J Korean Foot Ankle Soc.
2023 Dec;27(4):148-153. 10.14193/jkfas.2023.27.4.148.
Bony Union of Osteochondral Lesion of the Talus after Bone Marrow Aspirate Concentrate and Matrix-Induced Chondrogenesis: A Case Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- KMID: 2553008
- DOI: http://doi.org/10.14193/jkfas.2023.27.4.148
Abstract
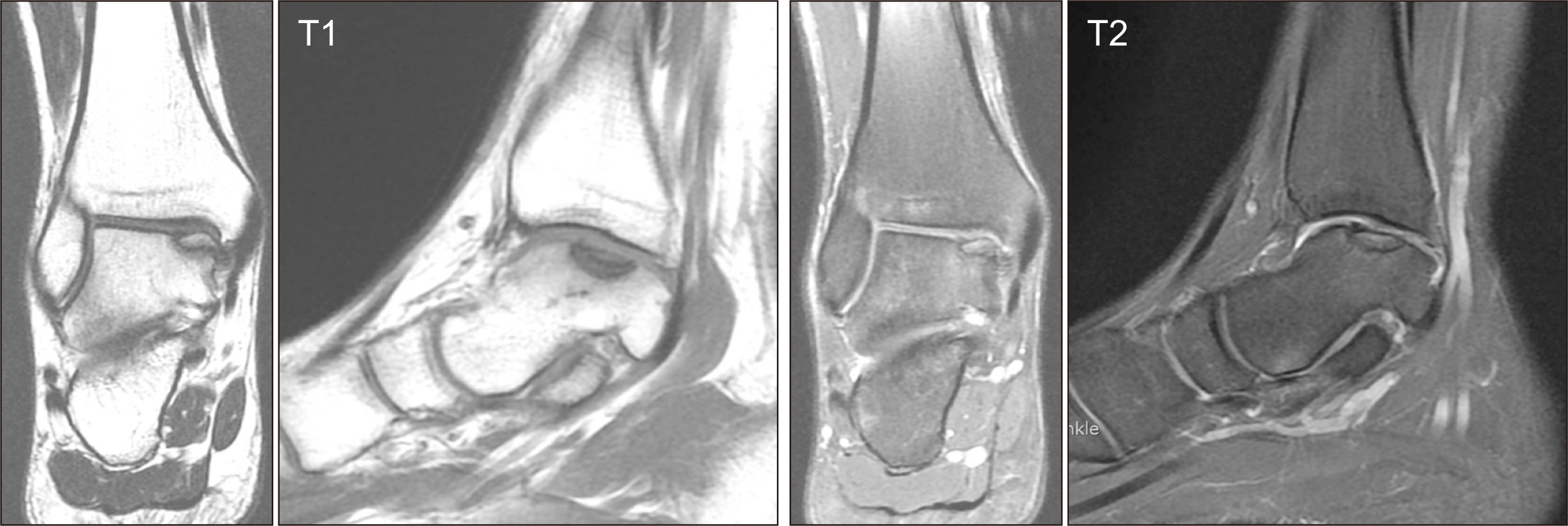
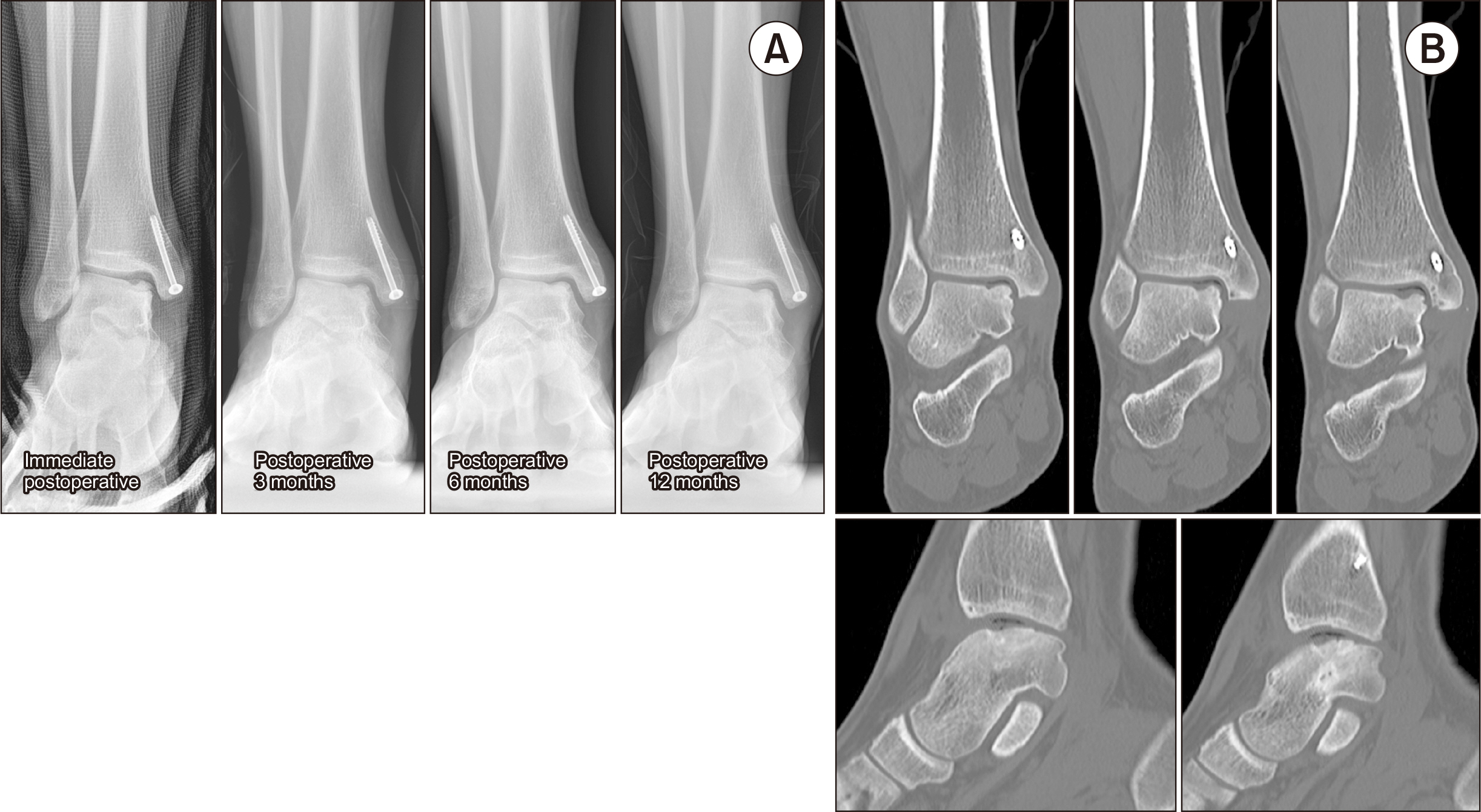
- Traditionally, arthroscopic microfracture and autologous osteochondral autograft transplantation have been the primary surgical treatments for osteochondral lesions of the talus. On the other hand, recent advancements have introduced alternative approaches, such as autologous chondrocyte transplantation, matrix-derived autologous chondrocyte transplantation, intra-articular injection of concentrated bone marrow aspirate concentrate, and the use of fibrin glue to address chondral defects. Furthermore, some studies have explored a combination of bone marrow aspirate and matrix-derived chondrogenesis. In light of these developments, this report presents a case study of a young male patient in his early twenties with a relatively large osteochondral lesion exceeding 1.5 cm 2 on the medial talar dome. Instead of removing the osteochondral lesion, a surgical approach was employed to retain the lesion while addressing the unstable cartilage in the affected area. This approach involved a combination of bone marrow aspirate concentrate and matrix-derived chondrogenesis. The treatment yielded favorable clinical outcomes and ultimately successfully induced the bony union of osteochondral lesions. This paper reports the author’s experience with this innovative approach with a review of the relevant literature.
Keyword
Figure
Reference
-
References
1. Choi WJ, Park KK, Kim BS, Lee JW. 2009; Osteochondral lesion of the talus: is there a critical defect size for poor outcome? Am J Sports Med. 37:1974–80. doi: 10.1177/0363546509335765. DOI: 10.1177/0363546509335765. PMID: 19654429.2. Benthien JP, Behrens P. 2010; Autologous matrix-induced chondrogenesis (AMIC): combining microfracturing and a collagen I/III matrix for articular cartilage resurfacing. Cartilage. 1:65–8. doi: 10.1177/1947603509360044. DOI: 10.1177/1947603509360044. PMID: 26069536. PMCID: PMC4440611.3. Kim BS, Na Y, Kwon WH. 2020; Operative treatment for osteochondral lesions of the talus: bone marrow aspirate concentrate and matrix-induced chondrogenesis. J Korean Foot Ankle Soc. 24:61–8. doi: 10.14193/jkfas.2020.24.2.61. DOI: 10.14193/jkfas.2020.24.2.61.
Article4. Corr D, Raikin J, O'Neil J, Raikin S. 2021; Long-term outcomes of microfracture for treatment of osteochondral lesions of the talus. Foot Ankle Int. 42:833–40. doi: 10.1177/1071100721995427. DOI: 10.1177/1071100721995427. PMID: 33719632. PMCID: PMC8772008.
Article5. Madry H, Gao L, Eichler H, Orth P, Cucchiarini M. 2017; Bone marrow aspirate concentrate-enhanced marrow stimulation of chondral defects. Stem Cells Int. 2017:1609685. doi: 10.1155/2017/1609685. DOI: 10.1155/2017/1609685. PMID: 28607559. PMCID: PMC5451778.
Article6. Murphy EP, McGoldrick NP, Curtin M, Kearns SR. 2019; A prospective evaluation of bone marrow aspirate concentrate and microfracture in the treatment of osteochondral lesions of the talus. Foot Ankle Surg. 25:441–8. doi: 10.1016/j.fas.2018.02.011. DOI: 10.1016/j.fas.2018.02.011. PMID: 30321966.
Article7. Volz M, Schaumburger J, Frick H, Grifka J, Anders S. 2017; A randomized controlled trial demonstrating sustained benefit of Autologous Matrix-Induced Chondrogenesis over microfracture at five years. Int Orthop. 41:797–804. doi: 10.1007/s00264-016-3391-0. DOI: 10.1007/s00264-016-3391-0. PMID: 28108777.
Article8. Vannini F, Cavallo M, Ramponi L, Castagnini F, Massimi S, Giannini S, et al. 2017; Return to sports after bone marrow-derived cell transplantation for osteochondral lesions of the talus. Cartilage. 8:80–7. doi: 10.1177/1947603516642574. DOI: 10.1177/1947603516642574. PMID: 27994723. PMCID: PMC5154421.
Article9. Richter M, Zech S. 2019; Matrix-associated stem cell transplantation (MAST) in chondral lesions at the ankle as part of a complex surgical approach- 5-year-follow-up in 100 patients. Foot Ankle Surg. 25:264–71. doi: 10.1016/j.fas.2017.11.004. DOI: 10.1016/j.fas.2017.11.004. PMID: 29409182.
Article10. Sadineni RT, Pasumarthy A, Bellapa NC, Velicheti S. 2015; Imaging patterns in MRI in recent bone injuries following negative or inconclusive plain radiographs. J Clin Diagn Res. 9:TC10–3. doi: 10.7860/JCDR/2015/15451.6685. DOI: 10.7860/JCDR/2015/15451.6685. PMID: 26557590. PMCID: PMC4625309.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Operative Treatment for Osteochondral Lesions of the Talus: Bone Marrow Aspirate Concentrate and Matrix-induced Chondrogenesis
- Corrigendum: Operative Treatment for Osteochondral Lesions of the Talus: Bone Marrow Aspirate Concentrate and Matrix-induced Chondrogenesis
- Osteochondral Lesion of the Talus in Children and Adolescents
- Supramalleolar Osteotomy Combined with Redo Arthroscopy for a Patient with Persistent Pain after Primary Arthroscopic Microfracture for Medial Osteochondral Lesion of the Talus: A Case Report
- Simultaneously Occurred Medial and Lateral Osteochondral Lesions of the Talus