J Korean Med Sci.
2023 Nov;38(45):e383. 10.3346/jkms.2023.38.e383.
Sex-Based Outcomes of P2Y12 Inhibitor Monotherapy After Three Months of Dual Antiplatelet Therapy in Patients Undergoing Percutaneous Coronary Intervention
- Affiliations
-
- 1Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Division of Cardiology, Department of Internal Medicine, Kangwon National University College of Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 3Division of Cardiology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2547984
- DOI: http://doi.org/10.3346/jkms.2023.38.e383
Abstract
- Background
In patients undergoing percutaneous coronary intervention (PCI) in the SMART-CHOICE trial, P2Y12 inhibitor monotherapy after three months of dual antiplatelet therapy (DAPT) achieved clinical outcomes comparable to those of 12 months of DAPT. Nonetheless, the effects of sex on these outcomes remain unknown.
Methods
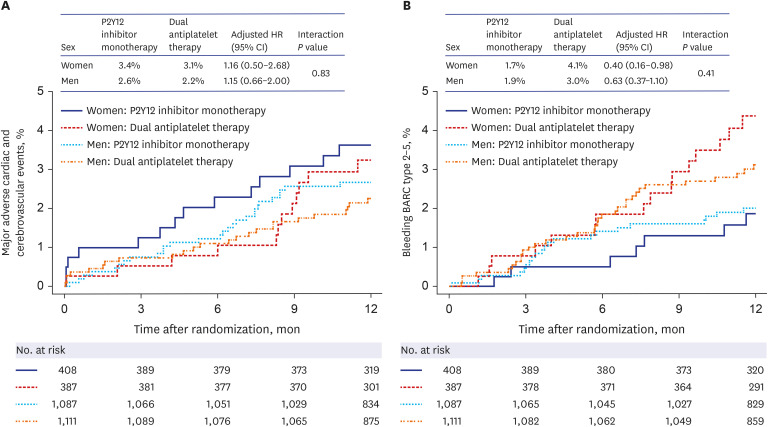
This open-label, non-inferiority, randomized study, conducted in 33 hospitals in South Korea, included 2,993 patients undergoing PCI with drug-eluting stents. Patients were randomly assigned to receive DAPT (aspirin plus a P2Y12 inhibitor) for three months then P2Y12 inhibitor alone for nine months, or DAPT for the entire 12 months. The primary endpoints were major adverse cardiac and cerebrovascular events (a composite of all-cause death, myocardial infarction, or stroke) 12 months after the index procedure. The bleeding endpoints were Bleeding Academic Research Consortium (BARC) bleeding types 2 to 5.
Results
Of the patients, 795 (26.6%) were women, who were older and had a higher prevalence of hypertension, diabetes, and dyslipidemia than men. The sexes exhibited comparable primary endpoints (adjusted hazard ratio [HR], 0.93; 95% confidence interval [CI], 0.55–1.55; P = 0.770) and bleeding endpoints (adjusted HR, 1.07; 95% CI, 0.63–1.81; P = 0.811). P2Y12 inhibitor monotherapy vs DAPT was associated with lower risk of BARC type 2 to 5 bleeding in women (adjusted HR, 0.40; 95% CI, 0.16–0.98; P = 0.045) but the difference was not statistically significant when using the Bonferroni correction. The primary endpoints were similar between treatment groups in both sexes.
Conclusion
In both sexes undergoing PCI, P2Y12 inhibitor monotherapy after three months of DAPT achieved similar risks of the primary endpoints and the bleeding events compared with prolonged DAPT. Therefore, the benefits of early aspirin withdrawal with ongoing P2Y12 inhibitors may be comparable in women and men.
Keyword
Figure
Reference
-
1. Levine GN, Bates ER, Bittl JA, Brindis RG, Fihn SD, Fleisher LA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2016; 152(5):1243–1275. PMID: 27751237.2. Capodanno D, Alfonso F, Levine GN, Valgimigli M, Angiolillo DJ. ACC/AHA versus ESC guidelines on dual antiplatelet therapy: JACC guideline comparison. J Am Coll Cardiol. 2018; 72(23 Pt A):2915–2931. PMID: 30522654.3. Mehran R, Pocock SJ, Stone GW, Clayton TC, Dangas GD, Feit F, et al. Associations of major bleeding and myocardial infarction with the incidence and timing of mortality in patients presenting with non-ST-elevation acute coronary syndromes: a risk model from the ACUITY trial. Eur Heart J. 2009; 30(12):1457–1466. PMID: 19351691.
Article4. Ndrepepa G, Schuster T, Hadamitzky M, Byrne RA, Mehilli J, Neumann FJ, et al. Validation of the Bleeding Academic Research Consortium definition of bleeding in patients with coronary artery disease undergoing percutaneous coronary intervention. Circulation. 2012; 125(11):1424–1431. PMID: 22344040.
Article5. Giustino G, Baber U, Sartori S, Mehran R, Mastoris I, Kini AS, et al. Duration of dual antiplatelet therapy after drug-eluting stent implantation: a systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2015; 65(13):1298–1310. PMID: 25681754.
Article6. Palmerini T, Benedetto U, Bacchi-Reggiani L, Della Riva D, Biondi-Zoccai G, Feres F, et al. Mortality in patients treated with extended duration dual antiplatelet therapy after drug-eluting stent implantation: a pairwise and Bayesian network meta-analysis of randomised trials. Lancet. 2015; 385(9985):2371–2382. PMID: 25777667.
Article7. Palmerini T, Benedetto U, Biondi-Zoccai G, Della Riva D, Bacchi-Reggiani L, Smits PC, et al. Long-term safety of drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. J Am Coll Cardiol. 2015; 65(23):2496–2507. PMID: 26065988.8. Hahn JY, Song YB, Oh JH, Chun WJ, Park YH, Jang WJ, et al. Effect of P2Y12 inhibitor monotherapy vs dual antiplatelet therapy on cardiovascular events in patients undergoing percutaneous coronary intervention: the SMART-CHOICE randomized clinical trial. JAMA. 2019; 321(24):2428–2437. PMID: 31237645.
Article9. Mehran R, Chandrasekhar J, Urban P, Lang IM, Windhoevel U, Spaulding C, et al. Sex-based outcomes in patients with a high bleeding risk after percutaneous coronary intervention and 1-month dual antiplatelet therapy: a secondary analysis of the LEADERS FREE randomized clinical trial. JAMA Cardiol. 2020; 5(8):939–947. PMID: 32432718.
Article10. Chichareon P, Modolo R, Kerkmeijer L, Tomaniak M, Kogame N, Takahashi K, et al. Association of sex with outcomes in patients undergoing percutaneous coronary intervention: a subgroup analysis of the GLOBAL LEADERS randomized clinical trial. JAMA Cardiol. 2020; 5(1):21–29. PMID: 31693078.
Article11. Vogel B, Baber U, Cohen DJ, Sartori S, Sharma SK, Angiolillo DJ, et al. Sex differences among patients with high risk receiving ticagrelor with or without aspirin after percutaneous coronary intervention: a subgroup analysis of the TWILIGHT randomized clinical trial. JAMA Cardiol. 2021; 6(9):1032–1041. PMID: 33991416.
Article12. Song YB, Oh SK, Oh JH, Im ES, Cho DK, Cho BR, et al. Rationale and design of the comparison between a P2Y12 inhibitor monotherapy versus dual antiplatelet therapy in patients undergoing implantation of coronary drug-eluting stents (SMART-CHOICE): A prospective multicenter randomized trial. Am Heart J. 2018; 197:77–84. PMID: 29447787.
Article13. Yu J, Mehran R, Grinfeld L, Xu K, Nikolsky E, Brodie BR, et al. Sex-based differences in bleeding and long term adverse events after percutaneous coronary intervention for acute myocardial infarction: three year results from the HORIZONS-AMI trial. Catheter Cardiovasc Interv. 2015; 85(3):359–368. PMID: 25115966.
Article14. Spirito A, Gragnano F, Corpataux N, Vaisnora L, Galea R, Svab S, et al. Sex-based differences in bleeding risk after percutaneous coronary intervention and implications for the academic research consortium high bleeding risk criteria. J Am Heart Assoc. 2021; 10(12):e021965. PMID: 34098740.
Article15. Hess CN, McCoy LA, Duggirala HJ, Tavris DR, O’Callaghan K, Douglas PS, et al. Sex-based differences in outcomes after percutaneous coronary intervention for acute myocardial infarction: a report from TRANSLATE-ACS. J Am Heart Assoc. 2014; 3(1):e000523. PMID: 24510115.
Article16. Anderson ML, Peterson ED, Brennan JM, Rao SV, Dai D, Anstrom KJ, et al. Short- and long-term outcomes of coronary stenting in women versus men: results from the National Cardiovascular Data Registry Centers for Medicare & Medicaid services cohort. Circulation. 2012; 126(18):2190–2199. PMID: 22988009.
Article17. Husted S, James SK, Bach RG, Becker RC, Budaj A, Heras M, et al. The efficacy of ticagrelor is maintained in women with acute coronary syndromes participating in the prospective, randomized, PLATelet inhibition and patient Outcomes (PLATO) trial. Eur Heart J. 2014; 35(23):1541–1550. PMID: 24682844.
Article18. Chandiramani R, Cao D, Claessen BE, Sorrentino S, Guedeney P, Blum M, et al. Sex-related differences in patients at high bleeding risk undergoing percutaneous coronary intervention: a patient-level pooled analysis from 4 postapproval studies. J Am Heart Assoc. 2020; 9(7):e014611. PMID: 32223396.
Article19. Shin ES, Lee CW, Ahn JM, Lee PH, Chang M, Kim MJ, et al. Sex differences in left main coronary artery stenting: Different characteristics but similar outcomes for women compared with men. Int J Cardiol. 2018; 253:50–54. PMID: 29306470.
Article20. Shin ES, Jun EJ, Han JK, Kong MG, Kang J, Zheng C, et al. Sex-related impact on clinical outcomes of patients treated with drug-eluting stents according to clinical presentation: Patient-level pooled analysis from the GRAND-DES registry. Cardiol J. 2023; 30(1):105–116. PMID: 33634845.
Article21. Lee SH, Choi J, Chang YJ, Shin ES, Choi KH, Lee JM, et al. Sex difference in long-term clinical outcomes after percutaneous coronary intervention: a propensity-matched analysis of National Health Insurance data in Republic of Korea. Catheter Cardiovasc Interv. 2021; 98(2):E171–E180. PMID: 33547718.
Article22. Schreuder MM, Badal R, Boersma E, Kavousi M, Roos-Hesselink J, Versmissen J, et al. Efficacy and safety of high potent P2Y12 inhibitors prasugrel and ticagrelor in patients with coronary heart disease treated with dual antiplatelet therapy: a sex-specific systematic review and meta-analysis. J Am Heart Assoc. 2020; 9(4):e014457. PMID: 32063118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- De-escalation strategies of dual antiplatelet therapy in patients undergoing percutaneous coronary intervention for acute coronary syndrome
- Dual Antiplatelet Therapy after Noncardioembolic Ischemic Stroke or Transient Ischemic Attack: Pros and Cons
- The Evolving Concept of Dual Antiplatelet Therapy after Percutaneous Coronary Intervention: Focus on Unique Feature of East Asian and “Asian Paradoxâ€
- Perioperative management for patients undergoing noncardiac surgery after percutaneous coronary intervention
- The Role of Novel Oral Anticoagulants and Antiplatelet Therapy after Percutaneous Coronary Intervention: Individualizing Therapy to Optimize Outcomes