Ann Surg Treat Res.
2023 Nov;105(5):271-280. 10.4174/astr.2023.105.5.271.
Multicenter study of prognostic factors in paraaortic lymph node dissection for metastatic colorectal cancer
- Affiliations
-
- 1Department of Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- KMID: 2547532
- DOI: http://doi.org/10.4174/astr.2023.105.5.271
Abstract
- Purpose
The role of paraaortic lymph node dissection (PALND) in colorectal cancer (CRC) has been less evaluated than surgical treatments for other distant metastases. We evaluated surgical outcomes after PALND and identified prognostic factors.
Methods
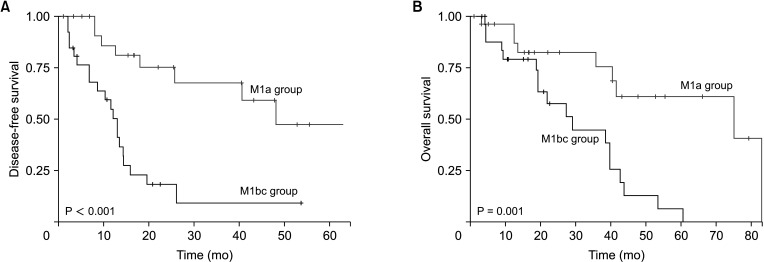
The medical records of patients who underwent PALND for paraaortic lymph node metastasis (PALNM) were reviewed retrospectively. All patients were categorized into the M1a group (isolated PALNM, n = 27), and the M1bc group (distant metastases other than PALNM, n = 26). Three severity factors (PALNM-SF: number of harvested paraaortic lymph nodes [hLN], ≥14; number of metastatic paraaortic lymph nodes [mLN], ≥5; and lymph nodes ratio [mLN/hLN], ≥0.5) were defined to determine their effects on survival.
Results
The 5-year overall survival (OS) of the M1a and M1bc groups were 61.1% and 6.4%, respectively (P = 0.0013). The 5-year disease-free survival (DFS) of the M1a group was 47.4%, and the 3-year DFS of the M1bc group was 9.1% (P < 0.001). Patients with 2 or more PALNM-SFs showed worse OS than those with 1 PALNM-SF (P = 0.017). In multivariate analysis, M1bc (non-isolated PALNM) was the only significant factor for survival. In the M1a group, patients with 2 or more PALNMSFs showed significantly worse survival than those with a single PALNM-SF. In multivariate analysis, 2 or more PALNM-SF was a significant factor for survival.
Conclusion
PALND for CRC provided favorable outcomes in the survival of an isolated PALNM, although this was uncertain for non-isolated PALNMs. The PALNM-SFs helped assess the prognosis after PALND.
Keyword
Figure
Reference
-
1. Hu CY, Bailey CE, You YN, Skibber JM, Rodriguez-Bigas MA, Feig BW, et al. Time trend analysis of primary tumor resection for stage IV colorectal cancer: less surgery, improved survival. JAMA Surg. 2015; 150:245–251. PMID: 25588105.
Article2. Jawed I, Wilkerson J, Prasad V, Duffy AG, Fojo T. Colorectal cancer survival gains and novel treatment regimens: a systematic review and analysis. JAMA Oncol. 2015; 1:787–795. PMID: 26181239.
Article3. Lee RM, Cardona K, Russell MC. Historical perspective: two decades of progress in treating metastatic colorectal cancer. J Surg Oncol. 2019; 119:549–563. PMID: 30806493.
Article4. Min BS, Kim NK, Sohn SK, Cho CH, Lee KY, Baik SH. Isolated paraaortic lymph-node recurrence after the curative resection of colorectal carcinoma. J Surg Oncol. 2008; 97:136–140. PMID: 17963247.
Article5. Gagnière J, Dupré A, Chabaud S, Peyrat P, Meeus P, Rivoire M. Retroperitoneal nodal metastases from colorectal cancer: curable metastases with radical retroperitoneal lymphadenectomy in selected patients. Eur J Surg Oncol. 2015; 41:731–737. PMID: 25899983.
Article6. Wong JS, Tan GH, Teo MC. Management of para-aortic lymph node metastasis in colorectal patients: a systemic review. Surg Oncol. 2016; 25:411–418. PMID: 27916174.
Article7. Song SH, Park SY, Park JS, Kim HJ, Yang CS, Choi GS. Laparoscopic para-aortic lymph node dissection for patients with primary colorectal cancer and clinically suspected para-aortic lymph nodes. Ann Surg Treat Res. 2016; 90:29–35. PMID: 26793690.
Article8. Lee J, Park HM, Lee SY, Kim CH, Kim HR. Prognostic significance of enlarged paraaortic lymph nodes detected during left-sided colorectal cancer surgery: a single-center retrospective cohort study. World J Surg Oncol. 2021; 19:9. PMID: 33430884.
Article9. Choi PW, Kim HC, Kim AY, Jung SH, Yu CS, Kim JC. Extensive lymphadenectomy in colorectal cancer with isolated para-aortic lymph node metastasis below the level of renal vessels. J Surg Oncol. 2010; 101:66–71. PMID: 19842140.
Article10. Bae SU, Hur H, Min BS, Baik SH, Lee KY, Kim NK. Which patients with isolated para-aortic lymph node metastasis will truly benefit from extended lymph node dissection for colon cancer? Cancer Res Treat. 2018; 50:712–719. PMID: 28707461.
Article11. Zizzo M, Dorma MP, Zanelli M, Sanguedolce F, Bassi MC, Palicelli A, et al. Long-term outcomes of surgical resection of pathologically confirmed isolated para-aortic lymph node metastases in colorectal cancer: a systematic review. Cancers (Basel). 2022; 14:661. PMID: 35158930.
Article12. Kim HJ, Choi GS. Clinical implications of lymph node metastasis in colorectal cancer: current status and future perspectives. Ann Coloproctol. 2019; 35:109–117. PMID: 31288500.
Article13. Ceelen W, Van Nieuwenhove Y, Pattyn P. Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review. Ann Surg Oncol. 2010; 17:2847–2855. PMID: 20559741.
Article14. Nakai N, Yamaguchi T, Kinugasa Y, Shiomi A, Kagawa H, Yamakawa Y, et al. Long-term outcomes after resection of para-aortic lymph node metastasis from left-sided colon and rectal cancer. Int J Colorectal Dis. 2017; 32:999–1007. PMID: 28382511.
Article15. Ushigome H, Yasui M, Ohue M, Haraguchi N, Nishimura J, Sugimura K, et al. The treatment strategy of R0 resection in colorectal cancer with synchronous para-aortic lymph node metastasis. World J Surg Oncol. 2020; 18:229. PMID: 32859208.
Article16. Yamada K, Tsukamoto S, Ochiai H, Shida D, Kanemitsu Y. Improving selection for resection of synchronous para-aortic lymph node metastases in colorectal cancer. Dig Surg. 2019; 36:369–375. PMID: 30045044.
Article17. Albandar MH, Cho MS, Bae SU, Kim NK. Surgical management of extra-regional lymph node metastasis in colorectal cancer. Expert Rev Anticancer Ther. 2016; 16:503–513. PMID: 26950286.
Article18. Park J, Lee SD, Han SS, Kim SH, Park SJ, Oh JH, et al. Repeat hepatectomy for recurred colorectal liver metastasis: is it justified? Ann Surg Treat Res. 2019; 97:7–14. PMID: 31297347.
Article19. Guo M, Jin N, Pawlik T, Cloyd JM. Neoadjuvant chemotherapy for colorectal liver metastases: a contemporary review of the literature. World J Gastrointest Oncol. 2021; 13:1043–1061. PMID: 34616511.
Article20. Engstrand J, Strömberg C, Nilsson H, Freedman J, Jonas E. Synchronous and metachronous liver metastases in patients with colorectal cancer-towards a clinically relevant definition. World J Surg Oncol. 2019; 17:228. PMID: 31878952.
Article21. Arimoto A, Uehara K, Kato T, Nakamura H, Kamiya T, Nagino M. Clinical significance of para-aortic lymph node dissection for advanced or metastatic colorectal cancer in the current era of modern chemotherapy. Dig Surg. 2015; 32:439–444. PMID: 26402333.
Article22. Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT, et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010; 11:38–47. PMID: 19942479.
Article23. Primrose J, Falk S, Finch-Jones M, Valle J, O'Reilly D, Siriwardena A, et al. Systemic chemotherapy with or without cetuximab in patients with resectable colorectal liver metastasis: the New EPOC randomised controlled trial. Lancet Oncol. 2014; 15:601–611. PMID: 24717919.
Article24. Miyazawa T, Ebe K, Koide N, Fujita N. Complete response of isolated para-aortic lymph node recurrence from rectosigmoid cancer treated by chemoradiation therapy with capecitabine/oxaliplatin plus bevacizumab: a case report. Case Rep Oncol. 2012; 5:216–221. PMID: 22679426.
Article25. Yasuda S, Kamata H, Machida T, Okada K, Tanaka A, Suzuki T, et al. A case of isolated paraaortic lymph node recurrence from colon cancer successfully treated with chemoradiotherapy. Tokai J Exp Clin Med. 2012; 37:47–50. PMID: 22763827.26. Kasi A, Abbasi S, Handa S, Al-Rajabi R, Saeed A, Baranda J, et al. Total neoadjuvant therapy vs standard therapy in locally advanced rectal cancer: a systematic review and meta-analysis. JAMA Netw Open. 2020; 3:e2030097. PMID: 33326026.27. Sun Y, Xu Z, Yu L, Lin H, Huang Y, Chi P. Indocyanine green f luorescence imaging guided laparoscopic para-aortic lymphadenectomy for rectal cancer with para-aortic lymph node metastasis-a video vignette. Colorectal Dis. 2023; 25:340–341. PMID: 36050596.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Implications of Lymph Node Metastasis in Colorectal Cancer: Current Status and Future Perspectives
- Prognostic value of the lymph node metastasis in patients with ampulla of Vater cancer after surgical resection
- Laparoscopic para-aortic lymph node dissection for patients with primary colorectal cancer and clinically suspected para-aortic lymph nodes
- Prognostic Factors for Serosal Invasive Gastric Cancer: Clinical Significance of Metastatic Lymph Node Ratio
- Minimally Invasive Surgery Based on Sentinel Node Biopsy for Gastrointestinal Cancer