J Stroke.
2024 Jan;26(1):54-63. 10.5853/jos.2023.04119.
Standard Versus Intensive Blood Pressure Control in Acute Ischemic Stroke Patients Successfully Treated With Endovascular Thrombectomy: A Systemic Review and Meta-Analysis of Randomized Controlled Trials
- Affiliations
-
- 1Department of Neurology, Keimyung University School of Medicine, Daegu, Korea
- 2Department of Convergence Medicine, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- 3Department of Anatomy, School of Medicine, Pusan National University, Yangsan, Korea
- 4Department of Neurology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, Seoul, Korea
- KMID: 2551347
- DOI: http://doi.org/10.5853/jos.2023.04119
Abstract
- Background and Purpose
The optimal blood pressure (BP) control after successful endovascular thrombectomy (EVT) in acute ischemic stroke (AIS) with large vessel occlusion (LVO) remains debatable. We conducted a systematic review and meta-analysis of randomized controlled trials (RCTs) that evaluate the efficacy and safety of standard BP control (with systolic BP ≤180 mm Hg) versus intensive BP control (systolic BP <140 mm Hg) during the 24 hours after successful EVT in AIS with LVO.
Methods
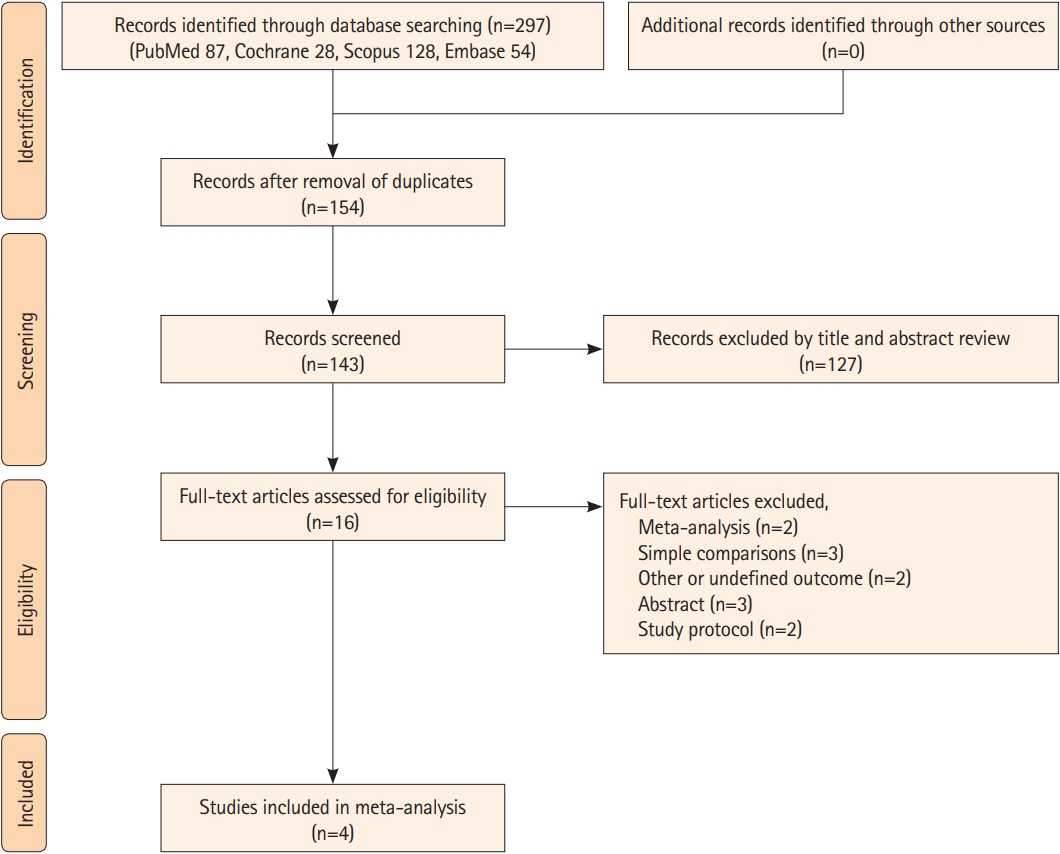
PubMed, Scopus, the Cochrane Central Register of Controlled Trials, and Embase were searched to identify relevant trials. The crude odds ratio (OR) and 95% confidence interval (CI) were calculated and estimates using random-effects models were pooled. This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (PROSPERO ID: CRD42023450673).
Results
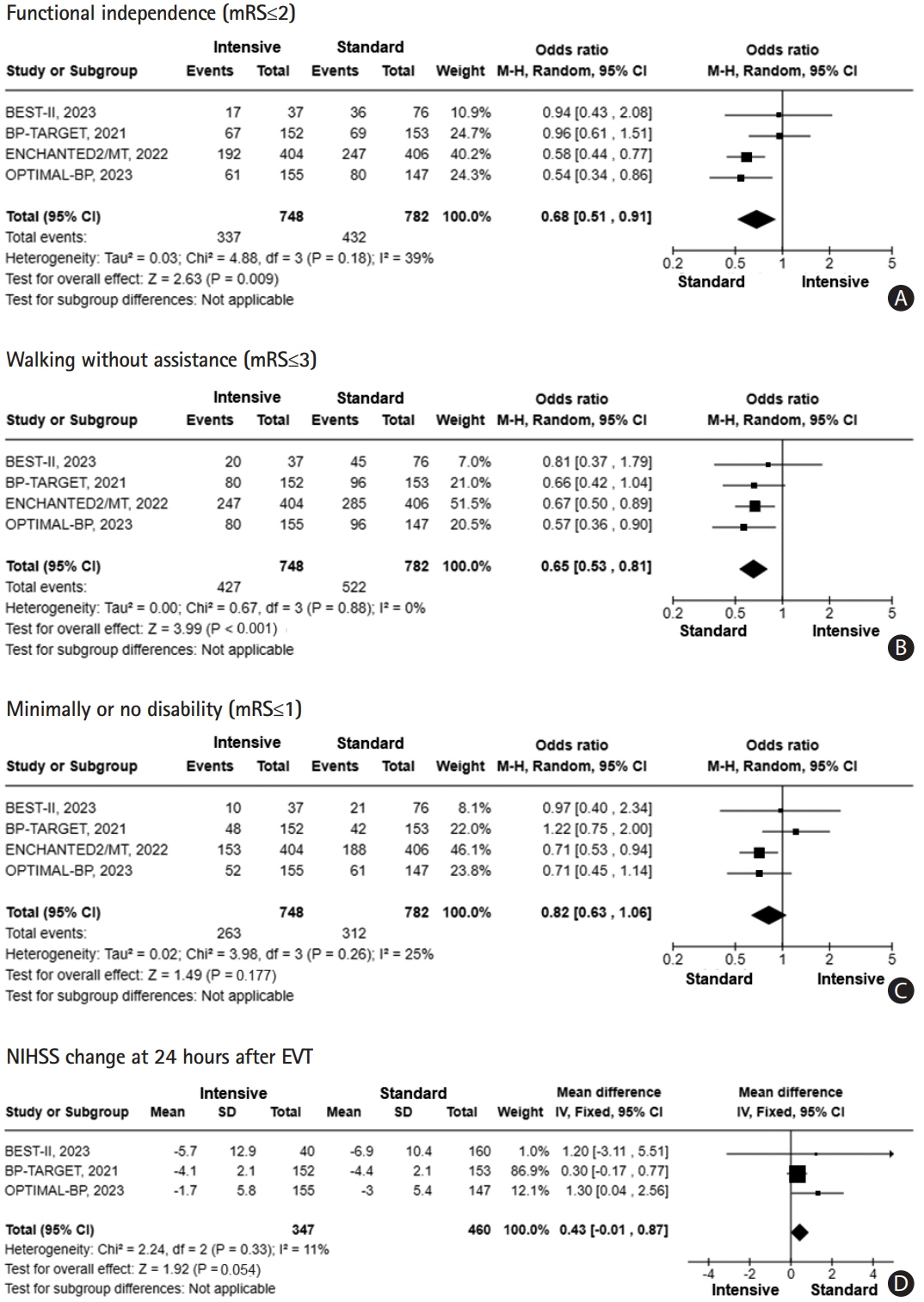
Four RCTs involving 1,559 participants were included. Regarding efficacy outcomes, intensive BP control was associated with a lower likelihood of functional independence (OR: 0.68; 95% CI: 0.51–0.91 for modified Rankin Scale [mRS] ≤2) and walking without assistance (OR: 0.65; 95% CI: 0.53–0.81 for mRS ≤3). For safety outcomes, consistent with the efficacy findings, intensive BP control was significantly associated with severe disability or death (mRS 5 or 6) (OR: 1.34; 95% CI: 1.07–1.69). However, there were no significant differences including all-cause mortality, any intracerebral hemorrhage (ICH), symptomatic ICH, parenchymal hematoma type 2, and stroke recurrence.
Conclusion
While all four RCTs were conducted to demonstrate the superiority of intensive BP control over standard BP control, standard BP control may be beneficial for the outcome after EVT for AIS with LVO without increasing adverse safety outcomes. Caution should be needed with the application of intensive BP control during the 24 hours following successful recanalization after EVT.
Figure
Reference
-
References
1. Galecio-Castillo M, Farooqui M, Hassan AE, Jumaa MA, Divani AA, Ribo M, et al. Clinical and safety outcomes of endovascular therapy 6 to 24 hours after large vessel occlusion ischemic stroke with tandem lesions. J Stroke. 2023; 25:378–387.2. Morsi RZ, Elfil M, Ghaith HS, Aladawi M, Elmashad A, Kothari S, et al. Endovascular thrombectomy for large ischemic strokes: a living systematic review and meta-analysis of randomized trials. J Stroke. 2023; 25:214–222.3. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.4. Lapergue B, Blanc R, Costalat V, Desal H, Saleme S, Spelle L, et al. Effect of thrombectomy with combined contact aspiration and stent retriever vs stent retriever alone on revascularization in patients with acute ischemic stroke and large vessel occlusion: the ASTER2 randomized clinical trial. JAMA. 2021; 326:1158–1169.5. Jiang QM, Yu S, Dong XF, Wang HS, Hou J, Huang ZC, et al. Predictors and dynamic nomogram to determine the individual risk of malignant brain edema after endovascular thrombectomy in acute ischemic stroke. J Clin Neurol. 2022; 18:298–307.6. Maier IL, Tsogkas I, Behme D, Bähr M, Knauth M, Psychogios MN, et al. High systolic blood pressure after successful endovascular treatment affects early functional outcome in acute ischemic stroke. Cerebrovasc Dis. 2018; 45:18–25.7. Goyal N, Tsivgoulis G, Pandhi A, Chang JJ, Dillard K, Ishfaq MF, et al. Blood pressure levels post mechanical thrombectomy and outcomes in large vessel occlusion strokes. Neurology. 2017; 89:540–547.8. Martins AI, Sargento-Freitas J, Silva F, Jesus-Ribeiro J, Correia I, Gomes JP, et al. Recanalization modulates association between blood pressure and functional outcome in acute ischemic stroke. Stroke. 2016; 47:1571–1576.9. Heo JH, Lucero J, Abumiya T, Koziol JA, Copeland BR, del Zoppo GJ. Matrix metalloproteinases increase very early during experimental focal cerebral ischemia. J Cereb Blood Flow Metab. 1999; 19:624–633.10. Heo JH, Han SW, Lee SK. Free radicals as triggers of brain edema formation after stroke. Free Radic Biol Med. 2005; 39:51–70.11. Kim BJ, Singh N, Menon BK. Hemodynamics of leptomeningeal collaterals after large vessel occlusion and blood pressure management with endovascular treatment. J Stroke. 2021; 23:343–357.12. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.13. Turc G, Bhogal P, Fischer U, Khatri P, Lobotesis K, Mazighi M, et al. European Stroke Organisation (ESO) - European Society for Minimally Invasive Neurological Therapy (ESMINT) guidelines on mechanical thrombectomy in acute ischemic stroke. J Neurointerv Surg. 2019; 11:535–538.14. Sandset EC, Anderson CS, Bath PM, Christensen H, Fischer U, Ga ¸secki D, et al. European Stroke Organisation (ESO) guidelines on blood pressure management in acute ischaemic stroke and intracerebral haemorrhage. Eur Stroke J. 2021; 6:XLVIII–LXXXIX.15. Matusevicius M, Cooray C, Bottai M, Mazya M, Tsivgoulis G, Nunes AP, et al. Blood pressure after endovascular thrombectomy: modeling for outcomes based on recanalization status. Stroke. 2020; 51:519–525.16. Anadani M, Arthur AS, Tsivgoulis G, Simpson KN, Alawieh A, Orabi Y, et al. Blood pressure goals and clinical outcomes after successful endovascular therapy: a multicenter study. Ann Neurol. 2020; 87:830–839.17. Petersen NH, Kodali S, Meng C, Li F, Nguyen CK, Peshwe KU, et al. Blood pressure trajectory groups and outcome after endovascular thrombectomy: a multicenter study. Stroke. 2022; 53:1216–1225.18. Mistry EA, Sucharew H, Mistry AM, Mehta T, Arora N, Starosciak AK, et al. Blood pressure after endovascular therapy for ischemic stroke (BEST): a multicenter prospective cohort study. Stroke. 2019; 50:3449–3455.19. Katsanos AH, Malhotra K, Ahmed N, Seitidis G, Mistry EA, Mavridis D, et al. Blood pressure after endovascular thrombectomy and outcomes in patients with acute ischemic stroke: an individual patient data meta-analysis. Neurology. 2022; 98:e291–e301.20. Mistry EA, Hart KW, Davis LT, Gao Y, Prestigiacomo CJ, Mittal S, et al. Blood pressure management after endovascular therapy for acute ischemic stroke: the BEST-II randomized clinical trial. JAMA. 2023; 330:821–831.21. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021; 372:n71.22. Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. 2nd ed. Hoboken, NJ: John Wiley & Sons, Inc;2019.23. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.24. Sterne JAC, Savovic ´ J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898.25. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008; 336:924–926.26. Mazighi M, Richard S, Lapergue B, Sibon I, Gory B, Berge J, et al. Safety and efficacy of intensive blood pressure lowering after successful endovascular therapy in acute ischaemic stroke (BP-TARGET): a multicentre, open-label, randomised controlled trial. Lancet Neurol. 2021; 20:265–274.27. Yang P, Song L, Zhang Y, Zhang X, Chen X, Li Y, et al. Intensive blood pressure control after endovascular thrombectomy for acute ischaemic stroke (ENCHANTED2/MT): a multicentre, open-label, blinded-endpoint, randomised controlled trial. Lancet. 2022; 400:1585–1596.28. Nam HS, Kim YD, Heo J, Lee H, Jung JW, Choi JK, et al. Intensive vs conventional blood pressure lowering after endovascular thrombectomy in acute ischemic stroke: the OPTIMALBP randomized clinical trial. JAMA. 2023; 330:832–842.29. Béjot Y. Targeting blood pressure for stroke prevention: current evidence and unanswered questions. J Neurol. 2021; 268:785–795.30. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020; 75:285–292.31. Ruland S, Aiyagari V. Cerebral autoregulation and blood pressure lowering. Hypertension. 2007; 49:977–978.32. Peng TJ, Ortega-Gutiérrez S, de Havenon A, Petersen NH. Blood pressure management after endovascular thrombectomy. Front Neurol. 2021; 12:723461.33. Lee JS, Hwang YH, Sohn SI. Factors contributing to an efficacious endovascular treatment for acute ischemic stroke in Asian population. Neurointervention. 2021; 16:91–110.34. Zhang Z, Pu Y, Mi D, Liu L. Cerebral hemodynamic evaluation after cerebral recanalization therapy for acute ischemic stroke. Front Neurol. 2019; 10:719.35. Mastorakos P, Liu KC, Schomer A. Adverse effects of aggressive blood pressure control in patients with intracerebral hemorrhage. J Neurocrit Care. 2017; 10:36–40.36. Silverman A, Kodali S, Sheth KN, Petersen NH. Hemodynamics and hemorrhagic transformation after endovascular therapy for ischemic stroke. Front Neurol. 2020; 11:728.37. Anadani M, Orabi MY, Alawieh A, Goyal N, Alexandrov AV, Petersen N, et al. Blood pressure and outcome after mechanical thrombectomy with successful revascularization. Stroke. 2019; 50:2448–2454.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endovascular Treatment of Acute Ischemic Stroke
- Endovascular Thrombectomy for Acute Ischemic Stroke : Current Concept in Management
- Endovascular Thrombectomy for Large Ischemic Strokes: A Living Systematic Review and Meta-Analysis of Randomized Trials
- Endovascular Mechanical Thrombectomy for Acute Ischemic Stroke: A New Standard of Care
- Causes and Solutions of Endovascular Treatment Failure