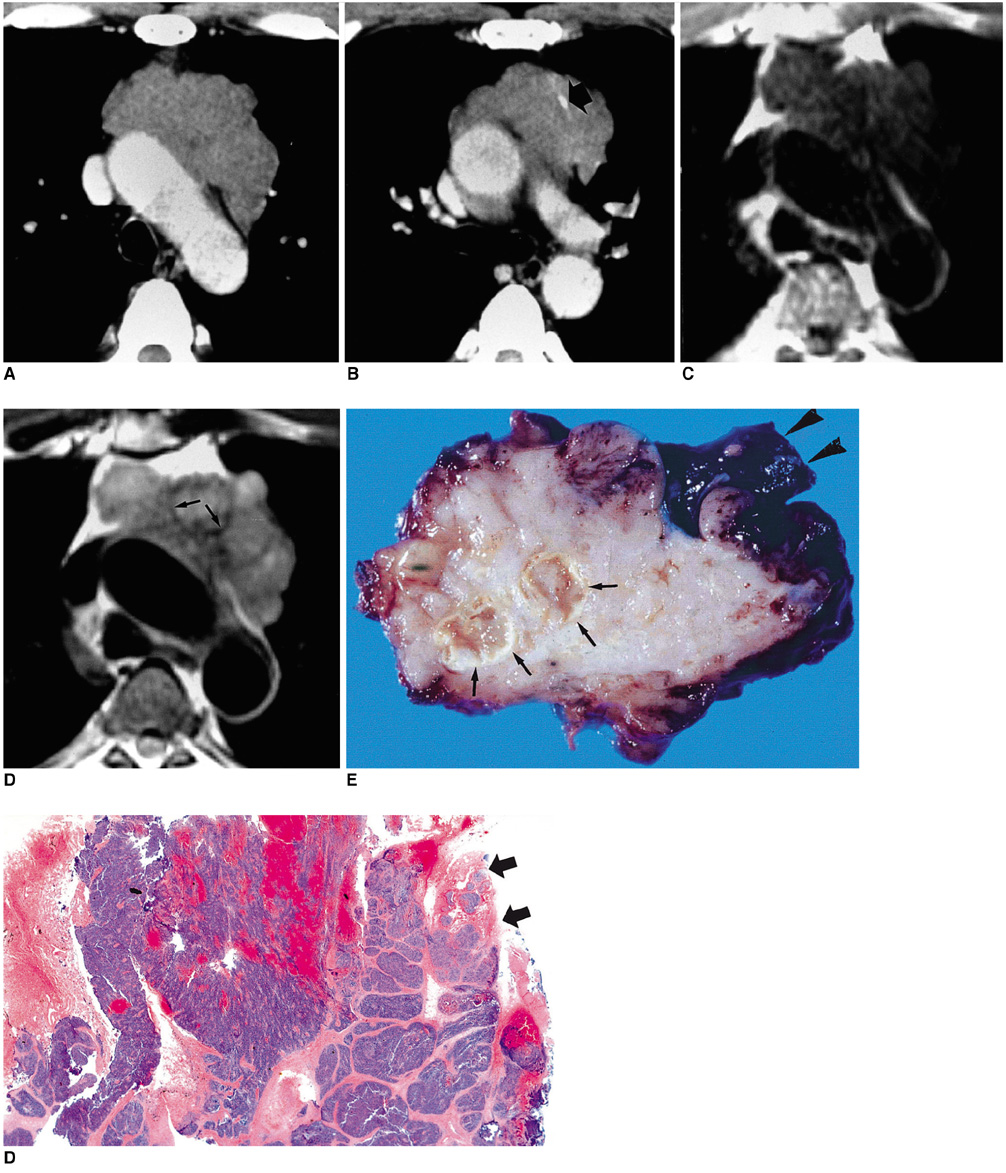
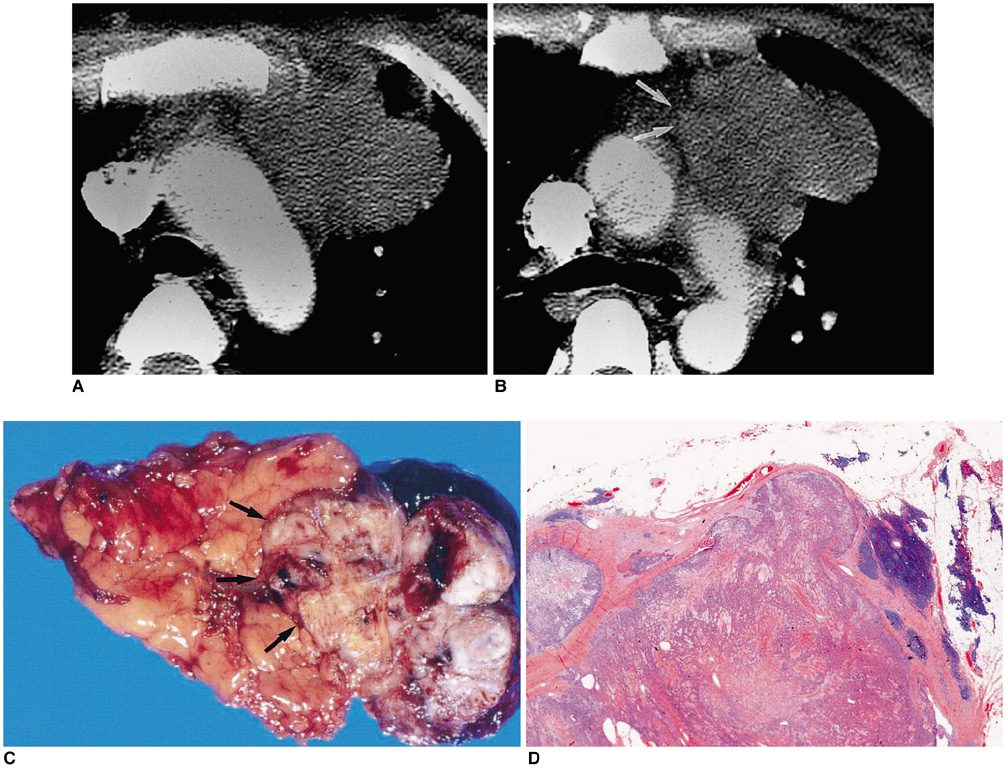
- Thymic epithelial tumor is a distinctive pathologic entity exhibiting variable histologic features and heterogeneous oncologic behavior. Among the various classification systems, that of the World Health Organization has been adopted because of good correlation between histologic appearance and oncologic behavior. Radiologically, a smooth contour and round shape are most suggestive of a type-A tumor, whereas an irregular contour most strongly suggests type C. Pleural seeding is rare in type-A and AB tumors; calcification is suggestive of type B. Type-C tumors are significantly larger and more commonly associated with lymphadenopathy than type B3. At T2-weighted MR imaging, lobular internal architecture is more prominent in types B1, B2, and B3 tumors than in others. However, imaging findings among the various types overlap to some extent, and the ability of imaging studies to differentiate types AB, B1, B2, and B3 is limited.
Keyword
Figure
Reference
-
1. Shimosato Y, Mukai K. Tumors of the mediastinum. Atlas of tumor pathology. 1997. Washington, DC: Armed Forces Institute of Pathology;3rd series, fascicle 21.2. Rosai J, Sobin LH. Histological typing of tumors of the thymus. International histological classification of tumours. 1999. 2nd ed. New York: Springer.3. Tomiyama N, Müller NL, Ellis SJ, et al. Invasive and non-invasive thymoma: distinctive CT features. J Comput Assist Tomogr. 2001. 25:388–393.4. Tomiyama N, Johkoh T, Mihara N, et al. Using the World Health Organization classification of thymic epithelial neoplasms to describe CT findings. AJR Am J Roentgenol. 2002. 179:881–886.5. Jung KJ, Lee KS, Han J, Kim J, Kim TS, Kim EA. Malignant thymic epithelial tumors: CT-pathologic correlation. AJR Am J Roentgenol. 2001. 176:433–439.6. Suster S, Moran CA. Thymoma, atypical thymoma, and thymic carcinoma: A novel conceptual approach to the classification of thymic epithelial neoplasms. Am J Clin Pathol. 1999. 111:826–833.7. Müller-Hermelink HK, Marino M, Palestro G. Pathology of thymic epithelial tumors. Curr Top Pathol. 1986. 75:207–268.8. Okumura M, Miyoshi S, Fujii Y, et al. Clinical and functional significance of WHO classification of human thymic epithelial neoplasms. A study of 146 consecutive tumors. Am J Surg Pathol. 2001. 25:103–110.9. Okumura M, Ohta M, Tateyama H, et al. The World Health Organization histologic classification system reflects the oncological behavior of thymoma: a clinical study of 273 patients. Cancer. 2002. 94:624–632.10. Do YS, Im J-G, Lee BH, et al. CT findings in malignant tumors of thymic epithelium. J Comput Assist Tomogr. 1995. 19:192–197.11. Herold CJ, Zerhouni EA. Higgins CB, Hricak H, Helms CA, editors. The mediastinum and lungs. Magnetic resonance imaging of the body. 1992. 2nd ed. New York: Raven Press.12. Molina PL, Siegel MJ, Glazer HS. Thymic masses on MR imaging. AJR Am J Roentgenol. 1990. 155:495–500.13. Ikezoe J, Takeuchi N, Johkoh T, et al. MRI of anterior mediastinal tumors. Radiat Med. 1992. 10:176–183.14. Sakai F, Sone S, Kiyono K, et al. MR imaging of thymoma: radiologic-pathologic correlation. AJR Am J Roentgenol. 1992. 158:751–756.15. Kushihashi T, Fujisawa H, Munechika H. Magnetic resonance imaging of thymic epithelial tumors. Crit Rev Diagn Imaging. 1996. 37:191–259.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Immunoexpression of Ki-67, Bcl-2, p53, and Tyrosine Kinase Receptors in Thymic Epithelial Tumors; Their Correlation with the WHO Histologic Subtypes and the Prognostic Value
- (18)F-FDG PET/CT is Useful for Pretreatment Assessment of the Histopathologic Type of Thymic Epithelial Tumors
- Anterior Mediastinal Tumor
- Thymic Carcinoma Presenting Two Independent Nodules: Case Report
- Expression of bcl-2 , p53 Protein and Aggressiveness in Thymic Epithelial Tumor