Ann Lab Med.
2023 Jan;43(1):29-37. 10.3343/alm.2023.43.1.29.
Intuitive Modification of the Friedewald Formula for Calculation of LDL-Cholesterol
- Affiliations
-
- 1Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine, Hallym University Chuncheon Sacred Heart Hospital, Chuncheon, Korea
- 3University of Ulsan College of Medicine, Seoul, Korea
- 4Department of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2551577
- DOI: http://doi.org/10.3343/alm.2023.43.1.29
Abstract
- Background
High LDL-cholesterol (LDL-C) is an established risk factor for cardiovascular disease and is considered an important therapeutic target. It can be measured directly or calculated from the results of other lipid tests. The Friedewald formula is the most widely used formula for calculating LDL-C. We modified the Friedewald formula for a more accurate and practical estimation of LDL-C.
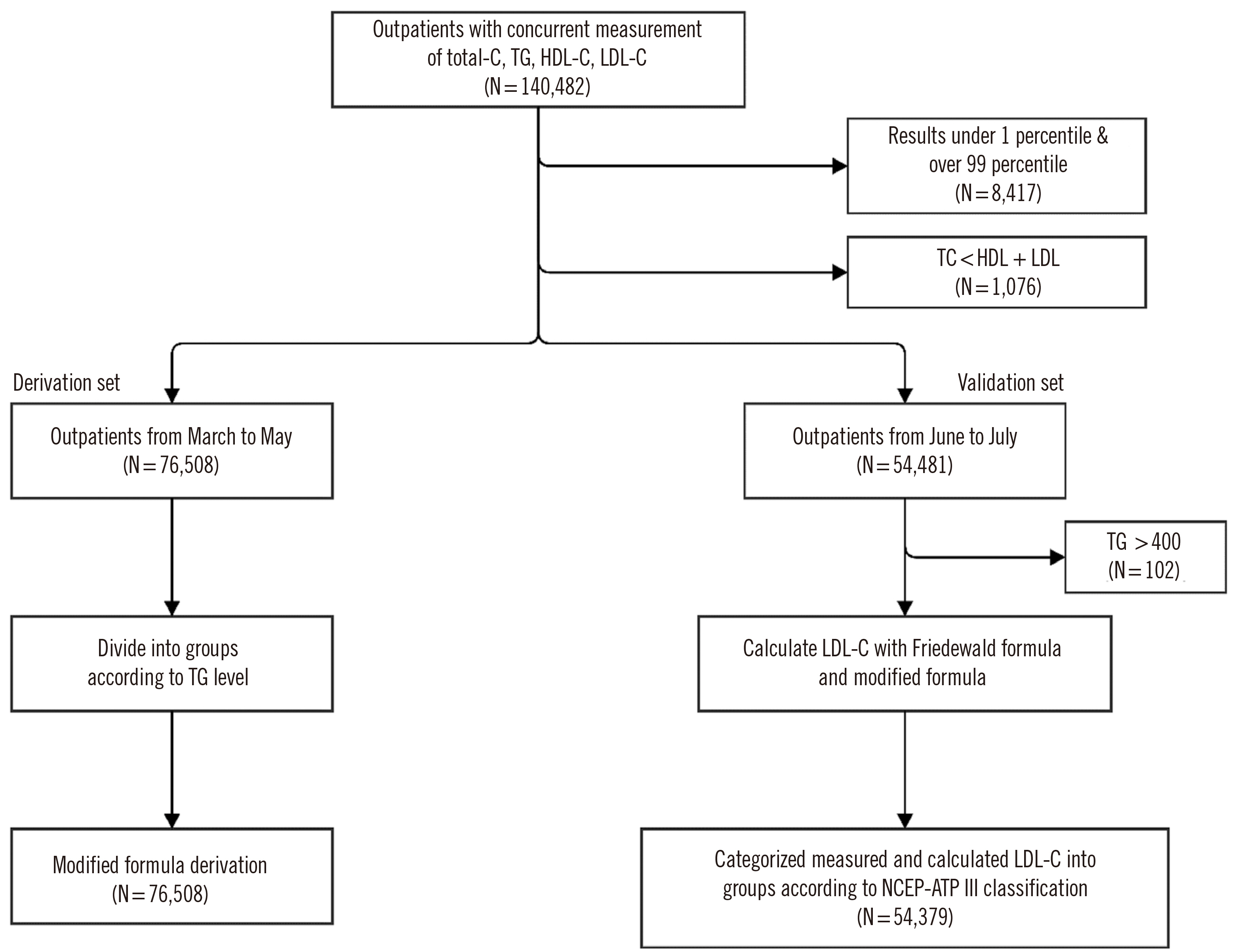
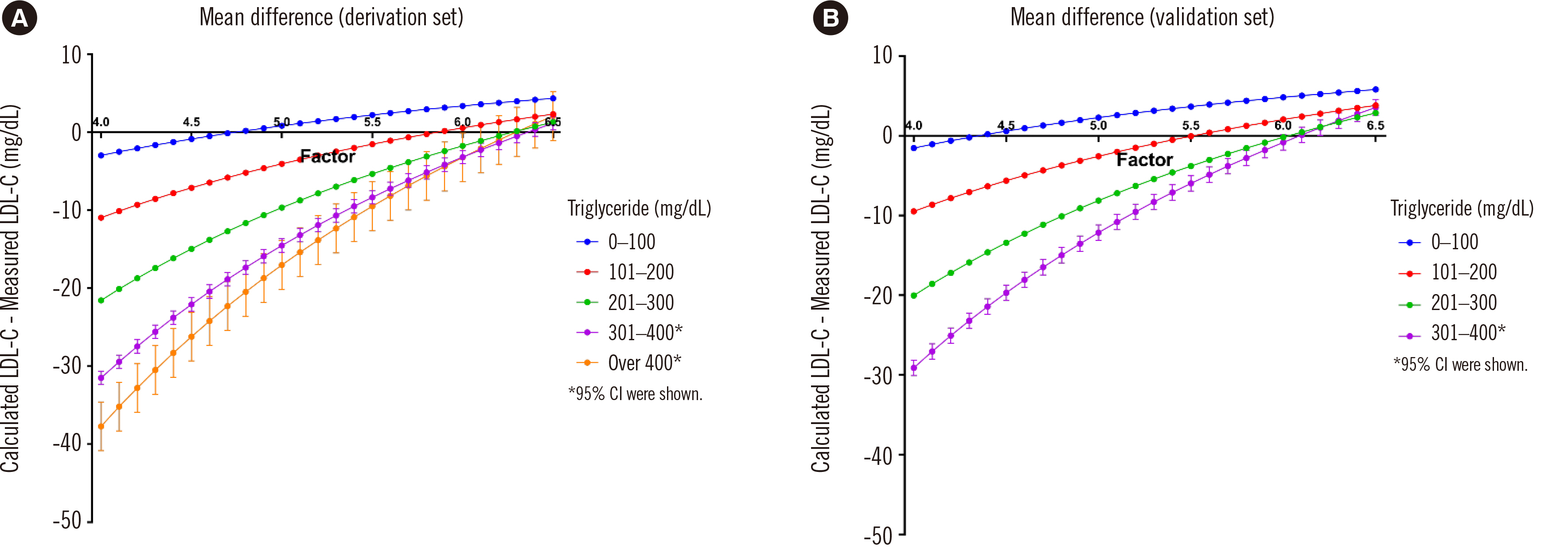
Methods
Datasets, including measured triglyceride, total cholesterol, HDL-cholesterol, and LDL-C concentrations were collected and assigned to derivation and validation sets. The datasets were further divided into five groups based on triglyceride concentrations. In the modified formula, LDL-C was defined as total cholesterol − HDL-cholesterol − (triglyceride/adjustment factor). For each group, the adjustment factor that minimized the difference between measured LDL-C and calculated LDL-C using modified formula was obtained. For validation, measured LDL-C and LDL-C calculated using the modified formula (LDL-CM), Friedewald formula (LDL-CF), Martin-Hopkins formula (LDL-CMa), and Sampson formula (LDL-CS) were compared.
Results
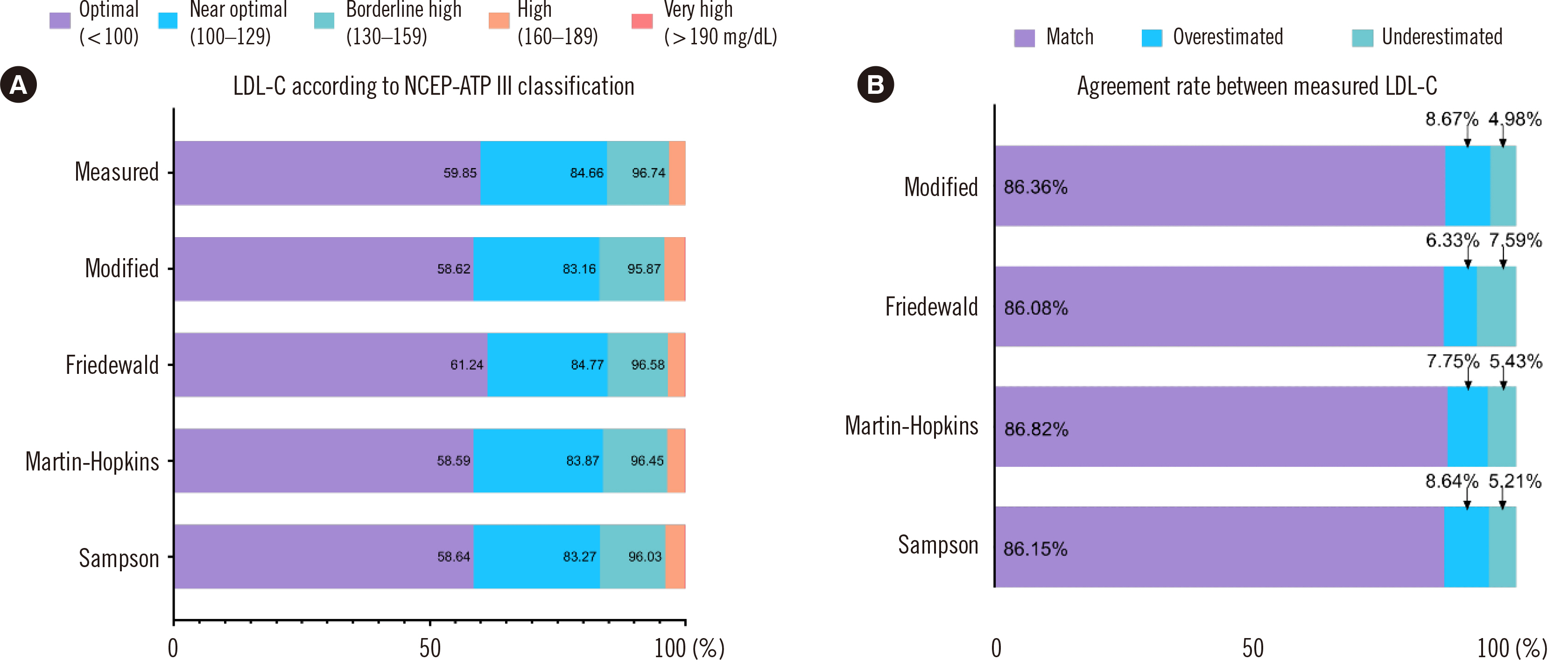
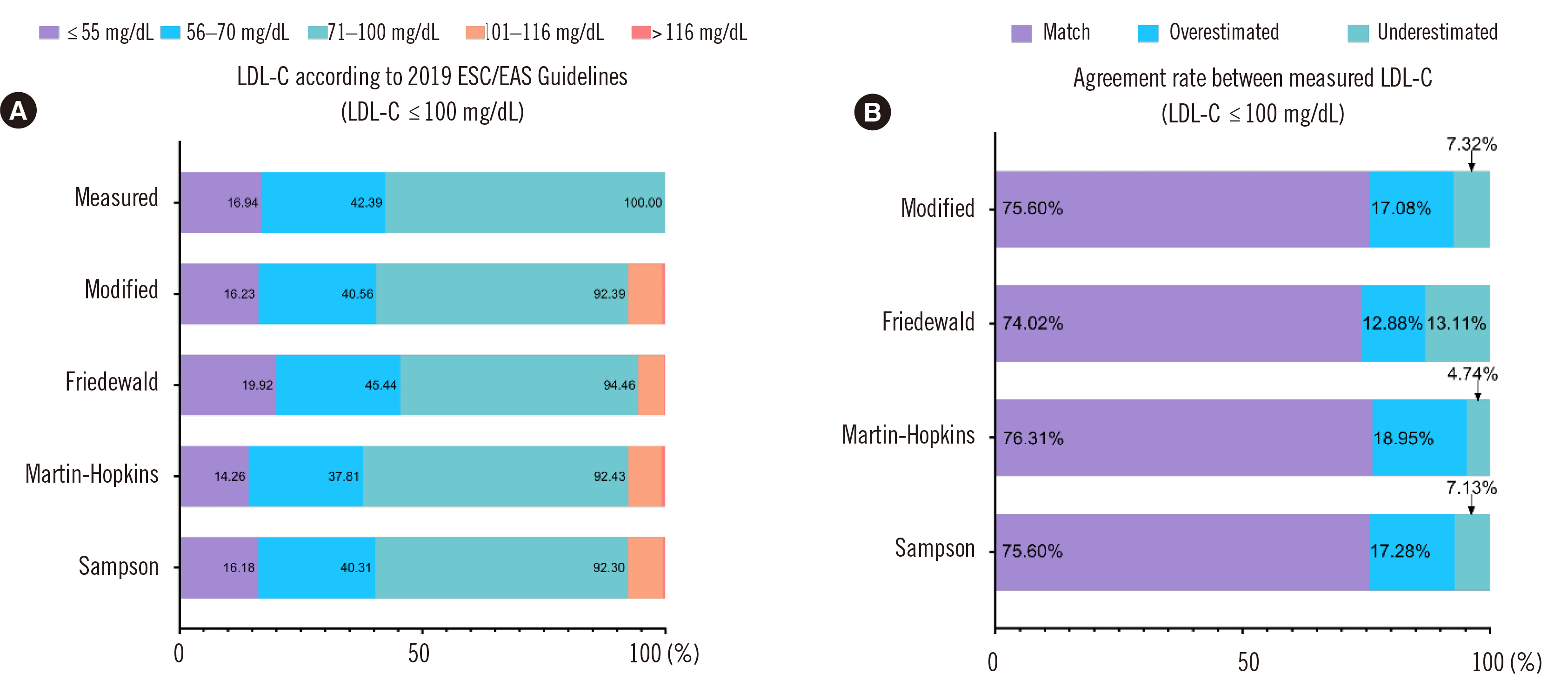
In the derivation set, the adjustment factors were 4.7, 5.9, 6.3, and 6.4 for the groups with triglyceride concentrations <100, 101–200, 201–300, and >300 mg/dL, respectively. In the validation set, the coefficient of determination (R2) between measured and calculated LDL-C was higher for LDL-CM than for LDL-CF (R2=0.9330 vs. 0.9206). The agreement according to the National Cholesterol Education Program Adult Treatment Panel III classification of LDL-C was 86.36%, 86.08%, 86.82%, and 86.15% for LDL-CM, LDL-CF, LDL-CMa, and LDL-CS, respectively.
Conclusions
We proposed a practical, improved LDL-C calculation formula by applying different factors depending on the triglyceride concentration.
Figure
Cited by 1 articles
-
Associations of LDL Cholesterol, Non-HDL Cholesterol, and Apolipoprotein B With Cardiovascular Disease Occurrence in Adults: Korean Genome and Epidemiology Study
Shin Young Yun, John Hoon Rim, Hyein Kang, Sang-Guk Lee, Jong-Baeck Lim
Ann Lab Med. 2023;43(3):237-243. doi: 10.3343/alm.2023.43.3.237.
Reference
-
1. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2019; 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 139:e1082–143. DOI: 10.1161/CIR.0000000000000624. PMID: 30586774. PMCID: PMC7403606.2. Yang HS, Hur M, Kim H, Kim SJ, Shin S, Somma SD, et al. 2020; HDL Subclass Analysis in Predicting Metabolic Syndrome in Koreans With High HDL Cholesterol Levels. Ann Lab Med. 40:297–305. DOI: 10.3343/alm.2020.40.4.297. PMID: 32067428. PMCID: PMC7054694.
Article3. Yang HS, Jeong HJ, Kim H, Hwang HK, Hur M, Lee S. 2022; Sex-Specific U-Shaped Relationships Between High-Density Lipoprotein Cholesterol Levels and 10-year Major Adverse Cardiovascular Events: A Nationwide Cohort Study of 5.7 Million South Koreans. Ann Lab Med. 42:415–27. DOI: 10.3343/alm.2022.42.4.415. PMID: 35177562. PMCID: PMC8859558.
Article4. Berliner JA, Navab M, Fogelman AM, Frank JS, Demer LL, Edwards PA, et al. 1995; Atherosclerosis: basic mechanisms. Oxidation, inflammation, and genetics. Circulation. 91:2488–96. DOI: 10.1161/01.CIR.91.9.2488. PMID: 7729036.5. Navab M, Fogelman AM, Berliner JA, Territo MC, Demer LL, Frank JS, et al. 1995; Pathogenesis of atherosclerosis. Am J Cardiol. 76:18C–23C. DOI: 10.1016/S0002-9149(99)80466-4. PMID: 7572682.
Article6. Cholesterol Treatment Trialists' (CTT) Collaboration. 2010; Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 376:1670–81. DOI: 10.1016/S0140-6736(10)61350-5. PMID: 21067804. PMCID: PMC2988224.7. Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, et al. 2012; Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 60:2631–9. DOI: 10.1016/j.jacc.2012.09.017. PMID: 23083789.8. Ference BA, Ginsberg HN, Graham I, Ray KK, Packard CJ, Bruckert E, et al. 2017; Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 38:2459–72. DOI: 10.1093/eurheartj/ehx144. PMID: 28444290. PMCID: PMC5837225.
Article9. Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, et al. 2005; Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 366:1267–78. DOI: 10.1016/S0140-6736(05)67394-1. PMID: 16214597.
Article10. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2020; ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 41:111–88. DOI: 10.1093/eurheartj/ehz455. PMID: 31504418.11. Rifai N, Warnick GR, Dominiczak MH. 2001. Handbook of Lipoprotein Testing. 2nd ed. AACC Press;Washington:12. Nauck M, Warnick GR, Rifai N. 2002; Methods for measurement of LDL-cholesterol: a Critical assessment of direct measurement by homogeneous assays versus calculation. Clin Chem. 48:236–54. DOI: 10.1093/clinchem/48.2.236. PMID: 11805004.
Article13. Türkalp I, Cil Z, Ozkazanç D. 2005; Analytical performance of a direct assay for LDL-cholesterol: a comparative assessment versus Friedewald's formula. Anadolu Kardiyol Derg. 5:13–7. PMID: 15755695.14. Miller WG, Myers GL, Sakurabayashi I, Bachmann LM, Caudill SP, Dziekonski A, et al. 2010; Seven direct methods for measuring HDL and LDL cholesterol compared with ultracentrifugation reference measurement procedures. Clin Chem. 56:977–86. DOI: 10.1373/clinchem.2009.142810. PMID: 20378768. PMCID: PMC4687457.
Article15. Vesper HW. 2018. Educational Discussion: Lipids, 2018 Accuracy-Based Lipids (ABL). https://documents.cap.org/documents/2018-lipid-b.pdf.16. Friedewald WT, Levy RI, Fredrickson DS. 1972; Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 18:499–502. DOI: 10.1093/clinchem/18.6.499. PMID: 4337382.
Article17. Anandaraja S, Narang R, Godeswar R, Laksmy R, Talwar KK. 2005; Low-density lipoprotein cholesterol estimation by a new formula in Indian population. Int J Cardiol. 102:117–20. DOI: 10.1016/j.ijcard.2004.05.009. PMID: 15939107.
Article18. Hattori Y, Suzuki M, Tsushima M, Yoshida M, Tokunaga Y, Wang Y, et al. 1998; Development of approximate formula for LDL-chol, LDL-apo B and LDL-chol/LDL-apo B as indices of hyperapobetalipoproteinemia and small dense LDL. Atherosclerosis. 138:289–99. DOI: 10.1016/S0021-9150(98)00034-3. PMID: 9690912.
Article19. Puavilai W, Laorugpongse D, Deerochanawong C, Muthapongthavorn N, Srilert P. 2009; The accuracy in using modified Friedewald equation to calculate LDL from non-fast triglyceride: a pilot study. J Med Assoc Thai. 92:182–7. PMID: 19253792.20. Hata Y, Nakajima K. 1986; Application of Friedewald's LDL-cholesterol estimation formula to serum lipids in the Japanese population. Jpn Circ J. 50:1191–200. DOI: 10.1253/jcj.50.1191. PMID: 3469420.
Article21. Martin SS, Blaha MJ, Elshazly MB, Toth PP, Kwiterovich PO, Blumenthal RS, et al. 2013; Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA. 310:2061–8. DOI: 10.1001/jama.2013.280532. PMID: 24240933. PMCID: PMC4226221.
Article22. Sampson M, Ling C, Sun Q, Harb R, Ashmaig M, Warnick R, et al. 2020; A new equation for calculation of low-density lipoprotein cholesterol in patients with normolipidemia and/or hypertriglyceridemia. JAMA Cardiol. 5:540–8. DOI: 10.1001/jamacardio.2020.0013. PMID: 32101259. PMCID: PMC7240357.
Article23. Arranz-Peña ML, Tasende-Mata J, Martin-Gil FJ. 1998; Comparison of two homogeneous assays with a precipitation method and an ultracentrifugation method for the measurement of HDL-cholesterol. Clin Chem. 44:2499–505. DOI: 10.1093/clinchem/44.12.2499. PMID: 9836717.
Article24. Iwasaki Y, Matsuyama H, Nakashima N. 2006; Improved specificity of a new homogeneous assay for LDL-cholesterol in serum with abnormal lipoproteins. Clin Chem. 52:886–8. DOI: 10.1373/clinchem.2005.053983. PMID: 16556687.
Article25. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. 2001; Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA. 285:2486–97. DOI: 10.1001/jama.285.19.2486. PMID: 11368702.26. Martin SS, Blaha MJ, Elshazly MB, Brinton EA, Toth PP, McEvoy JW, et al. 2013; Friedewald-estimated versus directly measured low-density lipoprotein cholesterol and treatment implications. J Am Coll Cardiol. 62:732–9. DOI: 10.1016/j.jacc.2013.01.079. PMID: 23524048.
Article27. Myers GL, Kimberly MM, Waymack PP, Smith SJ, Cooper GR, Sampson EJ. 2000; A reference method laboratory network for cholesterol: a model for standardization and improvement of clinical laboratory measurements. Clin Chem. 46:1762–72. DOI: 10.1093/clinchem/46.11.1762. PMID: 11067811.
Article28. Beckman Coulter. LDL-cholesterol calibrator Instructions for Use BLODC0012.04. 2016. DOI: 10.1093/clinchem/46.11.1762.29. Rossouw HM, Nagel SE, Pillay TS. 2021; Comparability of 11 different equations for estimating LDL cholesterol on different analysers. Clin Chem Lab Med. 59:1930–43. DOI: 10.1515/cclm-2021-0747. PMID: 34384146.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting the Difference between the Low-Density Lipoprotein Cholesterol Concentrations Measured Directly and Calculated Using the Friedewald Formula
- Analysis of Low-Density Lipoprotein Cholesterol by Homogenous Assay in Comparison with Friedewald Formula
- Comparison of Formulas for Calculating Low-density Lipoprotein Cholesterol in General Population and High-risk Patients with Cardiovascular Disease
- Validation of the Friedewald formula for estimating low density lipoprotein cholesterol: the Korea National Health and Nutrition Examination Survey, 2009 to 2011
- Martin's Equation as the Most Suitable Method for Estimation of Low-Density Lipoprotein Cholesterol Levels in Korean Adults