Clin Exp Otorhinolaryngol.
2023 Nov;16(4):395-402. 10.21053/ceo.2023.01046.
Pathophysiological Mechanisms Underlying Unilateral Vocal Fold Paralysis in Female Patients: An Ultrasonographic Study
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
- 2Master of Science Degree Program in Innovation for Smart Medicine, Chang Gung University, Taoyuan, Taiwan
- 3Department of Medical Education, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
- 4Department of Physical Medicine and Rehabilitation, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
- 5Center of Vascularized Tissue Allograft, Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
- 6Graduate School of Science Design Program in Innovation for Smart Medicine, Chang Gung University, Taoyuan, Taiwan
- KMID: 2548368
- DOI: http://doi.org/10.21053/ceo.2023.01046
Abstract
Objectives
. Laryngeal ultrasonography (LUS) has been suggested as an alternative diagnostic tool for unilateral vocal fold paralysis (UVFP). The present study applied LUS and quantitative laryngeal electromyography (LEMG) in female UVFP patients to investigate the pathophysiologic mechanisms of UVFP.
Methods
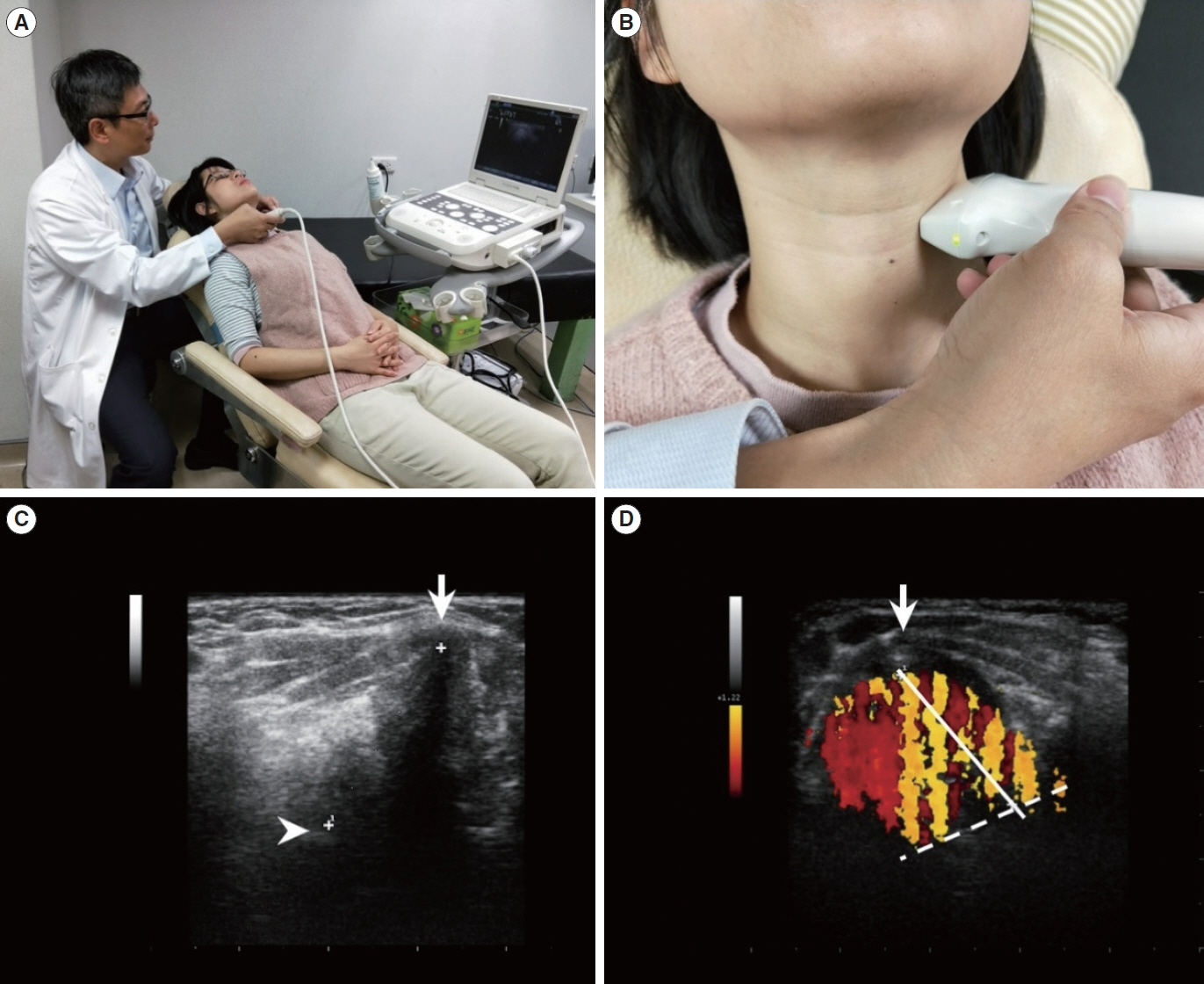
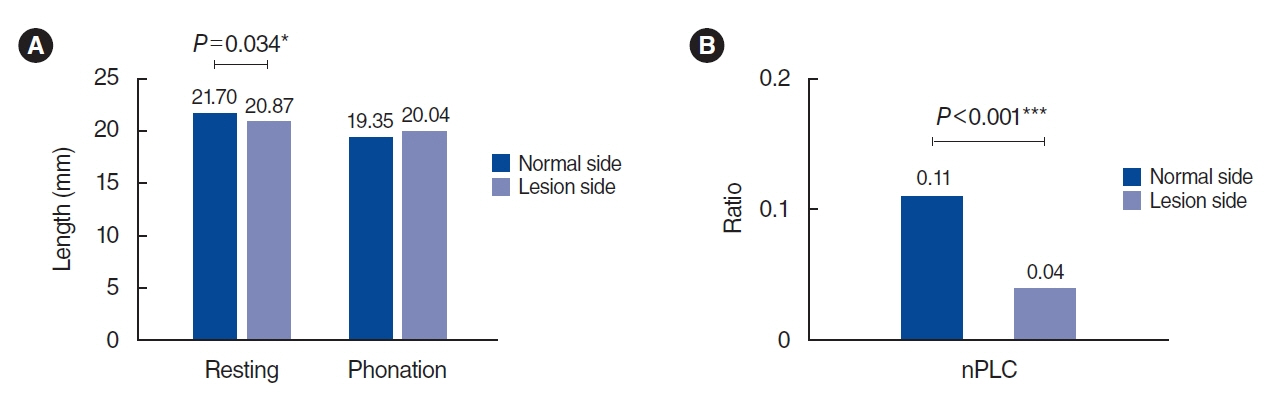
. In this cross-sectional study, vocal fold (VF) length parameters included resting and phonating VF length measured using B-mode LUS, and color Doppler vibrating length (CDVL) measured using the color Doppler mode.
Results
. Forty female patients with UVFP were enrolled, among whom 11 and 29 were assigned to the thyroarytenoid (TA) muscle+cricothyroid (CT) muscle group (with CT involvement) and the TA (without CT involvement) group, respectively. In the TA group, the turn frequency in thyroarytenoid-lateral cricoarytenoid (TA-LCA) on the paralyzed side, as observed through LEMG, correlated with the VF length during the resting phase (R=0.368, P=0.050) and CDVL values (R=0.627, P=0.000) on the paralyzed side. In the TA+CT group, the turn ratio in the CT muscle correlated with the normalized phonatory vocal length change (nPLC; R=0.621, P=0.041) on the paralyzed side.
Conclusion
. CDVL and nPLC are two parameters that can be utilized to predict the turn frequencies of TA-LCA in UVFP cases without CT involvement, and the turn ratio of CT in cases of UVFP with CT involvement, respectively. The findings suggest that LUS, as a noninvasive tool, can serve as an alternative method for assessing the severity of laryngeal nerve injury and offer valuable insights into the pathophysiology of UVFP.
Keyword
Figure
Reference
-
1. Rosenthal LH, Benninger MS, Deeb RH. Vocal fold immobility: a longitudinal analysis of etiology over 20 years. Laryngoscope. 2007; Oct. 117(10):1864–70.2. Wang HW, Lu CC, Chao PZ, Lee FP. Causes of vocal fold paralysis. Ear Nose Throat J. 2022; Aug. 101(7):NP294-8.3. Francis DO, Sherman AE, Hovis KL, Bonnet K, Schlundt D, Garrett CG, et al. Life experience of patients with unilateral vocal fold paralysis. JAMA Otolaryngol Head Neck Surg. 2018; May. 144(5):433–9.4. Pei YC, Lu YA, Wong AM, Chuang HF, Li HY, Fang TJ. Two trajectories of functional recovery in thyroid surgery related unilateral vocal cord paralysis. Surgery. 2020; Oct. 168(4):578–85.5. Pei YC, Fang TJ, Li HY, Wong AM. Cricothyroid muscle dysfunction impairs vocal fold vibration in unilateral vocal fold paralysis. Laryngoscope. 2014; Jan. 124(1):201–6.6. Liu KC, Lu YA, Lee LA, Li HY, Wong AM, Pei YC, et al. Cricothyroid muscle dysfunction affects aerodynamic performance in patients with unilateral vocal fold paralysis. J Voice. 2021 Aug 20 [Epub]. https://doi.org/10.1016/j.jvoice.2021.07.002.7. Shaw GY, Searl JP, Hoover LA. Diagnosis and treatment of unilateral cricothyroid muscle paralysis with a modified Isshiki type 4 thyroplasty. Otolaryngol Head Neck Surg. 1995; Dec. 113(6):679–88.8. Wong KP, Lang BH, Ng SH, Cheung CY, Chan CT, Lo CY. A prospective, assessor-blind evaluation of surgeon-performed transcutaneous laryngeal ultrasonography in vocal cord examination before and after thyroidectomy. Surgery. 2013; Dec. 154(6):1158–65.9. Kim DH, Lee J, Seo Y, Kim SW, Hwang SH. Perioperative transcutaneous laryngeal ultrasonography to assess vocal cord function in thyroid surgery. Am J Surg. 2022; May. 223(5):893–9.10. Patel A, Spychalski P, Aszkielowicz A, Mikaszewski B, Kobiela J. Transcutaneous laryngeal ultrasound for vocal cord paralysis assessment in patients undergoing thyroid and parathyroid surgery: a systematic review and meta-analysis. J Clin Med. 2021; Nov. 10(22):5393.11. Hu Q, Zhu SY, Luo F, Gao Y, Yang XY. High-frequency sonographic measurements of true and false vocal cords. J Ultrasound Med. 2010; Jul. 29(7):1023–30.12. Cho W, Hong J, Park H. Real-time ultrasonographic assessment of true vocal fold length in professional singers. J Voice. 2012; Nov. 26(6):819.13. Hsiao TY, Wang CL, Chen CN, Hsieh FJ, Shau YW. Elasticity of human vocal folds measured in vivo using color Doppler imaging. Ultrasound Med Biol. 2002; Sep. 28(9):1145–52.14. Fang TJ, Pei YC, Hsin LJ, Lin WN, Lee LA, Li HY, et al. Quantitative laryngeal electromyography assessment of cricothyroid function in patients with unilateral vocal fold paralysis. Laryngoscope. 2015; Nov. 125(11):2530–5.15. Campbell MJ. Statistics at square one. 12th ed. Wiley-Blackwell; 2021.16. Lammers MJ, Lea J, Westerberg BD. Guidance for otolaryngology health care workers performing aerosol generating medical procedures during the COVID-19 pandemic. J Otolaryngol Head Neck Surg. 2020; Jun. 49(1):36.17. Noel JE, Orloff LA, Sung K. Laryngeal evaluation during the COVID-19 pandemic: transcervical laryngeal ultrasonography. Otolaryngol Head Neck Surg. 2020; Jul. 163(1):51–3.18. Sciancalepore PI, Anzivino R, Petrone P, Petrone D, Quaranta N. Transcutaneous laryngeal ultrasonography: a promising tool for otolaryngologists during COVID-19. Am J Otolaryngol. 2021; JanFeb. 42(1):102772.19. Moisik SR, Lin H, Esling JH. A study of laryngeal gestures in Mandarin citation tones using simultaneous laryngoscopy and laryngeal ultrasound (SLLUS). J Int Phon Assoc. 2014; Apr. 44(1):21–58.20. Fregosi RF, Ludlow CL. Activation of upper airway muscles during breathing and swallowing. J Appl Physiol (1985). 2014; Feb. 116(3):291–301.21. Crumley RL. Unilateral recurrent laryngeal nerve paralysis. J Voice. 1994; Mar. 8(1):79–83.22. Woodson GE. Configuration of the glottis in laryngeal paralysis. I: clinical study. Laryngoscope. 1993; Nov. 103(11 Pt 1):1227–34.23. Wang CP, Chen TC, Yang TL, Chen CN, Lin CF, Lou PJ, et al. Transcutaneous ultrasound for evaluation of vocal fold movement in patients with thyroid disease. Eur J Radiol. 2012; Mar. 81(3):e288–91.24. Raghavendra BN, Horii SC, Reede DL, Rumancik WM, Persky M, Bergeron T. Sonographic anatomy of the larynx, with particular reference to the vocal cords. J Ultrasound Med. 1987; May. 6(5):225–30.25. Ooi LL, Chan HS, Soo KC. Color Doppler imaging for vocal cord palsy. Head Neck. 1995; Jan-Feb. 17(1):20–3.26. Hsiao TY, Wang CL, Chen CN, Hsieh FJ, Shau YW. Noninvasive assessment of laryngeal phonation function using color Doppler ultrasound imaging. Ultrasound Med Biol. 2001; Aug. 27(8):1035–40.27. Shau YW, Wang CL, Hsieh FJ, Hsiao TY. Noninvasive assessment of vocal fold mucosal wave velocity using color doppler imaging. Ultrasound Med Biol. 2001; Nov. 27(11):1451–60.28. Koufman JA, Walker FO, Joharji GM. The cricothyroid muscle does not influence vocal fold position in laryngeal paralysis. Laryngoscope. 1995; Apr. 105(4 Pt 1):368–72.29. Woodson GE, Murry MP, Schweizer V, Hengesteg A, Chen N, Yeung D. Unilateral cricothyroid contraction and glottic configuration. J Voice. 1998; Sep. 12(3):335–9.30. Friedman AD, Burns JA, Heaton JT, Zeitels SM. Early versus late injection medialization for unilateral vocal cord paralysis. Laryngoscope. 2010; Oct. 120(10):2042–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Vertical Level of the Paralyzed Vocal Fold in Unilateral Vocal Fold Paralysis
- Primary Thyroid Lymphoma with Vocal Fold Paralysis
- Vocal Fold Injection: Review of Indications, Techniques, and Materials for Augmentation
- A Case of Unilateral Vocal Fold Paralysis Secondary to Sarcoidosis
- Laryngeal Reinnervation as a Treatment Option for Permanent Unilateral Vocal Fold Paralysis