Ann Rehabil Med.
2024 Feb;48(1):94-101. 10.5535/arm.23118.
Impact of COVID-19 Pandemic on People with Locomotor Disability in North India: A Cross-Sectional Analysis
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India
- 2Department of Sports Medicine, Sports Injury Centre, Vardhman Mahavir Medical College and Safdarjung Hospital, New Delhi, India
- 3Department of Trauma Surgery, All India Institute of Medical Sciences, Mangalagiri, India
- 4Department of Physical Medicine and Rehabilitation, Government Medical College, Haldwani, India
- 5Department of Biostatistics and Health Informatics, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Lucknow, India
- KMID: 2553166
- DOI: http://doi.org/10.5535/arm.23118
Abstract
Objective
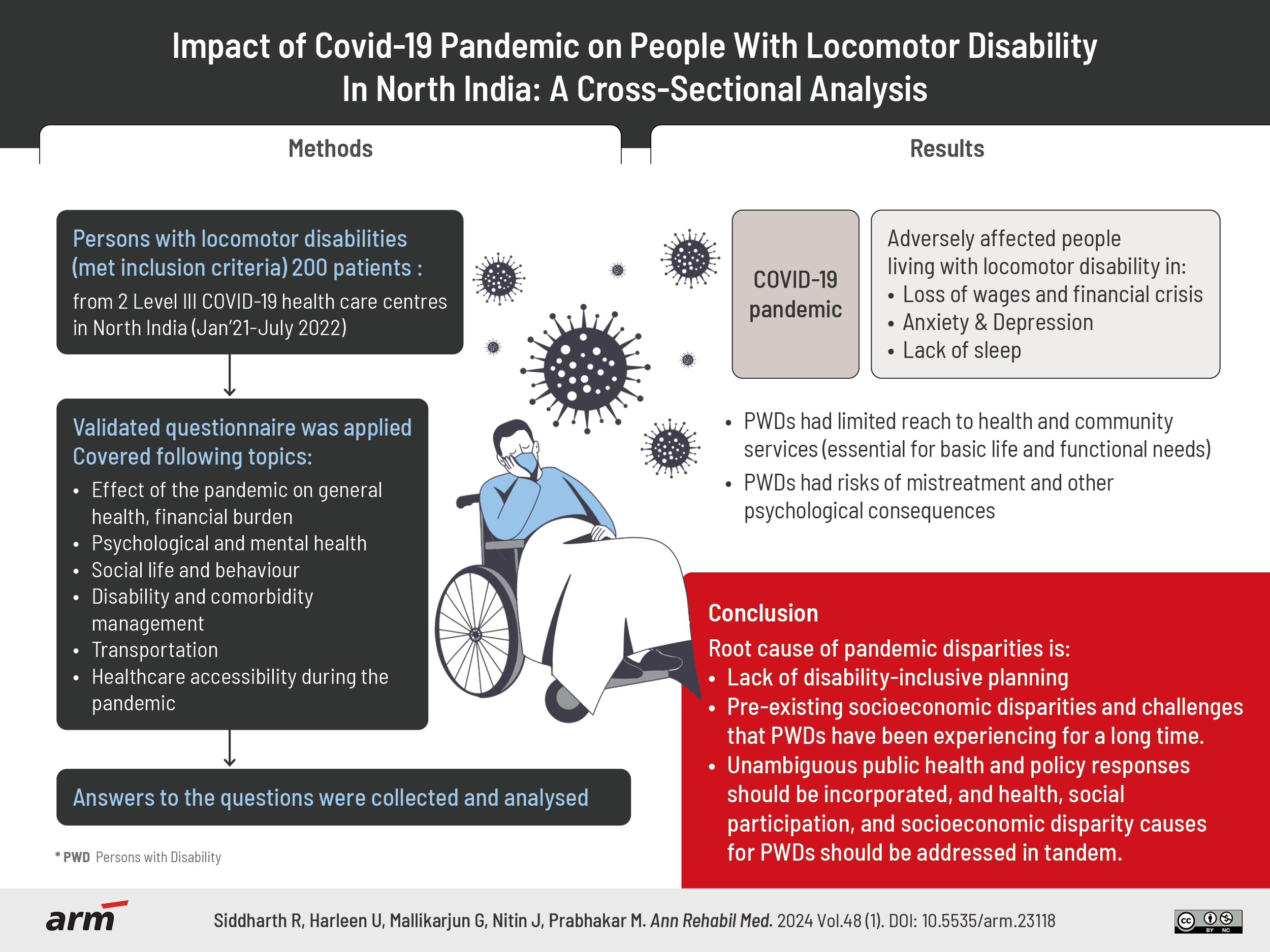
To assess, analyse, and infer the impact of the coronavirus disease 2019 (COVID-19) pandemic on people living with locomotor disability in North India.
Methods
Patients with locomotor disabilities who met the inclusion criteria received a questionnaire that had already undergone testing and validation. It covered topics highlighting the effect of the pandemic on general health, financial burden, psychological and mental health, social life and behaviour, disability and comorbidity management, transportation, and healthcare accessibility during the pandemic. In order to gauge the pandemic’s effects on the population of people with locomotor disabilities, the answers to the questions were collected and analyzed.
Results
The COVID-19 pandemic has adversely affected people living with locomotor disability, ranging from loss of wages and financial crisis to anxiety, depression and lack of sleep. People with disabilities had limited reach to health and community services that were vital for them, including basic life and functional needs, besides risks of mistreatment and other psychological consequences.
Conclusion
This analysis suggests that the root cause of pandemic disparities is the lack of disability-inclusive planning and, more significantly, the pre-existing socioeconomic disparities and challenges that disabled people have been experiencing for a long time. We suggest that unambiguous public health and policy responses should be incorporated, and health, social participation, and socioeconomic disparity causes for disabled people should be addressed in tandem.
Keyword
Figure
Reference
-
1. World Health Organization (WHO). Disabilities [Internet]. WHO [2023 December 20]. Available from: https://www.afro.who.int/health-topics/disabilities.2. World Health Organization (WHO). Disability and health [Internet]. WHO; 2018 [2023 December 20]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/disability-and-health.3. The World Bank; World Health Organization. World report on disability. The World Bank;World Health Organization;2011. p. 8–9.4. Gunjiganvi M, Rai S, Awale R, Mishra P, Gupta D, Gurjar M. Efficacy of Yoga Nidra on depression, anxiety, and insomnia in frontline COVID-19 healthcare workers: a pilot randomized controlled trial. Int J Yoga Therap. 2023; 33:Article 3.5. Mactaggart I, Kuper H, Murthy GV, Sagar J, Oye J, Polack S. Assessing health and rehabilitation needs of people with disabilities in Cameroon and India. Disabil Rehabil. 2016; 38:1757–64.6. Ministry of Statistics and Programme Implementation. Disabled persons in India: a statistical profile 2016. Social Statistics Division, Ministry of Statistics and Programme Implementation, Government of India;2016. p. 36–40.7. Lund EM, Forber-Pratt AJ, Wilson C, Mona LR. The COVID-19 pandemic, stress, and trauma in the disability community: a call to action. Rehabil Psychol. 2020; 65:313–22.8. Registrar General of India. Data on disabled population 2001 and 2011. Ministry of Home Affairs, Government of India;2016. p. 30–8.9. Boyle CA, Fox MH, Havercamp SM, Zubler J. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. 2020; 13:100943.10. Krahn GL, Walker DK, Correa-De-Araujo R. Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015; 105(Suppl 2):S198–206.11. O’Connell CM, Eriks-Hoogland I, Middleton JW. Now, more than ever, our community is needed: spinal cord injury care during a global pandemic. Spinal Cord Ser Cases. 2020; 6:18.12. Drum CE, Oberg A, Cooper K, Carlin R. COVID-19 & adults with disabilities: health and health care access online survey summary report [Internet]. American Association on Health and Disability; 2020 [2023 December 20]. Available from: https://www.aahd.us/wp-content/uploads/2020/05/COVID-19_Summary_Report.pdf.13. Emerson E, Stancliffe R, Hatton C, Llewellyn G, King T, Totsika V, et al. The impact of disability on employment and financial security following the outbreak of the 2020 COVID-19 pandemic in the UK. J Public Health (Oxf). 2021; 43:472–8.14. Jesus TS, Bhattacharjya S, Papadimitriou C, Bogdanova Y, Bentley J, Arango-Lasprilla JC, The Refugee Empowerment Task Force International Networking Group of the American Congress of Rehabilitation Medicine, et al. Lockdown-related disparities experienced by people with disabilities during the first wave of the COVID-19 pandemic: scoping review with thematic analysis. Int J Environ Res Public Health. 2021; 18:6178.15. Cochran AL. Impacts of COVID-19 on access to transportation for people with disabilities. Transp Res Interdiscip Perspect. 2020; 8:100263.16. Jesus TS, Landry MD, Jacobs K. A ‘new normal’ following COVID-19 and the economic crisis: using systems thinking to identify challenges and opportunities in disability, telework, and rehabilitation. Work. 2020; 67:37–46.17. Banks LM, Davey C, Shakespeare T, Kuper H. Disability-inclusive responses to COVID-19: lessons learnt from research on social protection in low- and middle-income countries. World Dev. 2021; 137:105178.18. Farrell TW, Ferrante LE, Brown T, Francis L, Widera E, Rhodes R, et al. AGS position statement: resource allocation strategies and age-related considerations in the COVID-19 era and beyond. J Am Geriatr Soc. 2020; 68:1136–42.19. Goodman-Casanova JM, Dura-Perez E, Guzman-Parra J, Cuesta-Vargas A, Mayoral-Cleries F. Telehealth home support during COVID-19 confinement for community-dwelling older adults with mild cognitive impairment or mild dementia: survey study. J Med Internet Res. 2020; 22:e19434.20. Pettinicchio D, Maroto M, Chai L, Lukk M. Findings from an online survey on the mental health effects of COVID-19 on Canadians with disabilities and chronic health conditions. Disabil Health J. 2021; 14:101085.21. Cheung G, Peri K. Challenges to dementia care during COVID-19: innovations in remote delivery of group Cognitive Stimulation Therapy. Aging Ment Health. 2021; 25:977–9.22. Azarpazhooh MR, Amiri A, Morovatdar N, Steinwender S, Rezaei Ardani A, Yassi N, et al. Correlations between COVID-19 and burden of dementia: an ecological study and review of literature. J Neurol Sci. 2020; 416:117013.23. Porath M. The Mighty survey: 72% say COVID-19 has impacted their healthcare [Internet]. The Mighty; 2020 [2023 December 20]. Available from: https://themighty.com/topic/corona-virus-covid-19/the-mighty-coronavirus-covid-19-survey/.24. Sharpless NE. COVID-19 and cancer. Science. 2020; 368:1290.25. Lim WS, Liang CK, Assantachai P, Auyeung TW, Kang L, Lee WJ, et al. COVID-19 and older people in Asia: Asian Working Group for Sarcopenia calls to actions. Geriatr Gerontol Int. 2020; 20:547–58.26. The New Yorker. Why N.Y.C.’s public housing was unprepared for COVID-19 [Internet]. The New Yorker; 2020 [2023 December 22]. Available from: https://www.youtube.com/watch?v=INrWb-kl5NI.27. McKinney EL, McKinney V, Swartz L. COVID-19, disability and the context of healthcare triage in South Africa: notes in a time of pandemic. Afr J Disabil. 2020; 9:766.28. Lee S, Kim J. A country report: impact of COVID-19 and inequity of health on South Korea’s disabled community during a pandemic. Disabil Soc. 2020; 35:1514–9.29. Banskota S, Healy M, Goldberg EM. 15 smartphone apps for older adults to use while in isolation during the COVID-19 pandemic. West J Emerg Med. 2020; 21:514–25.30. Andrews EE, Forber-Pratt AJ, Mona LR, Lund EM, Pilarski CR, Balter R. #SaytheWord: a disability culture commentary on the erasure of “disability”. Rehabil Psychol. 2019; 64:111–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Why Fast COVID-19 Vaccination Needed for People with Disabilities and Autistics in Korea?
- The coronavirus disease 2019 pandemic and chronic diseases
- COVID-19 and cancer: reflections 2 years into the pandemic
- COVID-19: Weighing the Endeavors of Nations, with Time to Event Analysis
- The Prevalence of Depression, Anxiety and Associated Factors among the General Public during COVID-19 Pandemic: a Cross-sectional Study in Korea