Restor Dent Endod.
2022 Aug;47(3):e33. 10.5395/rde.2022.47.e33.
Proximity of maxillary molar apexes to the cortical bone surface and the maxillary sinus
- Affiliations
-
- 1Department of Conservative Dentistry, School of Dentistry, Kyungpook National University, Daegu, Korea
- KMID: 2548137
- DOI: http://doi.org/10.5395/rde.2022.47.e33
Abstract
Objectives
This study aimed to analyze the proximity of maxillary molar roots to their overlying cortical bone surfaces and the maxillary sinus.
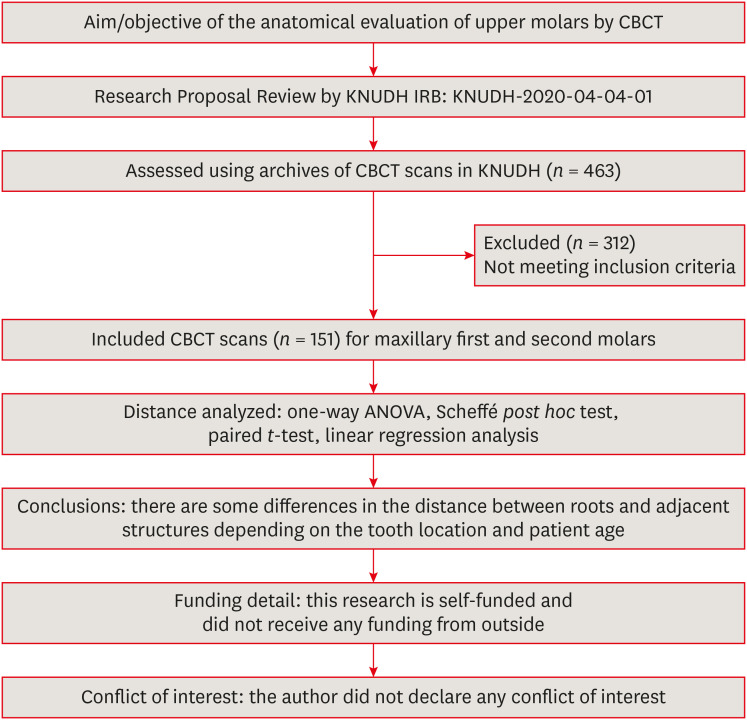
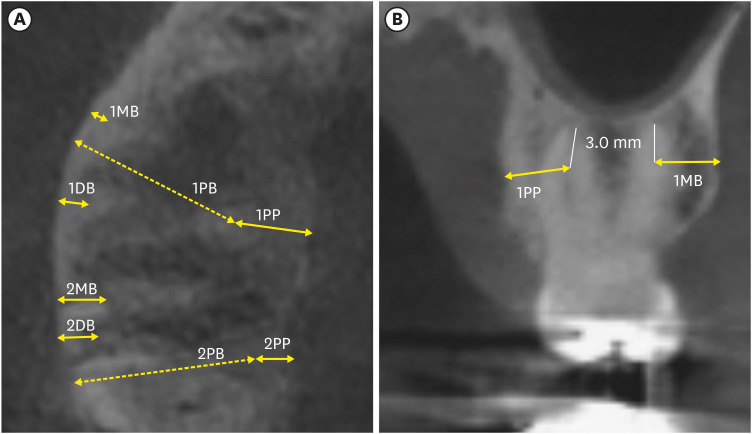
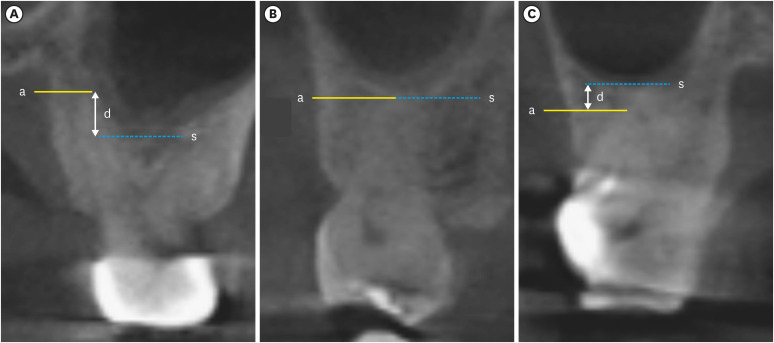
Materials and Methods
Cone-beam computed tomographic images of 151 patients with completely erupted upper molars that had 3 separate roots were studied. The following distances were measured: from the root apex to the cortical plate and maxillary sinus floor, and from the apical 3-mm level of the root to the cortical plate. Differences between groups were analyzed with 1-way analysis of variance and the Scheffé post hoc test, the significance of differences between cone-beam computed tomography views with the paired t-test, and the significance of differences among age groups with linear regression analysis. The significance level was set at p < 0.05.
Results
The mesiobuccal and distobuccal root apexes of maxillary second molars were more distant from the buccal cortical plate than the maxillary first molars (p < 0.05). The apical 3-mm level of the mesiobuccal root of the first molar was closer to the buccal cortical bone than the second molar (p < 0.05). In the maxillary first molars, the thickness of the buccal cortical bone decreased in all roots with age (p < 0.05). In all root apexes of both molars, the difference in the vertical level between the maxillary sinus floor and the root apex increased with age (p < 0.05).
Conclusions
Awareness of the anatomical profile of maxillary molar apices in relation to the cortical bones and maxillary sinus will be beneficial for apical surgery.
Figure
Reference
-
1. Maggiore F, Kim S. Chapter 7. Osteotomy. Kim S, Kratchman S, editors. Microsurgery in endodontics. Hoboken, NJ: Wiley Blackwell;2018. p. 57–65.2. Punwutikorn J, Waikakul A, Pairuchvej V. Clinically significant oroantral communications--a study of incidence and site. Int J Oral Maxillofac Surg. 1994; 23:19–21. PMID: 8163853.
Article3. Oberli K, Bornstein MM, von Arx T. Periapical surgery and the maxillary sinus: radiographic parameters for clinical outcome. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007; 103:848–853. PMID: 17197213.
Article4. Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002; 35:127–141. PMID: 11843967.
Article5. Ariji Y, Obayashi N, Goto M, Izumi M, Naitoh M, Kurita K, Shimozato K, Ariji E. Roots of the maxillary first and second molars in horizontal relation to alveolar cortical plates and maxillary sinus: computed tomography assessment for infection spread. Clin Oral Investig. 2006; 10:35–41.
Article6. Bornstein MM, Wasmer J, Sendi P, Janner SF, Buser D, von Arx T. Characteristics and dimensions of the Schneiderian membrane and apical bone in maxillary molars referred for apical surgery: a comparative radiographic analysis using limited cone beam computed tomography. J Endod. 2012; 38:51–57. PMID: 22152620.7. Lu Y, Liu Z, Zhang L, Zhou X, Zheng Q, Duan X, Zheng G, Wang H, Huang D. Associations between maxillary sinus mucosal thickening and apical periodontitis using cone-beam computed tomography scanning: a retrospective study. J Endod. 2012; 38:1069–1074. PMID: 22794207.
Article8. Phothikhun S, Suphanantachat S, Chuenchompoonut V, Nisapakultorn K. Cone-beam computed tomographic evidence of the association between periodontal bone loss and mucosal thickening of the maxillary sinus. J Periodontol. 2012; 83:557–564. PMID: 21910593.
Article9. Shanbhag S, Karnik P, Shirke P, Shanbhag V. Association between periapical lesions and maxillary sinus mucosal thickening: a retrospective cone-beam computed tomographic study. J Endod. 2013; 39:853–857. PMID: 23791251.
Article10. Watzek G, Bernhart T, Ulm C. Complications of sinus perforations and their management in endodontics. Dent Clin North Am. 1997; 41:563–583. PMID: 9248692.
Article11. Cotti E, Vargiu P, Dettori C, Mallarini G. Computerized tomography in the management and follow-up of extensive periapical lesion. Endod Dent Traumatol. 1999; 15:186–189. PMID: 10815569.12. Aggarwal V, Singla M. Use of computed tomography scans and ultrasound in differential diagnosis and evaluation of nonsurgical management of periapical lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010; 109:917–923. PMID: 20399691.
Article13. Dhamija R, Tewari S, Sangwan P, Duhan J, Mittal S. Impact of platelet-rich plasma in the healing of through-and-through periapical lesions using 2-dimensional and 3-dimensional evaluation: a randomized controlled trial. J Endod. 2020; 46:1167–1184. PMID: 32553878.
Article14. Eslami E, Barkhordar H, Abramovitch K, Kim J, Masoud MI. Cone-beam computed tomography vs conventional radiography in visualization of maxillary impacted-canine localization: a systematic review of comparative studies. Am J Orthod Dentofacial Orthop. 2017; 151:248–258. PMID: 28153153.
Article15. Low KM, Dula K, Bürgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008; 34:557–562. PMID: 18436034.
Article16. Siqueira JF Jr. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001; 34:1–10. PMID: 11307374.
Article17. Johnson BR, Fayad MI. Periradicular surgery. Hargreaves KM, Berman LH, editors. Cohen’s pathways of the pulp. 11th ed. Philadelphia, PA: Elsevier Inc.;2016. p. 387–446.18. Kim S. Chapter 9. Osteotomy and apical root resection. Color atlas of microsurgery in endodontics. Philadelphia, PA: Saunders;2000.19. Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984; 58:589–599. PMID: 6595621.
Article20. Kim D, Ha JH, Jin MU, Kim YK, Kim SK. Proximity of the mandibular molar root apex from the buccal bone surface: a cone-beam computed tomographic study. Restor Dent Endod. 2016; 41:182–188. PMID: 27508159.
Article21. Degerness RA, Bowles WR. Dimension, anatomy and morphology of the mesiobuccal root canal system in maxillary molars. J Endod. 2010; 36:985–989. PMID: 20478451.
Article22. Eberhardt JA, Torabinejad M, Christiansen EL. A computed tomographic study of the distances between the maxillary sinus floor and the apices of the maxillary posterior teeth. Oral Surg Oral Med Oral Pathol. 1992; 73:345–346. PMID: 1545967.
Article23. Jin GC, Kim KD, Roh BD, Lee CY, Lee SJ. Buccal bone plate thickness of the Asian people. J Endod. 2005; 31:430–434. PMID: 15917681.
Article25. Velasco-Torres M, Padial-Molina M, Avila-Ortiz G, García-Delgado R, O'Valle F, Catena A, Galindo-Moreno P. Maxillary sinus dimensions decrease as age and tooth loss increase. Implant Dent. 2017; 26:288–295. PMID: 28125519.
Article26. Kang SH, Kim BS, Kim Y. Proximity of posterior teeth to the maxillary sinus and buccal bone thickness: a biometric assessment using cone-beam computed tomography. J Endod. 2015; 41:1839–1846. PMID: 26411520.
Article27. NIH Osteonecrosis and Related Bone Diseases National Resource Center. NIH Pub. No. 18-7891. Osteoporosis: peak bone mass in women. Bethesda, MD: National Institutes of Health;2018.28. Timock AM, Cook V, McDonald T, Leo MC, Crowe J, Benninger BL, Covell DA Jr. Accuracy and reliability of buccal bone height and thickness measurements from cone-beam computed tomography imaging. Am J Orthod Dentofacial Orthop. 2011; 140:734–744. PMID: 22051495.
Article29. De Deus QD, Horizonte B. Frequency, location, and direction of the lateral, secondary, and accessory canals. J Endod. 1975; 1:361–366. PMID: 10697487.
Article30. Seltzer S, Soltanoff W, Bender IB, Ziontz M. Biologic aspects of endodontics, I. Histologic observations of the anatomy and morphology of root apices and surrounding structures. Oral Surg Oral Med Oral Pathol. 1966; 22:375–385.31. Wada M, Takase T, Nakanuma K, Arisue K, Nagahama F, Yamazaki M. Clinical study of refractory apical periodontitis treated by apicectomy. Part 1. Root canal morphology of resected apex. Int Endod J. 1998; 31:53–56. PMID: 9823129.
Article32. Kim S. Principles of endodontic microsurgery. Dent Clin North Am. 1997; 41:481–497. PMID: 9248686.
Article33. Jun BC, Song SW, Park CS, Lee DH, Cho KJ, Cho JH. The analysis of maxillary sinus aeration according to aging process; volume assessment by 3-dimensional reconstruction by high-resolutional CT scanning. Otolaryngol Head Neck Surg. 2005; 132:429–434. PMID: 15746857.
Article34. Sharan A, Madjar D. Maxillary sinus pneumatization following extractions: a radiographic study. Int J Oral Maxillofac Implants. 2008; 23:48–56. PMID: 18416412.35. Louie AF. Surgical and radiologic anatomy for oral implantology. 1st ed. Hanover: Quintessence Publishing;2013.36. Pagin O, Centurion BS, Rubira-Bullen IR, Alvares Capelozza AL. Maxillary sinus and posterior teeth: accessing close relationship by cone-beam computed tomographic scanning in a Brazilian population. J Endod. 2013; 39:748–751. PMID: 23683273.
Article37. Kilic C, Kamburoglu K, Yuksel SP, Ozen T. An assessment of the relationship between the maxillary sinus floor and the maxillary posterior teeth root tips using dental cone-beam computerized tomography. Eur J Dent. 2010; 4:462–467. PMID: 20922167.
Article38. Rigolone M, Pasqualini D, Bianchi L, Berutti E, Bianchi SD. Vestibular surgical access to the palatine root of the superior first molar: “low-dose cone-beam” CT analysis of the pathway and its anatomic variations. J Endod. 2003; 29:773–775. PMID: 14651289.
Article39. Rabiee H, McDonald NJ, Jacobs R, Aminlari A, Inglehart MR. Endodontics program directors’, residents’, and endodontists’ considerations about CBCT-related graduate education. J Dent Educ. 2018; 82:989–999. PMID: 30173196.
Article40. Kalender A, Aksoy U, Basmaci F, Orhan K, Orhan AI. Cone-beam computed tomography analysis of the vestibular surgical pathway to the palatine root of the maxillary first molar. Eur J Dent. 2013; 7:35–40. PMID: 23408714.
Article41. Kim SY, Kim BS, Woo J, Kim Y. Morphology of mandibular first molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals. J Endod. 2013; 39:1516–1521. PMID: 24238439.
Article42. American Association of Endodontists. American Acadamey of Oral and Maxillofacial Radiography. AAE and AAOMR joint position statement. Use of cone-beam-computed tomography in endodontics. Pa Dent J (Harrisb). 2011; 78:37–39.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Assessment of the relationship between the maxillary molars and adjacent structures using cone beam computed tomography
- Positional relationship between the maxillary sinus floor and the apex of the maxillary first molar using cone beam computed tomograph
- Comparison of panoramic radiography and cone beam computed tomography for assessing the relationship between the maxillary sinus floor and maxillary molars
- Expansile dentigerous cyst invading the entire maxillary sinus: a case report
- Consideration of maxillary sinus bone thickness when installing miniscrews