Obstet Gynecol Sci.
2024 May;67(3):261-269. 10.5468/ogs.23277.
Cervical cancer in Thailand: 2023 update
- Affiliations
-
- 1Department of Faculty of Medicine, Mahasarakham University, Maha Sarakham, Thailand
- 2Department of Faculty of Pharmaceutical Sciences, Ubon Ratchathani University, Ubon Ratchathani, Thailand
- KMID: 2555509
- DOI: http://doi.org/10.5468/ogs.23277
Abstract
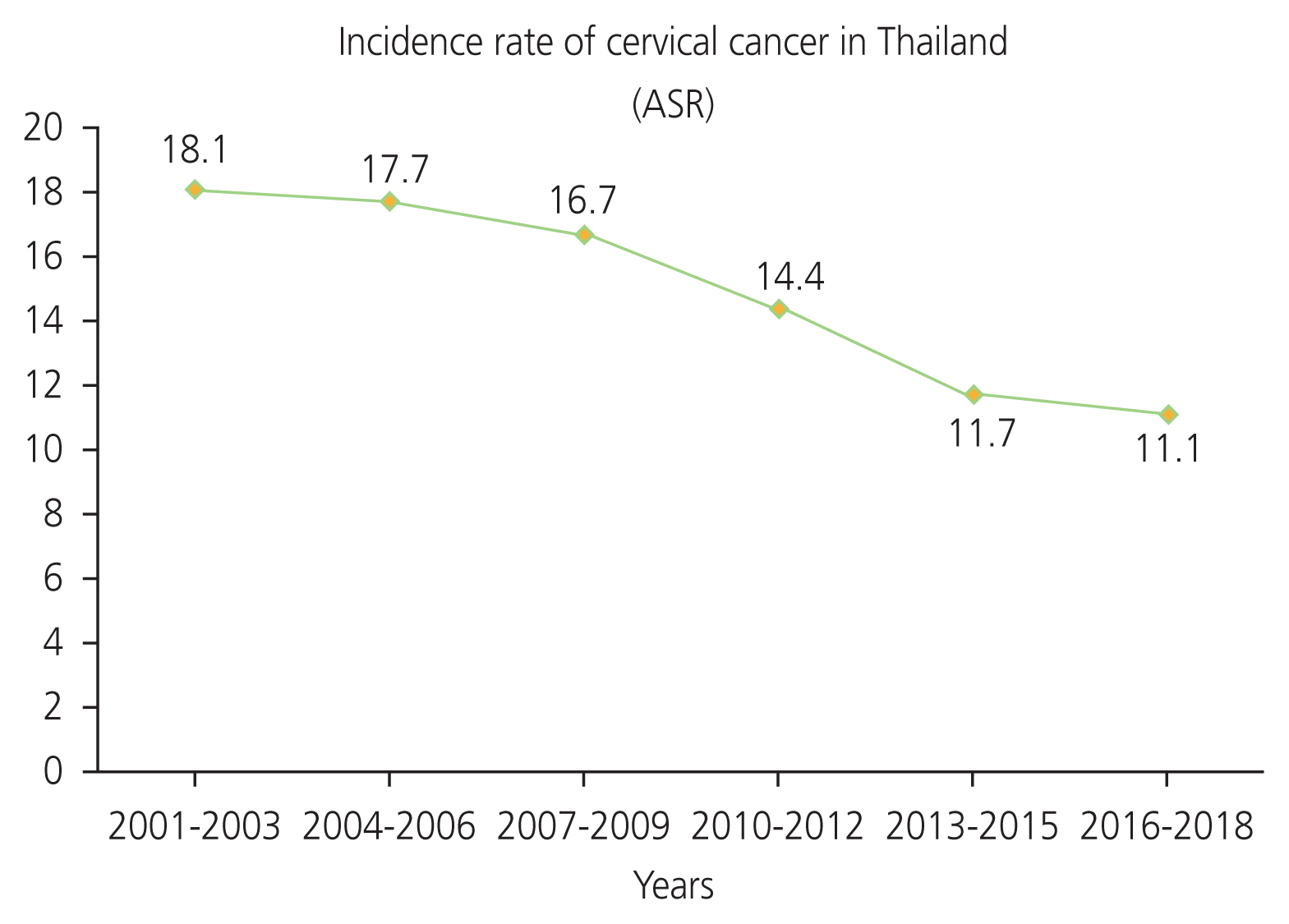
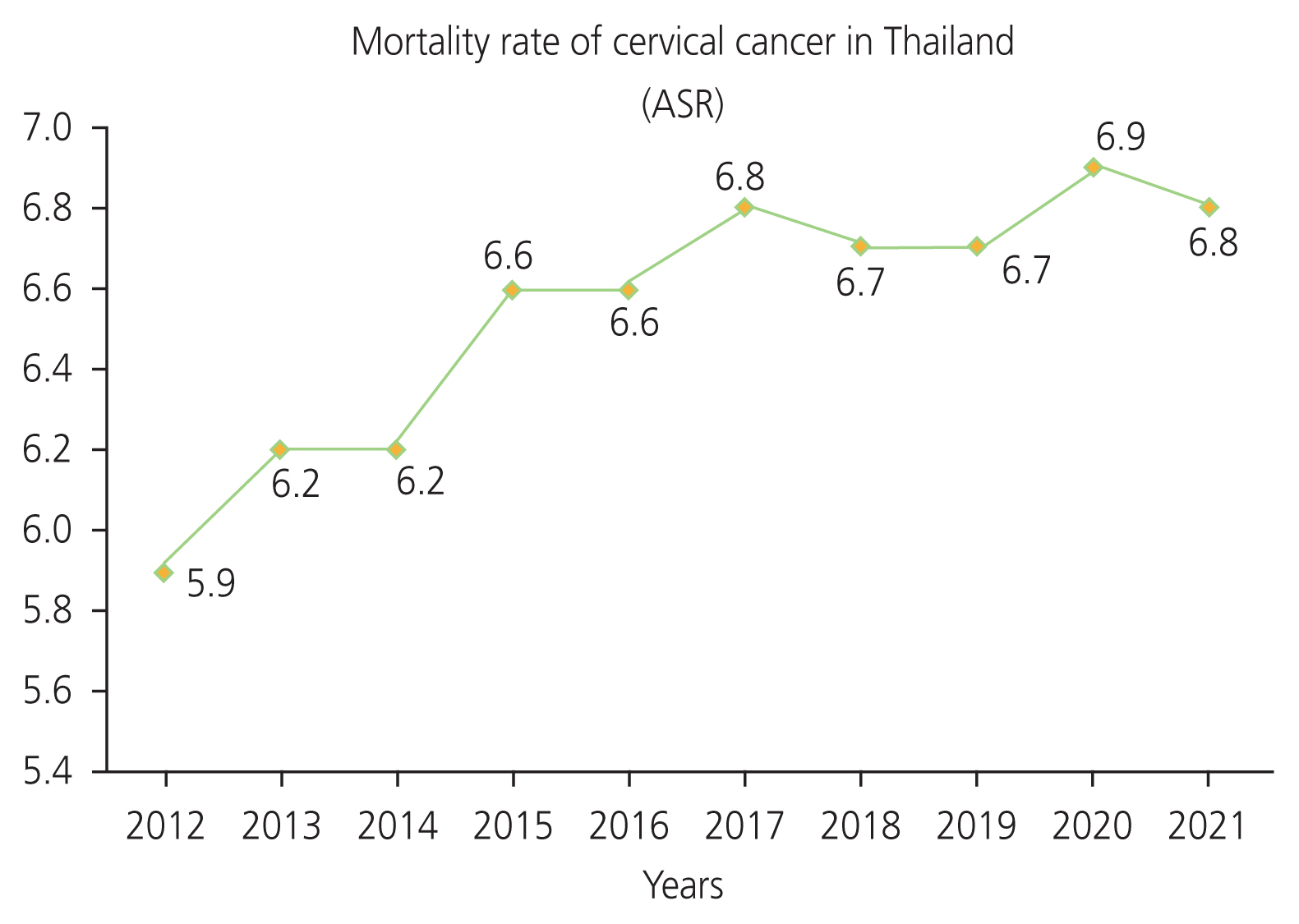
- Cervical cancer continues to pose a challenge to the health of Thai women, as the second most common cancer after breast cancer. Since high-risk human papillomavirus (HPV) types are the main cause for cervical cancer, cervical cancer screening and HPV vaccination are necessary to reduce the incidence of this disease. At present, the World Health Organization hopes to reduce the incidence of cervical cancer to 4 or less cases per 100,000 women-years using 90%- 70%-90% intervention by 2030. The first intervention involves vaccinating 90% of women aged 15 years with the HPV vaccine. The second intervention involves screening 70% of women between the ages of 35 and 45 years using a high-performance screening test. The third intervention involves detecting cervical lesions in 90% of affected women to enable diagnosis and treatment. In this context, this study reviews trends in the incidence and mortality rates of cervical cancer in Thailand, in addition to providing an up-to-date overview of the causes and necessary risk factors for cervical cancer, as well as reporting on cervical screening and HPV vaccination rates and cervical cancer during the coronavirus disease 2019 (COVID-19) pandemic. This study may prove useful for the formulation of policy aimed at eliminating cervical cancer in Thailand, such as the implementation of a free HPV vaccine service and providing athome kits for cervical screening through clinics and pharmacies. In addition, this review also highlights the need for further research on the effects of the COVID-19 pandemic on cervical cancer screening rates in Thailand.
Keyword
Figure
Reference
-
References
1. Bhatla N, Aoki D, Sharma DN, Sankaranarayanan R. Cancer of the cervix uteri: 2021 update. Int J Gynaecol Obstet. 2021; 155(Suppl 1):28–44.
Article2. Singh D, Vignat J, Lorenzoni V, Eslahi M, Ginsburg O, Lauby-Secretan B, et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO global cervical cancer elimination initiative. Lancet Glob Health. 2023; 11:e197–206.
Article3. National Cancer Institute. Hospital-based cancer registry 2021 [Internet]. Bangkok (TH): National Cancer Institute;c2022. [cited 2023 Jun 1]. Available from: https://www.nci.go.th/e_book/hosbased_2564/index.html.4. Ministry of Public Health. Cancer in Thailand Vol. V 2001–2003 [Internet]. Bangkok (TH): National Cancer Institute;c2010. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/th/File_download/Nci%20Cancer%20Registry/Book%20Cancer%20In%20Thailand%202010%20for%20Web.pdf.5. Ministry of Public Health. Cancer in Thailand Vol. VI 2004–2006 [Internet]. Bangkok (BK): National Cancer Institute;c2012. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/th/File_download/Nci%20Cancer%20Registry/Cancer%20in%20thailand.pdf.6. Ministry of Public Health. Cancer in Thailand. Vol VII. 2007–2009 [Internet]. Bangkok (TH): National Cancer Institute;c2013. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/th/File_download/Nci%20Cancer%20Registry/Cancer%20in%20thailand_VII.pdf.7. Ministry of Public Health. Cancer in Thailand Vol. VIII 2010–2012 [Internet]. Bangkok (TH): National Cancer Institute;c2015. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/th/File_download/Nci%20Cancer%20Registry/Cancer%20in%20Thailand8.pdf.8. Ministry of Public Health. Cancer in Thailand Vol IX 2013–2015 [Internet]. Bangkok (TH): National Cancer Institute;c2018. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/th/File_download/Nci%20Cancer%20Registry/In%20Cancer%20in%20Thailand%20IX%20OK.pdf.9. Ministry of Public Health. Cancer in Thailand Vol. X 2016–2018 [Internet]. Bangkok (TH): National Cancer Institute;c2021. [cited 2023 Mar 2]. Available from: https://www.nci.go.th/e_book/cit_x/index.html.10. Ministry of Public Health. Public health statistics A.D. 2012 [Internet]. Nonthaburi (TH): Ministry of Public Health;c2013. [cited 2023 Apr 25]. Available from: https://spd.moph.go.th/wp-content/uploads/2022/11/Hstatistic55.pdf.11. Ministry of Public Health. Public health statistics AD. 2015. 1st ed. Nonthaburi: Ministry of Public Health;2016.12. Ministry of Public Health. Public health statistics A.D. 2019 [Internet]. Nonthaburi (TH): Ministry of Public Health;c2020. [cited 2023 Apr 25]. Available from: https://spd.moph.go.th/wp-content/uploads/2022/08/สถิติสาธรารณสุข.pdf.13. Ministry of Public Health. Public health statistics A.D. 2020 [Internet]. Nonthaburi (TH): Ministry of Public Health;c2021. [cited 2023 Apr 25]. Available from: https://anyflip.com/tseqz/dxml.14. Ministry of Public Health. Public health statistics A.D. 2021 [Internet]. Nonthaburi (TH): Ministry of Public Health;c2022. [cited 2023 Apr 25]. Available from: https://spd.moph.go.th/wp-content/uploads/2022/11/Hstatistic64.pdf.15. Chichareon S, Herrero R, Muñoz N, Bosch FX, Jacobs MV, Deacon J, et al. Risk factors for cervical cancer in Thailand: a case-control study. J Natl Cancer Inst. 1998; 90:50–7.
Article16. Settheetham-Ishida W, Kanjanavirojkul N, Kularbkaew C, Ishida T. Human papillomavirus genotypes and the p53 codon 72 polymorphism in cervical cancer of Northeastern Thailand. Microbiol Immunol. 2005; 49:417–21.17. Natphopsuk S, Settheetham-Ishida W, Sinawat S, Pientong C, Yuenyao P, Ishida T. Risk factors for cervical cancer in northeastern Thailand: detailed analyses of sexual and smoking behavior. Asian Pac J Cancer Prev. 2012; 13:5489–95.
Article18. World Health Organization. Comprehensive cervical cancer control: a guide to essential practice. 2nd ed. Geneva: World Health Organization;2014.19. HPV Information Centre. Thailand: human papillomavirus and related cancers, fact sheet 2023 [Internet]. Barcelona (ES): HPV Information Centre;c2023. [cited 2023 Oct 2]. Available from: https://hpvcentre.net/statistics/reports/THA_FS.pdf.20. Frazer I. Correlating immunity with protection for HPV infection. Int J Infect Dis. 2007; 11(Suppl 2):S10–6.
Article21. Stanley M. HPV - immune response to infection and vaccination. Infect Agent Cancer. 2010; 5:19.
Article22. Stanley M. Pathology and epidemiology of HPV infection in females. Gynecol Oncol. 2010; 117:S5–10.
Article23. Panatto D, Amicizia D, Trucchi C, Casabona F, Lai PL, Bonanni P, et al. Sexual behaviour and risk factors for the acquisition of human papillomavirus infections in young people in Italy: suggestions for future vaccination policies. BMC Public Health. 2012; 12:623.
Article24. Bouvard V, Wentzensen N, Mackie A, Berkhof J, Brotherton J, Giorgi-Rossi P, et al. The IARC perspective on cervical cancer screening. N Engl J Med. 2021; 385:1908–18.
Article25. Song D, Li H, Li H, Dai J. Effect of human papillomavirus infection on the immune system and its role in the course of cervical cancer. Oncol Lett. 2015; 10:600–6.
Article26. Gupta SM, Mania-Pramanik J. Molecular mechanisms in progression of HPV-associated cervical carcinogenesis. J Biomed Sci. 2019; 26:28.27. Regauer S, Reich O. The origin of human papillomavirus (HPV) - induced cervical squamous cancer. Curr Opin Virol. 2021; 51:111–18.
Article28. Alzamil L, Nikolakopoulou K, Turco MY. Organoid systems to study the human female reproductive tract and pregnancy. Cell Death Differ. 2021; 28:35–51.
Article29. Deng H, Hillpot E, Mondal S, Khurana KK, Woodworth CD. HPV16-immortalized cells from human transformation zone and endocervix are more dysplastic than ectocervical cells in organotypic culture. Sci Rep. 2018; 8:15402.
Article30. Doorbar J, Griffin H. Refining our understanding of cervical neoplasia and its cellular origins. Papillomavirus Res. 2019; 7:176–9.
Article31. Sriamporn S, Parkin DM, Pisani P, Suwanrungruang K, Pengsaa P. Behavioural risk factors for cervical cancer from a prospective study in Khon Kaen, Northeast Thailand. Cancer Detect Prev. 2004; 28:334–9.
Article32. Ishida WS, Singto Y, Kanjanavirojkul N, Chatchawan U, Yuenyao P, Settheetham D, et al. Co-risk factors for HPV infection in Northeastern Thai women with cervical carcinoma. Asian Pac J Cancer Prev. 2004; 5:383–6.33. Phuthong S, Settheetham-Ishida W, Natphopsuk S, Ishida T. Genetic polymorphisms of vitamin D receptor gene are associated with cervical cancer risk in Northeastern Thailand. Asian Pac J Cancer Prev. 2020; 21:2935–9.
Article34. Li D, Liu Y, Kong D, Papukashvili D, Rcheulishvili N, Zhao H, et al. Vitamin D receptor gene polymorphisms and the risk of CIN2+ in Shanxi population. Biomed Res Int. 2022; 2022:6875996.
Article35. Wongpratate M, Ishida W, Phuthong S, Natphopsuk S, Ishida T. Genetic polymorphisms of the human cytochrome P450 1A1 (CYP1A1) and cervical cancer susceptibility among Northeast Thai women. Asian Pac J Cancer Prev. 2020; 21:243–8.
Article36. Wu B, Liu K, Huang H, Yuan J, Yuan W, Wang S, et al. MspI and Ile462Val polymorphisms in CYP1A1 and overall cancer risk: a meta-analysis. PLoS One. 2013; 8:e85166.
Article37. Ding B, Sun W, Han S, Cai Y, Ren M, Shen Y. Cytochrome P450 1A1 gene polymorphisms and cervical cancer risk: a systematic review and meta-analysis. Medicine (Baltimore). 2018; 97:e0210.38. Settheetham-Ishida W, Wongpratate M, Phuthong S, Natphopsuk S, Ishida T. Genetic polymorphism of glutathione S-transferase and cervical cancer susceptibility in Northeastern Thailand. APJCB. 2020; 5:35–41.
Article39. Ye J, Mu YY, Wang J, He XF. Individual effects of GSTM1 and GSTT1 polymorphisms on cervical or ovarian cancer risk: an updated meta-analysis. Front Genet. 2023; 13:1074570.40. Sobti RC, Kaur S, Kaur P, Singh J, Gupta I, Jain V, et al. Interaction of passive smoking with GST (GSTM1, GSTT1, and GSTP1) genotypes in the risk of cervical cancer in India. Cancer Genet Cytogenet. 2006; 166:117–23.
Article41. Phuthong S, Settheetham-Ishida W, Natphopsuk S, Settheetham D, Ishida T. Haplotype analysis of MDR1 and risk for cervical cancer in Northeastern Thailand. Asian Pac J Cancer Prev. 2017; 18:1815–9.42. Ploysawang P, Rojanamatin J, Prapakorn S, Jamsri P, Pangmuang P, Seeda K, et al. National cervical cancer screening in Thailand. Asian Pac J Cancer Prev. 2021; 22:25–30.
Article43. Gottschlich A, Nuntadusit T, Zarins KR, Hada M, Chooson N, Bilheem S, et al. Barriers to cervical cancer screening and acceptability of HPV self-testing: a cross-sectional comparison between ethnic groups in Southern Thailand. BMJ Open. 2019; 9:e031957.
Article44. Termrungruanglert W, Khemapech N, Vasuratna A, Havanond P, Deebukkham P, Kulkarni AS, et al. The epidemiologic and economic impact of a quadrivalent human papillomavirus vaccine in Thailand. PLoS One. 2021; 16:e0245894.
Article45. Juntasopeepun P, Davidson PM, Suwan N, Phianmongkhol Y, Srisomboon J. Human papillomavirus vaccination intention among young women in Thailand. Asian Pac J Cancer Prev. 2011; 12:3213–9.46. Ratanasiripong NT, Sri-Umporn S, Kathalae D, Hanklang S, Ratanasiripong P. Human papillomavirus (HPV) vaccination and factors related to intention to obtain the vaccine among young college women in Thailand. J Health Res. 2018; 32:142–51.
Article47. Chanprasertpinyo W, Rerkswattavorn C. Human papillomavirus (HPV) vaccine status and knowledge of students at a university in rural Thailand. Heliyon. 2020; 6:e04625.48. Klinsupa W, Pensuk P, Thongluan J, Boonsut S, Tragoolpua R, Yoocharoen P, et al. O16.3 Hpv vaccine introduction in thailand. Sex Transm Infect. 2015; 91:A1–258.49. Ong SK, Abe SK, Thilagaratnam S, Haruyama R, Pathak R, Jayasekara H, et al. Towards elimination of cervical cancer - human papillomavirus (HPV) vaccination and cervical cancer screening in Asian National Cancer Centers Alliance (ANCCA) member countries. Lancet Reg Health West Pac. 2023; 39:100860.
Article50. Santhanes D, Yong CP, Yap YY, Saw PS, Chaiyakunapruk N, Khan TM. Factors influencing intention to obtain the HPV vaccine in South East Asian and Western Pacific regions: a systematic review and meta-analysis. Sci Rep. 2018; 8:3640.
Article51. Kruiroongroj S, Chaikledkaew U, Thavorncharoensap M. Knowledge, acceptance, and willingness to pay for human papilloma virus (HPV) vaccination among female parents in Thailand. Asian Pac J Cancer Prev. 2014; 15:5469–74.
Article52. Klaipuk P, Ngoenwiwatkul Y, Tantipoj C, Phanuphak N, Khovidhunkit SP. Improved knowledge about HPV in Thai women after educational intervention. JDAT-DFCT. 2019; 69:1–7.53. Chunuan S, Wiwattanawongsa K, Widayati A. A predictive model of human papillomavirus vaccination intention among young women in Southern Thailand. Pac Rim Int J Nurs Res. 2021; 25:298–311.54. World Health Organization. Coronavirus disease (COVID-19) [Internet]. Geneva (CH): World Health Organization;c2023. [cited 2023 Apr 21]. Available from: https://www.who.int/news-room/fact-sheets/detail/coronavirusdisease-(covid-19.55. Duarte MBO, Argenton JLP, Carvalheira JBC. Impact of COVID-19 in cervical and breast cancer screening and systemic treatment in São Paulo, Brazil: an interrupted time series analysis. JCO Glob Oncol. 2022; 8:e2100371.
Article56. Castanon A, Rebolj M, Pesola F, Pearmain P, Stubbs R. COVID-19 disruption to cervical cancer screening in England. J Med Screen. 2022; 29:203–8.
Article57. Fedewa SA, Star J, Bandi P, Minihan A, Han X, Yabroff KR, et al. Changes in cancer screening in the US during the COVID-19 pandemic. JAMA Netw Open. 2022; 5:e2215490.
Article58. Lucas E, Murillo R, Arrossi S, Bárcena M, Chami Y, Nessa A, et al. Quantification of impact of COVID-19 pandemic on cancer screening programmes - a case study from Argentina, Bangladesh, Colombia, Morocco, Sri Lanka, and Thailand. Elife. 2023; 12:e86527.59. Eamratsameekool W, Phumiressunthon K, Sukprasert L, Pukdeesamai P. Comparison of self-to provider-collected cervical screening with HPV DNA test at roi Et province, Thailand during COVID-19 pandemic. J Med Assoc Thai. 2023; 106:8–13.
Article60. World Health Organization. Regional implementation framework for elimination of cervical cancer as a public health problem: 2021–2030 [Internet]. New Delhi (IN): World Health Organization;c2021. [cited 2023 Apr 21]. Available from: https://www.who.int/publications/i/item/9789290228875.61. Sripan P, Chitapanarux I, Fidler-Benaoudia MM, Miranda-Filho A, Bardot A, Pongnikorn D, et al. Impact of universal health care and screening on incidence and survival of Thai women with cervical cancer: a population-based study of the Chiang Mai province. Cancer Epidemiol. 2019; 63:101594.
Article62. Ngamphaiboon N. PSY7-5 current status of HPV vaccination and HPV-associated head and neck cancer in Thailand. Ann Oncol. 2022; 33:S422.
Article63. Ministry of Public Health. Policy driving plan, Ministry of Public Health [Internet]. Bangkok (TH): Ministry of Public Health;c2023. [cited 2023 Jan 15]. Available from: https://drive.google.com/file/d/1o1g4T8FWygleLTI8RlLu5vde1hKJzvy-/view.64. Wannasin R, Likitdee N, Kelly M, Thinkhamrop K. Survival after diagnosis of cervical cancer patients at a tertiary referral hospital in Northeast Thailand. Asian Pac J Cancer Prev. 2023; 24:1759–67.
Article65. Bangsomboon P, Kittisiam T, Chaowawanit W. Survival rate of cervical cancer patients according to the 2018 FIGO staging system: a tertiary hospital based study, Vajira Hospital, Bangkok. Thai J Obstet Gynaecol. 2022; 30:60–7.66. Yun BS, Park EH, Ha J, Lee JY, Lee KH, Lee TS, et al. Incidence and survival of gynecologic cancer including cervical, uterine, ovarian, vaginal, vulvar cancer and gestational trophoblastic neoplasia in Korea, 1999–2019: Korea Central Cancer Registry. Obstet Gynecol Sci. 2023; 66:545–61.
Article67. Landy R, Sasieni PD, Mathews C, Wiggins CL, Robertson M, McDonald YJ, et al. Impact of screening on cervical cancer incidence: a population-based case-control study in the United States. Int J Cancer. 2020; 147:887–96.68. Ha HI, Chang HK, Park SJ, Lim J, Won YJ, Lim MC. The incidence and survival of cervical, ovarian, and endometrial cancer in Korea, 1999–2017: Korea central cancer registry. Obstet Gynecol Sci. 2021; 64:444–53.
Article69. eClinicalMedicine. Global strategy to eliminate cervical cancer as a public health problem: are we on track? eClinicalMedicine. 2023; 55:101842.70. Burmeister CA, Khan SF, Schäfer G, Mbatani N, Adams T, Moodley J, et al. Cervical cancer therapies: current challenges and future perspectives. Tumour Virus Res. 2022; 13:200238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic report of gynecologic cancer in Thailand
- The Growing Problem of Radiologist Shortage: Thailand’s Perspective
- Clinical practice guidelines for cervical cancer: an update of the Korean Society of Gynecologic Oncology Guidelines
- The epidemiologic status of gynecologic cancer in Thailand
- The Situation of Osteoporosis in Thailand: Update for 2010