Clin Endosc.
2023 Nov;56(6):817-822. 10.5946/ce.2023.071.
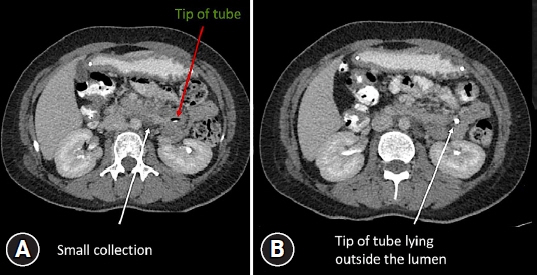
Nasojejunal tube-related duodenal perforations: a multicenter experience
- Affiliations
-
- 1Department of Gastroenterology and Advanced Endoscopy, Ansh Clinic, Ahmedabad, Gujarat, India
- 2Department of Gastroenterology and Advanced Endoscopy, Prime Hospital, Rajkot, Gujarat, India
- 3Department of Gastroenterology and Advanced Endoscopy, Mission Gastro Hospital, Ahmedabad, Gujarat, India
- 4Department of Gastroenterology and Endoscopy, Gujarat Gastro Hub, Mehsana, India
- KMID: 2547905
- DOI: http://doi.org/10.5946/ce.2023.071
Figure
Reference
-
1. Pearce CB, Duncan HD. Enteral feeding. Nasogastric, nasojejunal, percutaneous endoscopic gastrostomy, or jejunostomy: its indications and limitations. Postgrad Med J. 2002; 78:198–204.
Article2. Sajid MS, Harper A, Hussain Q, et al. An integrated systematic review and meta-analysis of published randomized controlled trials evaluating nasogastric against postpyloris (nasoduodenal and nasojejunal) feeding in critically ill patients admitted in intensive care unit. Eur J Clin Nutr. 2014; 68:424–432.
Article3. Blumenstein I, Shastri YM, Stein J. Gastroenteric tube feeding: techniques, problems and solutions. World J Gastroenterol. 2014; 20:8505–8524.
Article4. Halkic N, Guerid S, Blanchard A, et al. Small-bowel perforation: a consequence of feeding jejunostomy. Can J Surg. 2005; 48:161–162.5. Fang JC, Hilden K, Holubkov R, et al. Transnasal endoscopy vs. fluoroscopy for the placement of nasoenteric feeding tubes in critically ill patients. Gastrointest Endosc. 2005; 62:661–666.
Article6. ASGE Technology Committee, Kwon RS, Banerjee S, et al. Enteral nutrition access devices. Gastrointest Endosc. 2010; 72:236–248.
Article7. Schwab D, Mühldorfer S, Nusko G, et al. Endoscopic placement of nasojejunal tubes: a randomized, controlled, prospective trial comparing suitability and technical success for two different tubes. Gastrointest Endosc. 2002; 56:858–863.
Article8. Prabhakaran S, Doraiswamy VA, Nagaraja V, et al. Nasoenteric tube complications. Scand J Surg. 2012; 101:147–155.
Article9. Siegle RL, Rabinowitz JG, Sarasohn C. Intestinal perforations secondary to nasojejunal feeding tubes. AJR Am J Roentgenol. 1976; 126:1229–1232.
Article10. Merten DF, Mumford L, Filston HC, et al. Radiological observations during transpyloric tube feeding in infants of low birth weight. Perforation of the duodenum and variations in normal duodenal anatomy. Radiology. 1980; 136:67–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation
- Two Cases of Successful ERCP during ERCP-Related Iatrogenic Duodenal Perforation
- Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
- Perforation on the superior side of duodenum is a risk factor of laparoscopic primary repair for duodenal ulcer perforation
- A Case of Type I Duodenal Perforation Treated with Covered Metal Stent