J Stroke.
2024 Jan;26(1):95-103. 10.5853/jos.2023.02292.
Thrombectomy in Stroke Patients With Low Alberta Stroke Program Early Computed Tomography Score: Is Modified Thrombolysis in Cerebral Infarction (mTICI) 2c/3 Superior to mTICI 2b?
- Affiliations
-
- 1Department of Neurosurgery, Division of Neuroendovascular Surgery, Medical University of South Carolina, Charleston, SC, USA
- 2Department of Neurosurgery, Hyogo Medical University, Nishinomiya, Japan
- 3Department of Neurology, University Medical Center Göttingen, Göttingen, Germany
- 4Department of Neurosurgery, Thomas Jefferson University Hospitals, Philadelphia, PA, USA
- 5Department of Neurology, Chonnam National University Medical School, Chonnam National University Hospital, Gwangju, Korea
- 6Department of Neurosurgery, Wake Forest School of Medicine, Winston-Salem, NC, USA
- 7Department of Radiology, West Virginia School of Medicine, Morgantown, WV, USA
- 8Department of Neurosurgery, University of Miami Health System, Miami, FL, USA
- 9Department of Interventional and Diagnostical Neuroradiology, University of Basel, Basel, Switzerland
- 10Department of Neurology, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
- 11Department of Neurology, University of Iowa Hospitals and Clinics, Iowa City, IA, USA
- 12Department of Neurosurgery and Neurointerventional Radiology, Louisiana State University, Shreveport, LA, USA
- 13Department of Neurosurgery, Radiology and Imaging Sciences, Emory University, Atlanta, GA, USA
- 14Department of Neuroradiology, University Hospital San Giovanni di Dio e Ruggi d’Aragona, University of Salerno, Salerno, Italy
- 15Department of Neurosurgery, Baylor College of Medicine, Houston, TX, USA
- 16Department of Neurosurgery, University of Texas Health Science Center at San Antonio, San Antonio, TX, USA
- 17Department of Neuroradiology, Hospital São José Centro Hospitalar, Lisboa, Portugal
- 18Department of Neurosurgery, University of Florida, Gainesville, FL, USA
- 19Department of Neurological Surgery, Washington University, St. Louis, MO, USA
- 20Department of Neurosurgery, Endovascular Neurological Center, Montevideo, Uruguay
- 21Department of Neurosurgery, Yale School of Medicine, New Haven, CT, USA
- 22Department of Neurosurgery, University of Virginia, Charlottesville, VA, USA
- 23Department of Neurosurgery, University of Washington, Seattle, WA, USA
- 24Department of Radiology, Mayo Clinic, Rochester, MN, USA; Department of Neurosurgery, Mayo Clinic, Rochester, MN, USA
- 25Department of Neuroradiology, Washington Regional J.B. Hunt Transport Services Neuroscience Institute, Fayetteville, AZ, USA
- 26Department of Neurosurgery, University of Arizona, Tucson, AZ, USA
- 27Department of Neurosurgery, Allegheny Health Network, Pittsburgh, PA, USA
- 28Department of Neuroradiology, Hospital Universitario La Paz, Madrid, Spain
- 29Department of Neurological Surgery, University of Texas Medical Branch - Galveston, TX, USA
- 30Department of Neurosurgery, Mount Sinai Health System, New York, NY, USA
- 31Department of Neurosurgery, NorthShore University Health System, Evanston, IL, USA
- 32University of Houston, Department of Clinical Neuroscience, HCA Houston Healthcare Kingwood, Houston, TX, USA
- KMID: 2551351
- DOI: http://doi.org/10.5853/jos.2023.02292
Abstract
- Background and Purpose
Outcomes following mechanical thrombectomy (MT) are strongly correlated with successful recanalization, traditionally defined as modified Thrombolysis in Cerebral Infarction (mTICI) ≥2b. This retrospective cohort study aimed to compare the outcomes of patients with low Alberta Stroke Program Early Computed Tomography Score (ASPECTS; 2–5) who achieved mTICI 2b versus those who achieved mTICI 2c/3 after MT.
Methods
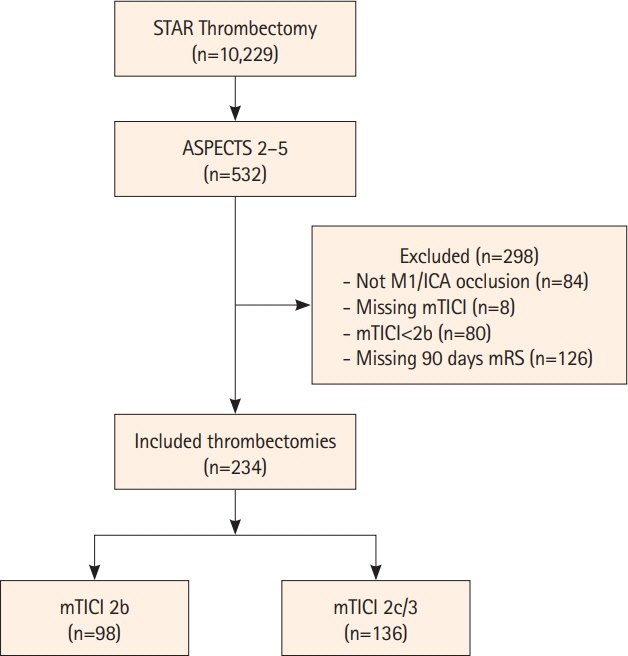
This study utilized data from the Stroke Thrombectomy and Aneurysm Registry (STAR), which combined databases from 32 thrombectomy-capable stroke centers between 2013 and 2023. The study included only patients with low ASPECTS who achieved mTICI 2b, 2c, or 3 after MT for internal carotid artery or middle cerebral artery (M1) stroke.
Results
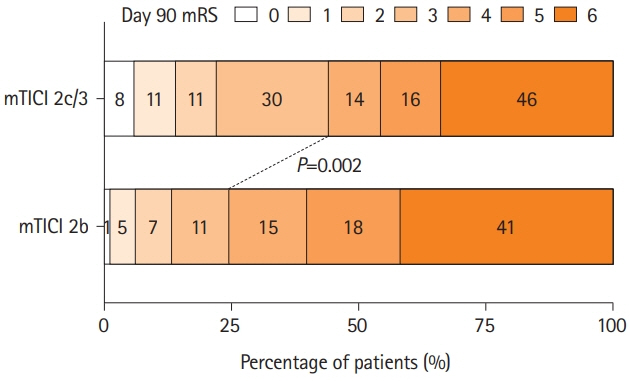
Of the 10,229 patients who underwent MT, 234 met the inclusion criteria. Of those, 98 (41.9%) achieved mTICI 2b, and 136 (58.1%) achieved mTICI 2c/3. There were no significant differences in baseline characteristics between the two groups. The 90-day favorable outcome (modified Rankin Scale score: 0–3) was significantly better in the mTICI 2c/3 group than in the mTICI 2b group (adjusted odds ratio 2.35; 95% confidence interval [CI] 1.18–4.81; P=0.02). Binomial logistic regression revealed that achieving mTICI 2c/3 was significantly associated with higher odds of a favorable 90-day outcome (odds ratio 2.14; 95% CI 1.07–4.41; P=0.04).
Conclusion
In patients with low ASPECTS, achieving an mTICI 2c/3 score after MT is associated with a more favorable 90-day outcome. These findings suggest that mTICI 2c/3 is a better target for MT than mTICI 2b in patients with low ASPECTS.
Keyword
Figure
Reference
-
References
1. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.2. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.3. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO)- European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019; 11:535–538.4. LeCouffe NE, Kappelhof M, Treurniet KM, Lingsma HF, Zhang G, van den Wijngaard IR, et al. 2B, 2C, or 3: what should be the angiographic target for endovascular treatment in ischemic stroke? Stroke. 2020; 51:1790–1796.5. Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, et al. First pass effect: a new measure for stroke thrombectomy devices. Stroke. 2018; 49:660–666.6. Nikoubashman O, Dekeyzer S, Riabikin A, Keulers A, Reich A, Mpotsaris A, et al. True first-pass effect. Stroke. 2019; 50:2140–2146.7. Flottmann F, Brekenfeld C, Broocks G, Leischner H, McDonough R, Faizy TD, et al. Good clinical outcome decreases with number of retrieval attempts in stroke thrombectomy: beyond the first-pass effect. Stroke. 2021; 52:482–490.8. Flottmann F, van Horn N, Maros ME, Leischner H, Bechstein M, Meyer L, et al. More retrieval attempts are associated with poorer functional outcome after unsuccessful thrombectomy. Clin Neuroradiol. 2022; 32:361–368.9. Alawieh A, Vargas J, Fargen KM, Langley EF, Starke RM, De Leacy R, et al. Impact of procedure time on outcomes of thrombectomy for stroke. J Am Coll Cardiol. 2019; 73:879–890.10. Almallouhi E, Al Kasab S, Hubbard Z, Bass EC, Porto G, Alawieh A, et al. Outcomes of mechanical thrombectomy for patients with stroke presenting with low Alberta Stroke Program Early Computed Tomography Score in the early and extended window. JAMA Netw Open. 2021; 4:e2137708.11. Hungerford JP, Hyer M, Turk AS, Turner RD, Chaudry MI, Fargen KM, et al. Impact of ASPECT scores and infarct distribution on outcomes among patients undergoing thrombectomy for acute ischemic stroke with the ADAPT technique. J Neurointerv Surg. 2017; 9:823–829.12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007; 370:1453–1457.13. Manning NW, Chapot R, Meyers PM. Endovascular stroke management: key elements of success. Cerebrovasc Dis. 2016; 42:170–177.14. Badhiwala JH, Nassiri F, Alhazzani W, Selim MH, Farrokhyar F, Spears J, et al. Endovascular thrombectomy for acute ischemic stroke: a meta-analysis. JAMA. 2015; 314:1832–1843.15. Hacke W, Kaste M, Fieschi C, Toni D, Lesaffre E, von Kummer R, et al. Intravenous thrombolysis with recombinant tissue plasminogen activator for acute hemispheric stroke. The European Cooperative Acute Stroke Study (ECASS). JAMA. 1995; 274:1017–1025.16. Haley EC Jr, Levy DE, Brott TG, Sheppard GL, Wong MC, Kongable GL, et al. Urgent therapy for stroke. Part II. Pilot study of tissue plasminogen activator administered 91-180 minutes from onset. Stroke. 1992; 23:641–645.17. Brott TG, Haley EC Jr, Levy DE, Barsan W, Broderick J, Sheppard GL, et al. Urgent therapy for stroke. Part I. Pilot study of tissue plasminogen activator administered within 90 minutes. Stroke. 1992; 23:632–640.18. Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med. 2023; 388:1272–1283.19. Yoshimura S, Sakai N, Yamagami H, Uchida K, Beppu M, Toyoda K, et al. Endovascular therapy for acute stroke with a large ischemic region. N Engl J Med. 2022; 386:1303–1313.20. Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023; 388:1259–1271.21. Campbell BCV, Majoie CBLM, Albers GW, Menon BK, Yassi N, Sharma G, et al. Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy: a meta-analysis of individual patient-level data. Lancet Neurol. 2019; 18:46–55.22. Román LS, Menon BK, Blasco J, Hernández-Pérez M, Dávalos A, Majoie CBLM, et al. Imaging features and safety and efficacy of endovascular stroke treatment: a meta-analysis of individual patient-level data. Lancet Neurol. 2018; 17:895–904.23. Mourand I, Abergel E, Mantilla D, Ayrignac X, Sacagiu T, Eker OF, et al. Favorable revascularization therapy in patients with ASPECTS ≤ 5 on DWI in anterior circulation stroke. J Neurointerv Surg. 2018; 10:5–9.24. Kaesmacher J, Chaloulos-Iakovidis P, Panos L, Mordasini P, Michel P, Hajdu SD, et al. Mechanical thrombectomy in ischemic stroke patients With Alberta Stroke Program Early Computed Tomography Score 0-5. Stroke. 2019; 50:880–888.25. Cagnazzo F, Derraz I, Dargazanli C, Lefevre PH, Gascou G, Riquelme C, et al. Mechanical thrombectomy in patients with acute ischemic stroke and ASPECTS ≤6: a meta-analysis. J Neurointerv Surg. 2020; 12:350–355.26. Yoo AJ, Berkhemer OA, Fransen PSS, van den Berg LA, Beumer D, Lingsma HF, et al. Effect of baseline Alberta Stroke Program Early CT Score on safety and efficacy of intra-arterial treatment: a subgroup analysis of a randomised phase 3 trial (MR CLEAN). Lancet Neurol. 2016; 15:685–694.27. Liebeskind DS, Bracard S, Guillemin F, Jahan R, Jovin TG, Majoie CB, et al. eTICI reperfusion: defining success in endovascular stroke therapy. J Neurointerv Surg. 2019; 11:433–438.28. Flottmann F, Leischner H, Broocks G, Nawabi J, Bernhardt M, Faizy TD, et al. Recanalization rate per retrieval attempt in mechanical thrombectomy for acute ischemic stroke. Stroke. 2018; 49:2523–2525.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intra-Arterial Thrombolysis to Improve Final Thrombolysis in Cerebral Infarction Score after Thrombectomy: A Case-Series Analysis
- DIRECT-SAFE: A Randomized Controlled Trial of DIRECT Endovascular Clot Retrieval versus Standard Bridging Therapy
- A “Radial Ready” Tricoaxial Setup for Anterior Circulation Mechanical Thrombectomy: Technical Aspects and Preliminary Results
- Single Centre Experience on Decision Making for Mechanical Thrombectomy Based on Single-Phase CT Angiography by Including NCCT and Maximum Intensity Projection Images – A Comparison with Magnetic Resonance Imaging after Non-Contrast CT
- Predictors of Good Outcomes in Patients with FailedEndovascular Thrombectomy