Ann Surg Treat Res.
2016 Jan;90(1):29-35. 10.4174/astr.2016.90.1.29.
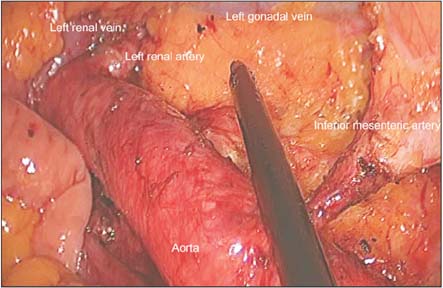
Laparoscopic para-aortic lymph node dissection for patients with primary colorectal cancer and clinically suspected para-aortic lymph nodes
- Affiliations
-
- 1Colorectal Cancer Center, Kyungpook National University Medical Center, Kyungpook National University School of Medicine, Daegu, Korea. kyuschoi@mail.knu.ac.kr
- KMID: 2149929
- DOI: http://doi.org/10.4174/astr.2016.90.1.29
Abstract
- PURPOSE
Treatment of patients with para-aortic lymph node metastasis from colorectal cancer is controversial. The goal of this study was to investigate the technical feasibility of laparoscopic intrarenal para-aortic lymph node dissection in patients with colorectal cancer and clinically suspected para-aortic lymph node dissection.
METHODS
The inclusion criteria for the laparoscopic approach were patients with infrarenal para-aortic lymph node metastasis from colorectal cancer. Patients who had any other distant metastatic lesion or metachronous para-aortic lymph node metastasis were excluded from this study. Perioperative outcomes and survival outcomes were analyzed.
RESULTS
Between November 2004 and October 2013, 40 patients underwent laparoscopic para-aortic lymph node dissection. The mean operating time was 192.3 +/- 68.8 minutes (range, 100-400 minutes) and the mean estimated blood loss was 65.6 +/- 52.6 mL (range, 20-210 mL). No patient required open conversion. The postoperative complication rate was 15.0%. Sixteen patients (40.0%) had pathologically positive lymph nodes. In patients with metastatic para-aortic lymph nodes, the 3-year overall survival rate and disease-free survival rate were 65.7% and 40.2%, respectively.
CONCLUSION
The results of our study suggest that a laparoscopic approach for patients with colorectal cancer with metastatic para-aortic lymph nodes can be a reasonable option for selected patients.
MeSH Terms
Figure
Cited by 1 articles
-
Multicenter study of prognostic factors in paraaortic lymph node dissection for metastatic colorectal cancer
Jun Woo Bong, Sanghee Kang, Pyoungjae Park
Ann Surg Treat Res. 2023;105(5):271-280. doi: 10.4174/astr.2023.105.5.271.
Reference
-
1. Fleshman J, Sargent DJ, Green E, Anvari M, Stryker SJ, Beart RW Jr, et al. Laparoscopic colectomy for cancer is not inferior to open surgery based on 5-year data from the COST Study Group trial. Ann Surg. 2007; 246:655–662.2. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52.3. Marks J, Mizrahi B, Dalane S, Nweze I, Marks G. Laparoscopic transanal abdominal transanal resection with sphincter preservation for rectal cancer in the distal 3 cm of the rectum after neoadjuvant therapy. Surg Endosc. 2010; 24:2700–2707.4. Park JS, Choi GS, Jun SH, Hasegawa S, Sakai Y. Laparoscopic versus open intersphincteric resection and coloanal anastomosis for low rectal cancer: intermediateterm oncologic outcomes. Ann Surg. 2011; 254:941–946.5. Park JS, Choi GS, Lim KH, Jang YS, Kim HJ, Park SY, et al. Laparoscopic extended lateral pelvic node dissection following total mesorectal excision for advanced rectal cancer: initial clinical experience. Surg Endosc. 2011; 25:3322–3329.6. Liang JT. Technical feasibility of laparoscopic lateral pelvic lymph node dissection for patients with low rectal cancer after concurrent chemoradiation therapy. Ann Surg Oncol. 2011; 18:153–159.7. Edge SB, Byrd DR, Compton CC, Fritz AG, Greene FL, Trotti A, editors. AJCC cancer staging manual. 7th ed. New York: Springer;2010.8. Howlader N, Noone AM, Krapcho M, Garshell J, Miller D, Altekruse SF, et al. SEER Cancer Statistics Review, 1975-2012 [Internet]. Bethesda (MD): National Cancer Institute;2014. cited 2015 Apr 30. Available from: http://seer.cancer.gov/csr/1975_2012/.9. Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015; 47:127–141.10. Mahmoud N, Bullard Dunn K. Metastasectomy for stage IV colorectal cancer. Dis Colon Rectum. 2010; 53:1080–1092.11. Khattak MA, Martin HL, Beeke C, Price T, Carruthers S, Kim S, et al. Survival differences in patients with metastatic colorectal cancer and with single site metastatic disease at initial presentation: results from South Australian clinical registry for advanced colorectal cancer. Clin Colorectal Cancer. 2012; 11:247–254.12. Gagniere J, Dupre A, Chabaud S, Peyrat P, Meeus P, Rivoire M. Retroperitoneal nodal metastases from colorectal cancer: curable metastases with radical retroperitoneal lymphadenectomy in selected patients. Eur J Surg Oncol. 2015; 41:731–737.13. Choi PW, Kim HC, Kim AY, Jung SH, Yu CS, Kim JC. Extensive lymphadenectomy in colorectal cancer with isolated paraaortic lymph node metastasis below the level of renal vessels. J Surg Oncol. 2010; 101:66–71.14. Min BS, Kim NK, Sohn SK, Cho CH, Lee KY, Baik SH. Isolated paraaortic lymphnode recurrence after the curative resection of colorectal carcinoma. J Surg Oncol. 2008; 97:136–140.15. Shibata D, Paty PB, Guillem JG, Wong WD, Cohen AM. Surgical management of isolated retroperitoneal recurrences of colorectal carcinoma. Dis Colon Rectum. 2002; 45:795–801.16. Liang JT, Huang KC, Lai HS, Lee PH, Sun CT. Oncologic results of laparoscopic D3 lymphadenectomy for male sigmoid and upper rectal cancer with clinically positive lymph nodes. Ann Surg Oncol. 2007; 14:1980–1990.17. Liang JT. Surgical techniques of laparoscopic peritonectomy plus paraaortic lymph node dissection for the treatment of patients with positive lymph node metastasis and peritoneal seeding from rectosigmoid cancer. Surg Endosc. 2012; 26:2383–2387.18. Liang JT, Lai HS, Wu CT, Huang KC, Lee PH, Shun CT. Laparoscopic prophylactic oophorectomy plus N3 lymphadenectomy for advanced rectosigmoid cancer. Ann Surg Oncol. 2007; 14:1991–1999.19. Dumont F, Kothodinis K, Goere D, Honore C, Dartigues P, Boige V, et al. Central retroperitoneal recurrences from colorectal cancer: are lymph node and locoregional recurrences the same disease? Eur J Surg Oncol. 2012; 38:611–616.20. Yeo SG, Kim DY, Kim TH, Jung KH, Hong YS, Kim SY, et al. Curative chemoradiotherapy for isolated retroperitoneal lymph node recurrence of colorectal cancer. Radiother Oncol. 2010; 97:307–311.21. Lee J, Chang JS, Shin SJ, Lim JS, Keum KC, Kim NK, et al. Incorporation of radiotherapy in the multidisciplinary treatment of isolated retroperitoneal lymph node recurrence from colorectal cancer. Ann Surg Oncol. 2015; 22:1520–1526.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Para-aortic Lymph Node Dissection in Patients with Gynecologic Malignancy
- Para-aortic Lymph Node Dissection in Gastric Cancer
- Prognosis of the Patients Showing Metastasis to the Para-aortic or/and Supraclavicular Lymph Nodes at the Time of Diagnosis of Recurrence of the Cervical Cancer
- Laparoscopic pelvic and para-aortic lymphadenectomy
- Surgical technique of two-step pelvic and para-aortic sentinel lymph node mapping in early-stage endometrial cancer: laparoscopic, robotic, and open method