J Korean Med Sci.
2021 Jul;36(29):e214. 10.3346/jkms.2021.36.e214.
The Prevalence of Depression, Anxiety and Associated Factors among the General Public during COVID-19 Pandemic: a Cross-sectional Study in Korea
- KMID: 2518742
- DOI: http://doi.org/10.3346/jkms.2021.36.e214
Abstract
- Background
Since its first case confirmed on January 20, 2020, Korea has been through three waves of the COVID-19 pandemic. Fears of the fourth wave persist as new cases continue to emerge. In such unpredictable times, the mental well-being of people is of crucial importance. This study examined the levels of depression and anxiety and their predictors among the Korean general public in Busan, Korea, during the COVID-19 pandemic.
Methods
We conducted a cross-sectional study via a self-reported questionnaire administered to 2,288 adult residents (aged 19–60 years) of Busan, Korea. Participants' depression and anxiety were assessed using the Korean version of the Patient Health Questionnaire-4 (PHQ-4), which consists of PHQ-2 and Generalized Anxiety Disorder-2 (GAD-2), with the cutoff score of 3.
Results
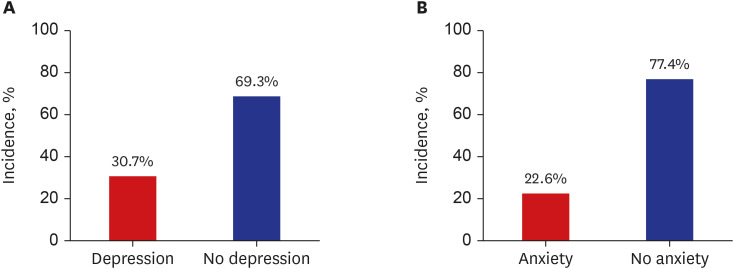
The mean age of the participants was 39.71 years. COVID-19 had several psychosocial impacts on people. It was revealed that 80.3% had restrictions in outside activities, 47.3% reported financial difficulties, and 53.6% had a fear of death or fatal outcome when infected with COVID-19. We performed logistic regression analysis to identify the factors associated with depression and anxiety. A total of 30.7% participants were classified as at risk of depression based on cutoff score of 3 on PHQ-2. Logistic regression analysis revealed that changes in sleep pattern due to COVID-19 were most strongly associated with depression, followed by restrictions in outside activities due to social distancing and increased family conflicts due to COVID-19. Also, 22.6% participants were classified as at risk of anxiety based on a cutoff score of 3 on GAD-2. Analysis revealed that changes in sleep pattern due to COVID-19 were most strongly associated with anxiety, followed by spending a lot of time searching for COVID-19-related information and having a fear of death or fatal outcome when infected with COVID-19.
Conclusion
The results are alarming; 30.7% had a PHQ-2 score of 3 or higher, indicating depression, and 22.6% had a GAD-2 score of 3 or higher, indicating anxiety. Changes in sleep pattern had the strongest association with both depression and anxiety. Our results can be used to formulate mental health policies tailored to the context of the city. Our findings suggest the high prevalence of depression and anxiety in the society during the COVID-19 pandemic, which places growing importance on early intervention for mental health problems during these times.
Keyword
Figure
Reference
-
1. World Health Organization. Coronavirus disease 2019 (COVID-19) situation report-51. Updated 2020. Accessed March 7, 2021. https://apps.who.int/iris/handle/10665/331475.2. Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020; 96(1137):399–402. PMID: 32366457.
Article3. Lee HS, Dean D, Baxter T, Griffith T, Park S. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. 2021; 295:113570. PMID: 33234326.
Article4. Korea Centers for Disease Control and Prevention. Updated 2021. Accessed March 15, 2021. http://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=712573&cg_code=&act=view&nPage=15.5. Jalloh MF, Li W, Bunnell RE, Ethier KA, O'Leary A, Hageman KM, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018; 3(2):e000471.
Article6. Lau JT, Yang X, Pang E, Tsui HY, Wong E, Wing YK. SARS-related perceptions in Hong Kong. Emerg Infect Dis. 2005; 11(3):417–424. PMID: 15757557.7. Yu BY, Yeung WF, Lam JC, Yuen SC, Lam SC, Chung VC, et al. Prevalence of sleep disturbances during COVID-19 outbreak in an urban Chinese population: a cross-sectional study. Sleep Med. 2020; 74:18–24. PMID: 32836181.
Article8. Busan Metropolitan Government. Updated 2021. Accessed March 15, 2021. https://www.busan.go.kr/covid19/Status02.do.9. Korea Centers for Disease Control and Prevention. Updated 2020. Accessed March 16, 2021. http://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015&list_no=368260&cg_code=&act=view&nPage=65.10. Kim HW, Shin C, Lee SH, Han C. Standardization of the Korean version of the Patient Health Questionnaire-4 (PHQ-4). Clin Psychopharmacol Neurosci. 2021; 19(1):104–111. PMID: 33508793.
Article11. Manea L, Gilbody S, Hewitt C, North A, Plummer F, Richardson R, et al. Identifying depression with the PHQ-2: a diagnostic meta-analysis. J Affect Disord. 2016; 203:382–395. PMID: 27371907.
Article12. Plummer F, Manea L, Trepel D, McMillan D. Screening for anxiety disorders with the GAD-7 and GAD-2: a systematic review and diagnostic metaanalysis. Gen Hosp Psychiatry. 2016; 39:24–31. PMID: 26719105.
Article13. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009; 50(6):613–621. PMID: 19996233.
Article14. Löwe B, Wahl I, Rose M, Spitzer C, Glaesmer H, Wingenfeld K, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. 2010; 122(1-2):86–95. PMID: 19616305.
Article15. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003; 41(11):1284–1292. PMID: 14583691.16. Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007; 146(5):317–325. PMID: 17339617.
Article17. Shin C, Kim Y, Park S, Yoon S, Ko YH, Kim YK, et al. Prevalence and associated factors of depression in general population of Korea: results from the Korea National Health and Nutrition Examination Survey, 2014. J Korean Med Sci. 2017; 32(11):1861–1869. PMID: 28960042.
Article18. Christensen H, Batterham PJ, Grant JB, Griffiths KM, Mackinnon AJ. A population study comparing screening performance of prototypes for depression and anxiety with standard scales. BMC Med Res Methodol. 2011; 11(1):154. PMID: 22103584.
Article19. Yu X, Stewart SM, Wong PT, Lam TH. Screening for depression with the Patient Health Questionnaire-2 (PHQ-2) among the general population in Hong Kong. J Affect Disord. 2011; 134(1-3):444–447. PMID: 21665288.
Article20. Choi EP, Hui BP, Wan EY. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health. 2020; 17(10):E3740. PMID: 32466251.
Article21. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). 5th ed. Washington, D.C., USA: American Psychiatric Association;2013.22. Lee YR, Lee JY, Park IH, Kim M, Jhon M, Kim JW, et al. The Relationships among media usage regarding COVID-19, knowledge about infection, and anxiety: structural model analysis. J Korean Med Sci. 2020; 35(48):e426. PMID: 33316862.
Article23. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. 2020; 17(5):E1729. PMID: 32155789.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mental Health of Physical Therapy Students in Clinical Practice during the COVID-19 Pandemic: A Cross-sectional Survey in Gwangju and Jeollanam-do, South Korea
- Association Between the Need for Mental Health Intervention and Mental Health Problems Among the General Population During the COVID-19 Pandemic
- Factors Associated With Depression and Anxiety in Korean Adolescents During the COVID-19 Pandemic
- Impact of the COVID-19 pandemic on depression during pregnancy: a cross-sectional study
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis