Pediatr Emerg Med J.
2024 Jan;11(1):17-27. 10.22470/pemj.2023.00836.
Incidence, severity, and clinical characteristics of lower respiratory tract infections in children before and after the coronavirus disease 2019 lockdown: a Dutch single-center study
- Affiliations
-
- 1Juliana Children’s Hospital, Haga Teaching Hospital, the Hague, the Netherlands
- 2University Medical Centre Groningen, Groningen, the Netherlands
- 3Department of Pediatrics, Isala Ziekenhuis, Zwolle, the Netherlands
- 4Department of Pediatrics, Leiden University Medical Centre, Leiden, the Netherlands
- KMID: 2549537
- DOI: http://doi.org/10.22470/pemj.2023.00836
Abstract
- Purpose
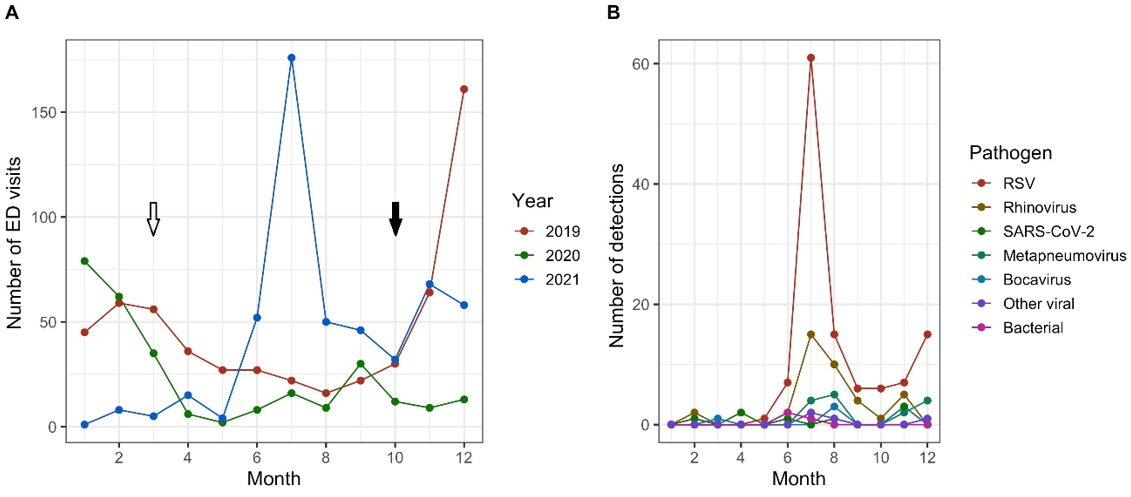
Coronavirus disease 2019 (COVID-19) public health measures reduced the incidence of pediatric lower respiratory tract infections (LRTIs) in 2020. An inter-seasonal surge in the LRTI has occurred after relaxation of restrictions. We aimed to compare characteristics and disease severity of children with LRTI before, during, and after COVID-19 lockdown.
Methods
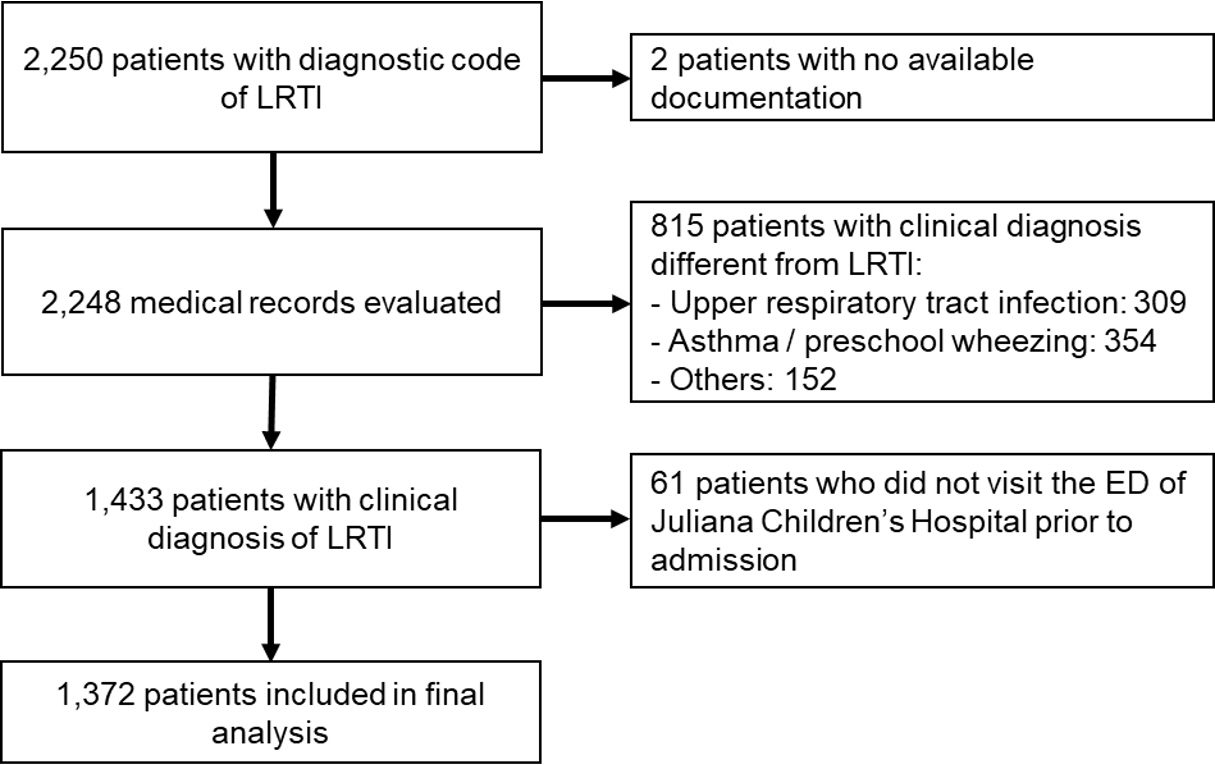
All LRTI-related visits to emergency department (ED) of a large pediatric hospital in the Netherlands between 2019 and 2021 were included. Variables were compared between 2019 and 2020, and between 2019 and 2021, respectively. The variables included demographic characteristics, condition upon ED arrival, diagnosis, applied treatment, and follow-up.
Results
In 2019, 2020, and 2021, numbers of the visits were 573, 280, and 519, respectively, comprising the study population (n = 1,372). In 2020, the patients were older, and showed higher frequencies of preterm birth history, co-occurring symptoms of obstructive lung disease, and salbutamol therapy in the ED, than in 2019. In 2021, the patients were younger, showed higher frequencies of desaturation, bronchiolitis, co-occurring symptoms of obstructive lung disease, salbutamol therapy, and hospitalization, and showed lower frequencies of respiratory ED visits or hospitalization in the past year, and antibiotic therapy. During hospitalization in 2020, the patients were older, and showed shorter duration of oxygen support and length of hospital stay, as well as lower frequencies of nasogastric tube insertion, compared to 2019. In 2021, compared to 2019, the patients showed a higher frequency of bronchiolitis and lower frequencies of underlying medical conditions and antibiotic therapy.
Conclusion
The children presenting with LRTIs in 2021 seem to have had a more severe clinical phenotype, possibly explained by immunity debt after the COVID-19 lockdown, stricter referral policy, or changes in healthcare-seeking behavior. Future research is needed to evaluate the long-term consequences of growing up during the lockdown.
Keyword
Figure
Reference
-
References
1. Schrijver TV, Brand PL, Bekhof J. Seasonal variation of diseases in children: a 6-year prospective cohort study in a general hospital. Eur J Pediatr. 2016; 175:457–64.2. Finkelman BS, Viboud C, Koelle K, Ferrari MJ, Bharti N, Grenfell BT. Global patterns in seasonal activity of influenza A/H3N2, A/H1N1, and B from 1997 to 2005: viral coexistence and latitudinal gradients. PLoS One. 2007; 2:e1296.3. Lipsett SC, Monuteaux MC, Fine AM. Seasonality of common pediatric infectious diseases. Pediatr Emerg Care. 2021; 37:82–5.4. Ben-Shimol S, Greenberg D, Hazan G, Shemer-Avni Y, Givon-Lavi N, Dagan R. Seasonality of both bacteremic and nonbacteremic pneumonia coincides with viral lower respiratory tract infections in early childhood, in contrast to nonpneumonia invasive pneumococcal disease, in the pre-pneumococcal conjugate vaccine era. Clin Infect Dis. 2015; 60:1384–7.5. Florin TA, Plint AC, Zorc JJ. Viral bronchiolitis. Lancet. 2017; 389:211–24.6. Jin Y, Yang H, Ji W, Wu W, Chen S, Zhang W, et al. Virology, epidemiology, pathogenesis, and control of COVID-19. Viruses. 2020; 12:372.7. World Health Organization (WHO). WHO coronavirus (COVID-19) dashboard: Measures [Internet]. WHO; 2020 [cited 2022 Apr 1]. Available from: https://covid19.who.int/measures.8. Government of the Netherlands. Coronavirus timeline [Internet]. Government of the Netherlands; 2021 [cited 2022 Mar 14]. Available from: https://www.rijksoverheid.nl/onderwerpen/coronavirus-tijdlijn. Dutch.9. Kruizinga MD, Noordzij JG, van Houten MA, Wieringa J, Tramper-Stranders GA, Hira V, et al. Effect of lockdowns on the epidemiology of pediatric respiratory disease: a retrospective analysis of the 2021 summer epidemic. Pediatr Pulmonol. 2023; 58:1229–36.10. Launay T, Souty C, Vilcu AM, Turbelin C, Blanchon T, Guerrisi C, et al. Common communicable diseases in the general population in France during the COVID-19 pandemic. PLoS One. 2021; 16:e0258391.11. Sullivan SG, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020; 25:2001847.12. Kuitunen I, Artama M, Mäkelä L, Backman K, Heiskanen-Kosma T, Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in finland during early 2020. Pediatr Infect Dis J. 2020; 39:e423–7.13. Kishimoto K, Bun S, Shin JH, Takada D, Morishita T, Kunisawa S, et al. Early impact of school closure and social distancing for COVID-19 on the number of inpatients with childhood non-COVID-19 acute infections in Japan. Eur J Pediatr. 2021; 180:2871–8.14. Tanislav C, Kostev K. Fewer non-COVID-19 respiratory tract infections and gastrointestinal infections during the COVID-19 pandemic. J Med Virol. 2022; 94:298–302.15. Van Brusselen D, De Troeyer K, Ter Haar E, Vander Auwera A, Poschet K, Van Nuijs S, et al. Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr. 2021; 180:1969–73.16. Stera G, Pierantoni L, Masetti R, Leardini D, Biagi C, Buonsenso D, et al. Impact of SARS-CoV-2 pandemic on bronchiolitis hospitalizations: the experience of an Italian tertiary center. Children (Basel). 2021; 8:556.17. Lumley SF, Richens N, Lees E, Cregan J, Kalimeris E, Oakley S, et al. Changes in paediatric respiratory infections at a UK teaching hospital 2016-2021; impact of the SARS-CoV-2 pandemic. J Infect. 2022; 84:40–7.18. Rybak A, Yang DD, Schrimpf C, Guedj R, Levy C, Cohen R, et al. Fall of community-acquired pneumonia in children following COVID-19 non-pharmaceutical interventions: a time series analysis. Pathogens. 2021; 10:1375.19. Yeoh DK, Foley DA, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. Impact of coronavirus disease 2019 public health measures on detections of influenza and respiratory syncytial virus in children during the 2020 Australian winter. Clin Infect Dis. 2021; 72:2199–202.20. Britton PN, Hu N, Saravanos G, Shrapnel J, Davis J, Snelling T, et al. COVID-19 public health measures and respiratory syncytial virus. Lancet Child Adolesc Health. 2020; 4:e42–3.21. Varela FH, Scotta MC, Polese-Bonatto M, Sartor IT, Ferreira CF, Fernandes IR, et al. Absence of detection of RSV and influenza during the COVID-19 pandemic in a Brazilian cohort: likely role of lower transmission in the community. J Glob Health. 2021; 11:05007.22. Chiapinotto S, Sarria EE, Mocelin HT, Lima JA, Mattiello R, Fischer GB. Impact of non-pharmacological initiatives for COVID-19 on hospital admissions due to pediatric acute respiratory illnesses. Paediatr Respir Rev. 2021; 39:3–8.23. Agha R, Avner JR. Delayed seasonal RSV surge observed during the COVID-19 pandemic. Pediatrics. 2021; 148:e2021052089.24. Delestrain C, Danis K, Hau I, Behillil S, Billard MN, Krajten L, et al. Impact of COVID-19 social distancing on viral infection in France: a delayed outbreak of RSV. Pediatr Pulmonol. 2021; 56:3669–73.25. Weinberger Opek M, Yeshayahu Y, Glatman-Freedman A, Kaufman Z, Sorek N, Brosh-Nissimov T. Delayed respiratory syncytial virus epidemic in children after relaxation of COVID-19 physical distancing measures, Ashdod, Israel, 2021. Euro Surveill. 2021; 26:2100706.26. Masarweh K, Gur M, Bar-Yoseph R, Bentur L, Dabaja-Younis H. Characterization of respiratory illness surge (April-June 2021) post-COVID-19 lockdown. Pediatr Pulmonol. 2022; 57:667–73.27. Foley DA, Phuong LK, Peplinski J, Lim SM, Lee WH, Farhat A, et al. Examining the interseasonal resurgence of respiratory syncytial virus in Western Australia. Arch Dis Child. 2022; 107:e7.28. Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021; 73:e2829–30.29. Saravanos GL, Hu N, Homaira N, Muscatello DJ, Jaffe A, Bartlett AW, et al. RSV epidemiology in Australia before and during COVID-19. Pediatrics. 2022; 149:e2021053537.30. Hatter L, Eathorne A, Hills T, Bruce P, Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021; 5:e44–5.31. Cohen R, Ashman M, Taha MK, Varon E, Angoulvant F, Levy C, et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021; 51:418–23.32. Cohen R, Pettoello-Mantovani M, Somekh E, Levy C. European Pediatric Societies call for an implementation of regular vaccination programs to contrast the immunity debt associated to coronavirus disease-2019 pandemic in children. J Pediatr. 2022; 242:260–261.e3.33. Camporesi A, Morello R, Ferro V, Pierantoni L, Rocca A, Lanari M, et al. Epidemiology, microbiology and severity of bronchiolitis in the first post-lockdown cold season in three different geographical areas in Italy: a prospective, observational study. Children (Basel). 2022; 9:491.34. Fourgeaud J, Toubiana J, Chappuy H, Delacourt C, Moulin F, Parize P, et al. Impact of public health measures on the post-COVID-19 respiratory syncytial virus epidemics in France. Eur J Clin Microbiol Infect Dis. 2021; 40:2389–95.35. Abe N, Yasudo H, Fukano R, Nakamura T, Okada S, Wakiguchi H, et al. Multi-season analyses of causative pathogens in children hospitalized with asthma exacerbation. Pediatr Allergy Immunol. 2019; 30:724–31.36. Kengne-Nde C, Kenmoe S, Modiyinji AF, Njouom R. Prevalence of respiratory viruses using polymerase chain reaction in children with wheezing, a systematic review and meta-analysis. PLoS One. 2020; 15:e0243735.37. Reukers DF, van Asten L, Brandsema PS, Dijkstra F, Hendriksen JM, Hooiveld M, et al. Annual report surveillance of COVID-19, influenza and other respiratory infections in the Netherlands: winter 2020/2021 [Internet]. National Institute for Public Health and the Environment; 2021 [cited 2022 Aug 9]. Available from: https://www.rivm.nl/bibliotheek/rapporten/2021-0133.pdf.38. Tenenbaum T, Doenhardt M, Diffloth N, Berner R, Armann JP. High burden of RSV hospitalizations in Germany 2021-2022. Infection. 2022; 50:1587–90.39. Cardenas J, Pringle C, Filipp SL, Gurka MJ, Ryan KA, Avery KL. Changes in critical bronchiolitis after COVID-19 lockdown. Cureus. 2022; 14:e25064.40. Garn H, Potaczek DP, Pfefferle PI. The hygiene hypothesis and new perspectives-current challenges meeting an old postulate. Front Immunol. 2021; 12:637087.41. Brooks C, Pearce N, Douwes J. The hygiene hypothesis in allergy and asthma: an update. Curr Opin Allergy Clin Immunol. 2013; 13:70–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Human Coronavirus in the 2014 Winter Season as a Cause of Lower Respiratory Tract Infection
- Clinical Characteristics of Acute Respiratory Tract Infections in Full-Term Newborns without Risk Factors
- Middle East Respiratory Syndrome Coronavirus Infection in Children
- Coronavirus Disease 2019: Reasons for Better Clinical Course for Children Compared to Adults