Clin Endosc.
2014 Jul;47(4):341-345. 10.5946/ce.2014.47.4.341.
The Management of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforation
- Affiliations
-
- 1Division of Gastroenterology and Hepatology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea. chokb@dsmc.or.kr
- KMID: 1907935
- DOI: http://doi.org/10.5946/ce.2014.47.4.341
Abstract
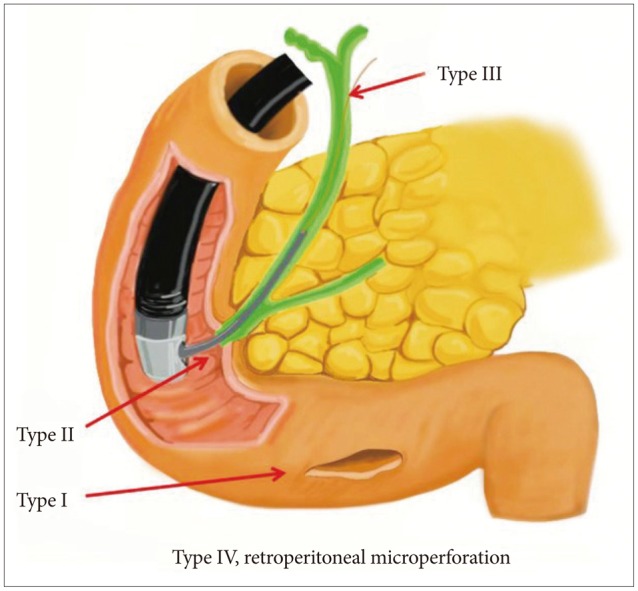
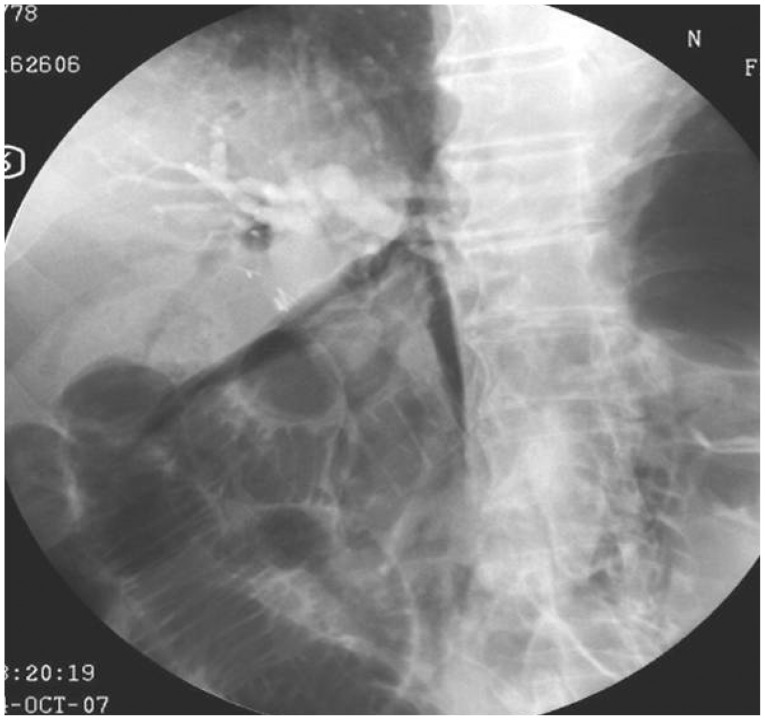
- Uneventful duodenal perforation during endoscopic retrograde cholangiopancreatography (ERCP) is an uncommon but occasionally fatal complication. ERCP-related perforations may occur during sphincterotomy and improper manipulation of the equipment and scope. Traditionally, duodenal perforation has been treated with early surgical repair. Recently, nonoperative early endoscopic management techniques including clips or fibrin glue have been reported. In the present paper we review the literature pertaining to the treatment of perforations.
MeSH Terms
Figure
Cited by 2 articles
-
Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
Seon Mee Park
Clin Endosc. 2016;49(4):376-382. doi: 10.5946/ce.2016.088.Highlights from the 50th Seminar of the Korean Society of Gastrointestinal Endoscopy
Eun Young Kim, Il Ju Choi, Kwang An Kwon, Ji Kon Ryu, Seok Ho Dong, Ki Baik Hahm
Clin Endosc. 2014;47(4):285-294. doi: 10.5946/ce.2014.47.4.285.
Reference
-
1. Cotton PB, Lehman G, Vennes J, et al. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991; 37:383–393. PMID: 2070995.
Article2. Freeman ML, DiSario JA, Nelson DB, et al. Risk factors for post-ERCP pancreatitis: a prospective, multicenter study. Gastrointest Endosc. 2001; 54:425–434. PMID: 11577302.
Article3. Loperfido S, Angelini G, Benedetti G, et al. Major early complications from diagnostic and therapeutic ERCP: a prospective multicenter study. Gastrointest Endosc. 1998; 48:1–10. PMID: 9684657.
Article4. Williams EJ, Taylor S, Fairclough P, et al. Risk factors for complication following ERCP: results of a large-scale, prospective multicenter study. Endoscopy. 2007; 39:793–801. PMID: 17703388.
Article5. Howard TJ, Tan T, Lehman GA, et al. Classification and management of perforations complicating endoscopic sphincterotomy. Surgery. 1999; 126:658–663. PMID: 10520912.
Article6. Stapfer M, Selby RR, Stain SC, et al. Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg. 2000; 232:191–198. PMID: 10903596.
Article7. Freeman ML, Nelson DB, Sherman S, et al. Complications of endoscopic biliary sphincterotomy. N Engl J Med. 1996; 335:909–918. PMID: 8782497.
Article8. Nakagawa Y, Nagai T, Soma W, et al. Endoscopic closure of a large ERCP-related lateral duodenal perforation by using endoloops and endoclips. Gastrointest Endosc. 2010; 72:216–217. PMID: 20304402.
Article9. Lee TH, Han JH, Park SH. Endoscopic treatments of endoscopic retrograde cholangiopancreatography-related duodenal perforations. Clin Endosc. 2013; 46:522–528. PMID: 24143315.
Article10. Park WY, Cho KB, Kim ES, Park KS. A case of ampullary perforation treated with a temporally covered metal stent. Clin Endosc. 2012; 45:177–180. PMID: 22866262.
Article11. Vezakis A, Fragulidis G, Nastos C, Yiallourou A, Polydorou A, Voros D. Closure of a persistent sphincterotomy-related duodenal perforation by placement of a covered self-expandable metallic biliary stent. World J Gastroenterol. 2011; 17:4539–4541. PMID: 22110286.
Article12. Enns R, Eloubeidi MA, Mergener K, et al. ERCP-related perforations: risk factors and management. Endoscopy. 2002; 34:293–298. PMID: 11932784.
Article13. Cheng CL, Sherman S, Watkins JL, et al. Risk factors for post-ERCP pancreatitis: a prospective multicenter study. Am J Gastroenterol. 2006; 101:139–147. PMID: 16405547.
Article14. Wang P, Li ZS, Liu F, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. 2009; 104:31–40. PMID: 19098846.
Article15. Wu HM, Dixon E, May GR, Sutherland FR. Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford). 2006; 8:393–399. PMID: 18333093.
Article16. Li G, Chen Y, Zhou X, Lv N. Early management experience of perforation after ERCP. Gastroenterol Res Pract. 2012; 2012:657418. PMID: 22899906.
Article17. Genzlinger JL, McPhee MS, Fisher JK, Jacob KM, Helzberg JH. Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am J Gastroenterol. 1999; 94:1267–1270. PMID: 10235205.
Article18. Zissin R, Shapiro-Feinberg M, Oscadchy A, Pomeranz I, Leichtmann G, Novis B. Retroperitoneal perforation during endoscopic sphincterotomy: imaging findings. Abdom Imaging. 2000; 25:279–282. PMID: 10823451.
Article19. Fatima J, Baron TH, Topazian MD, et al. Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg. 2007; 142:448–454. PMID: 17515486.20. Masci E, Toti G, Mariani A, et al. Complications of diagnostic and therapeutic ERCP: a prospective multicenter study. Am J Gastroenterol. 2001; 96:417–423. PMID: 11232684.
Article21. Mao Z, Zhu Q, Wu W, et al. Duodenal perforations after endoscopic retrograde cholangiopancreatography: experience and management. J Laparoendosc Adv Surg Tech A. 2008; 18:691–695. PMID: 18803511.
Article22. Baron TH, Gostout CJ, Herman L. Hemoclip repair of a sphincterotomy-induced duodenal perforation. Gastrointest Endosc. 2000; 52:566–568. PMID: 11023583.
Article23. Amodio PM, Faggiani R, Pastorelli A, et al. Selected treatments for duodenal perforation after ERCP. A report of three cases. Chir Ital. 2007; 59:343–346. PMID: 17663374.24. Lee TH, Bang BW, Jeong JI, et al. Primary endoscopic approximation suture under cap-assisted endoscopy of an ERCP-induced duodenal perforation. World J Gastroenterol. 2010; 16:2305–2310. PMID: 20458771.
Article25. Buffoli F, Grassia R, Iiritano E, Bianchi G, Dizioli P, Staiano T. Endoscopic "retroperitoneal fatpexy" of a large ERCP-related jejunal perforation by using a new over-the-scope clip device in Billroth II anatomy (with video). Gastrointest Endosc. 2012; 75:1115–1117. PMID: 21820111.
Article26. Mutignani M, Iacopini F, Dokas S, et al. Successful endoscopic closure of a lateral duodenal perforation at ERCP with fibrin glue. Gastrointest Endosc. 2006; 63:725–727. PMID: 16564890.
Article27. Kim KW, Lee TH, Park SH, et al. A primary repair with hemoclips and fibrin glue injection in biliary stent induced duodenal perforation. Korean J Gastrointest Endosc. 2011; 42:437–441.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Four Cases of Guidewire Induced Periampullary Perforation During Endoscopic Retrograde Cholangiopancreatography
- Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
- Two Cases of Successful ERCP during ERCP-Related Iatrogenic Duodenal Perforation
- Recent Advanced Endoscopic Management of Endoscopic Retrograde Cholangiopancreatography Related Duodenal Perforations
- Repair of an Endoscopic Retrograde Cholangiopancreatography-Related Large Duodenal Perforation Using Double Endoscopic Band Ligation and Endoclipping