J Korean Neurosurg Soc.
2023 Nov;66(6):703-715. 10.3340/jkns.2023.0071.
Factors Affecting Cage Obliquity and the Relationship between Cage Obliquity and Radiological Outcomes in Oblique Lateral Interbody Fusion at the L4-L5 Level
- Affiliations
-
- 1Department of Neurosurgery, The Armed Forces Capital Hospital, Seongnam, Korea
- KMID: 2547464
- DOI: http://doi.org/10.3340/jkns.2023.0071
Abstract
Objective
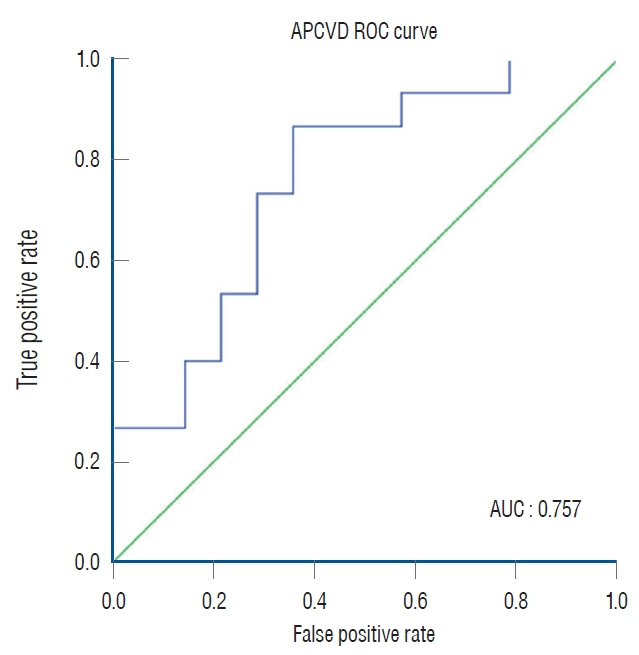
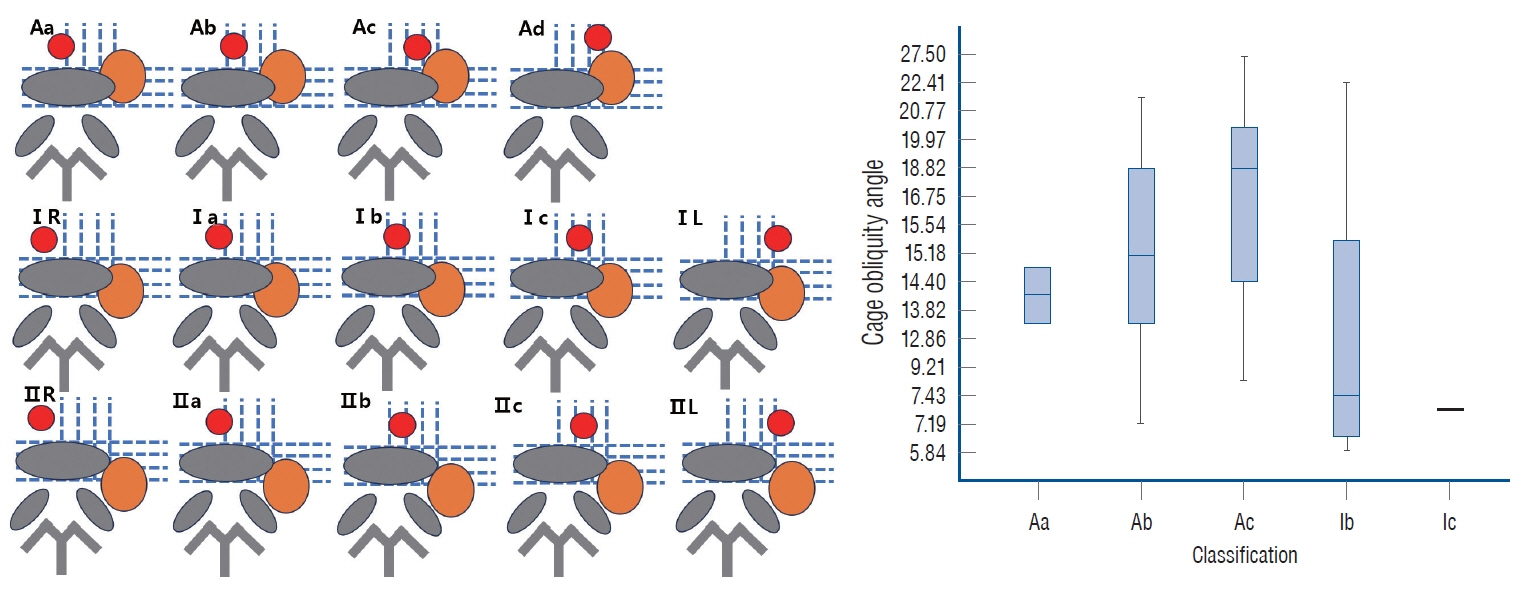
: This retrospective study investigated the factors that affect cage obliquity angle despite orthogonal maneuvers performed during oblique lateral interbody fusion (OLIF) and assessed the relationship between cage obliquity angle and radiological outcomes post-surgery.
Methods
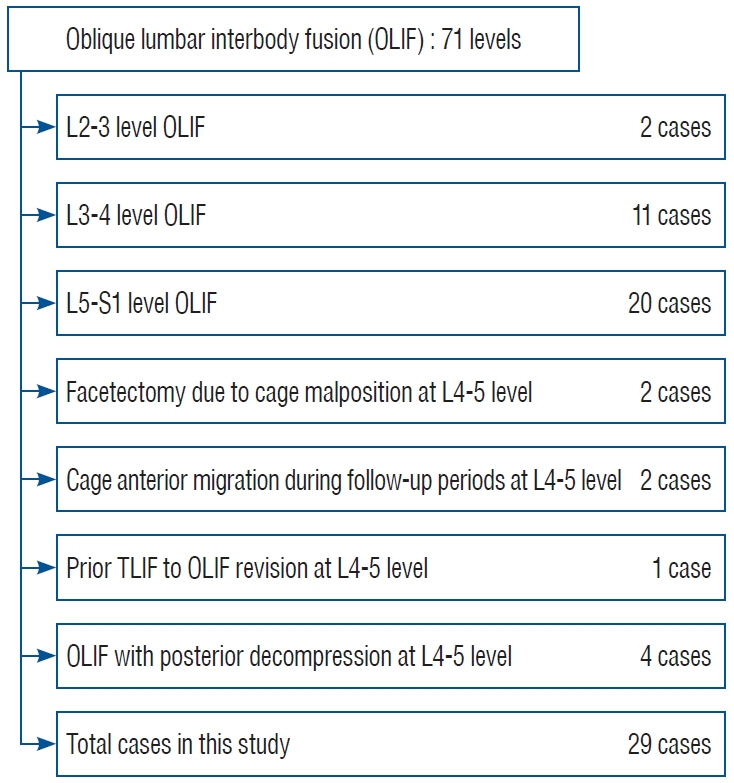
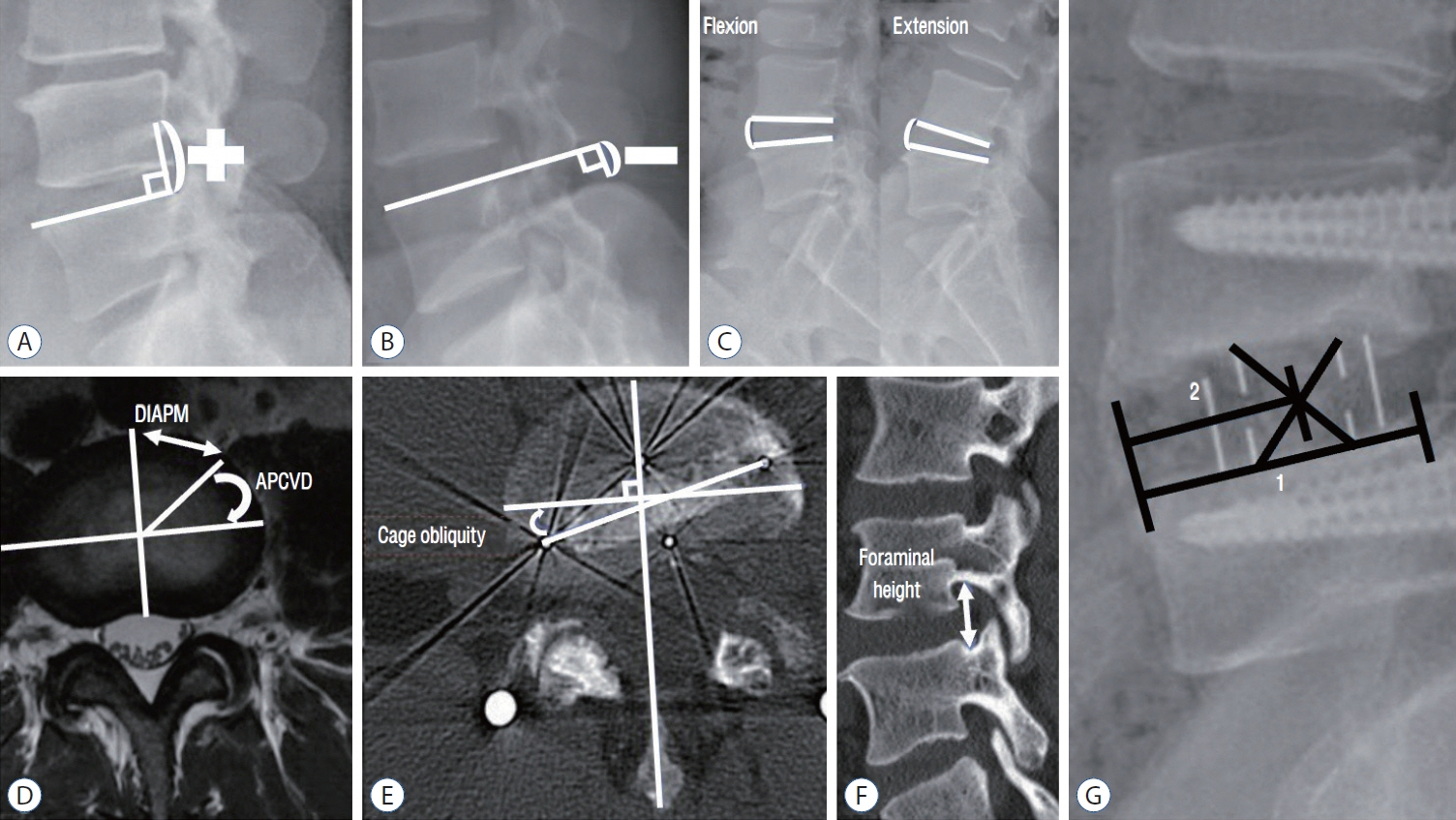
: Twenty-nine males who underwent L4-L5 OLIF for lumbar degenerative disease between 2019 and 2021 with a followup duration greater than 12 months were analyzed. Radiological parameters were measured including psoas muscle volume, total psoas area index (total psoas muscle area [cm2]/height squared [m2]), distance from the iliac artery to the origin of the psoas muscle (DIAPM), angle between the origin of the psoas muscle and the center of the vertebral disc (APCVD), iliac crest height, disc height, lumbar flexibility (lumbar flexion angle minus extension angle), cage location ratio, cage-induced segmental lumbar lordosis (LL) (postoperative index level segmental LL minus used cage angle), foraminal height changes, fusion grade.
Results
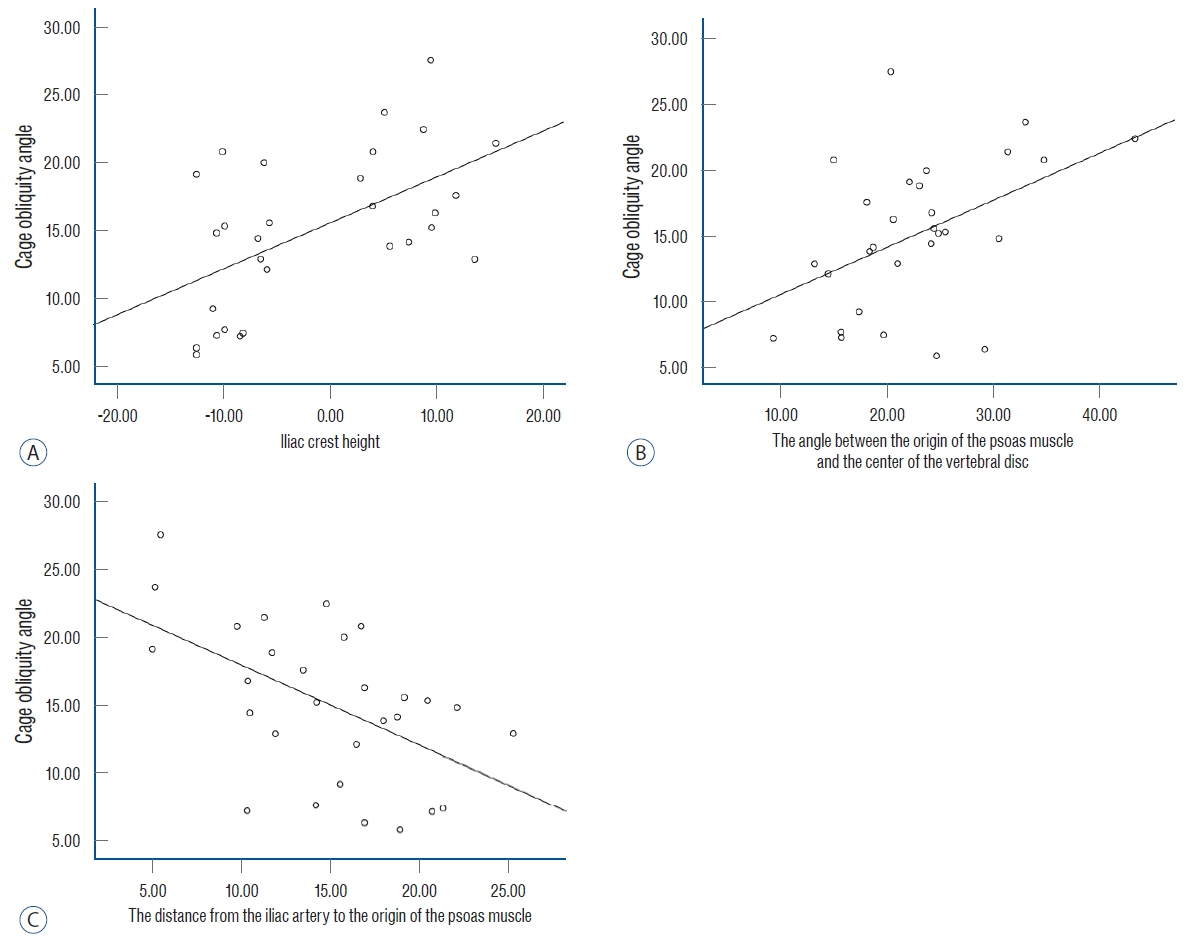
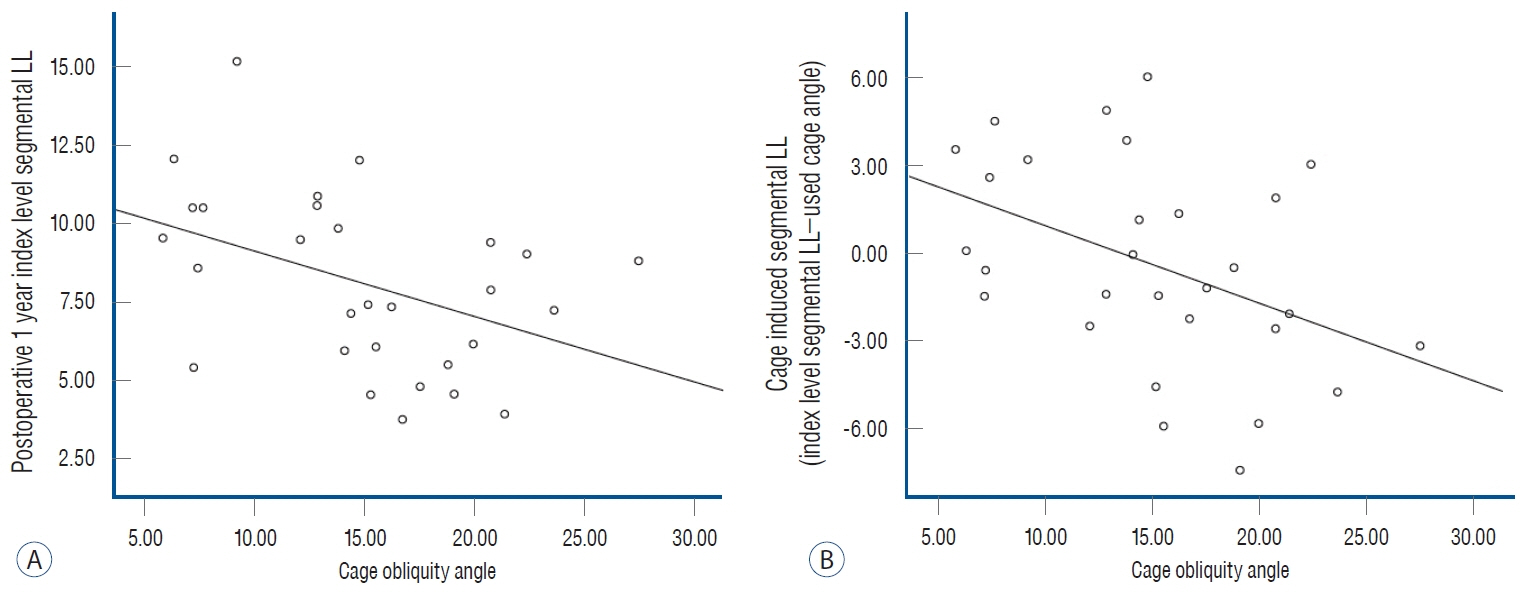
: DIAPM, APCVD, iliac crest height, postoperative index level segmental LL, and cage-induced segmental LL were significantly correlated with OLIF cage obliquity angle. However, other radiological parameters did not correlate with cage obliquity. Based on multiple regression analysis, the predictive equation for the OLIF cage obliquity angle was 13.062–0.318×DIAPM+0.325×A PCVD+0.174×iliac crest height. The greater the cage obliquity, the smaller the segmental LL compared to the cage angle used.
Conclusion
: At the L4-L5 level, OLIF cage obliquity was affected by DIAPM, APCVD, and iliac crest height, and as the cage obliquity angle increases, LL agnle achievable by the used cage could not be obtained.
Keyword
Figure
Reference
-
References
1. Allain J, Dufour T. Anterior lumbar fusion techniques: ALIF, OLIF, DLIF, LLIF, IXLIF. Orthop Traumatol Surg Res. 106:S149–S157. 2020.
Article2. Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 20:1410–1418. 1995.
Article3. Chung NS, Lee HD, Jeon CH. Accuracy of the lateral cage placement under intraoperative C-arm fluoroscopy in oblique lateral interbody fusion. J Orthop Sci. 23:918–922. 2018.
Article4. Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, et al. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine. 21:785–793. 2014.
Article5. Fontes RB, Traynelis VC. Iliac crest osteotomy to enhance exposure of the L4-5 interspace in minimally invasive lateral transpsoas interbody fusion: a cadaveric feasibility study. J Neurosurg Spine. 18:13–17. 2013.
Article6. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 40:E175–E182. 2015.
Article7. Hwang SH, Park SW, Kim YB. Risk factors for symptomatic contralateral foraminal stenosis after unilateral transforaminal lumbar interbody fusion. World Neurosurg. 133:e452–e458. 2020.
Article8. Jung JM, Chung CK, Kim CH, Yang SH, Won YI, Choi Y. Effects of total psoas area index on surgical outcomes of single-level lateral lumbar interbody fusion. World Neurosurg. 154:e838–e845. 2021.
Article9. Ko MJ, Park SW, Kim YB. Effect of cage in radiological differences between direct and oblique lateral interbody fusion techniques. J Korean Neurosurg Soc. 62:432–441. 2019.
Article10. Lee YS, Park SW, Kim YB. Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Korean Neurosurg Soc. 55:248–254. 2014.
Article11. Li J, Sun Y, Guo L, Zhang F, Ding W, Zhang W. Efficacy and safety of a modified lateral lumbar interbody fusion in L4-5 lumbar degenerative diseases compared with traditional XLIF and OLIF: a retrospective cohort study of 156 cases. BMC Musculoskelet Disord. 23:217. 2022.12. Liang Y, Zhao Y, Xu S, Zhu Z, Liu H, Mao K. Effects of different orientations of cage implantation on lumbar interbody fusion. World Neurosurg. 140:e97–e104. 2020.
Article13. Lovecchio FC, Vaishnav AS, Steinhaus ME, Othman YA, Gang CH, Iyer S, et al. Does interbody cage lordosis impact actual segmental lordosis achieved in minimally invasive lumbar spine fusion? Neurosurg Focus. 49:E17. 2020.
Article14. Mahatthanatrakul A, Kotheeranurak V, Lin GX, Hur JW, Chung HJ, Lokanath YK, et al. Do obliquity and position of the oblique lumbar interbody fusion cage influence the degree of indirect decompression of foraminal stenosis? J Korean Neurosurg Soc. 65:74–83. 2022.
Article15. Mayer HM. A new microsurgical technique for minimally invasive anterior lumbar interbody fusion. Spine (Phila Pa 1976). 22:691–699. discussion 700. 1997.
Article16. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. 1:2–18. 2015.17. Mourtzakis M, Prado CM, Lieffers JR, Reiman T, McCargar LJ, Baracos VE. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab. 33:997–1006. 2008.
Article18. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 6:435–443. 2006.
Article19. Parikh NP, Jhala AC. Contralateral lower limb radiculopathy following minimally invasive oblique lumbar interbody fusion in treatment of degenerative lumbar spine disease. J Minim Invasive Spine Surg Tech. 6:109–114. 2021.20. Park KH, Chung HW, Lee HD, Jeon CH, Koh JH, Chung NS. Cage obliquity and radiological outcomes in oblique lateral interbody fusion. Spine (Phila Pa 1976). 48:1611–1616. 2023.
Article21. Park SJ, Lee CS, Chung SS, Kang SS, Park HJ, Kim SH. The ideal cage position for achieving both indirect neural decompression and segmental angle restoration in lateral lumbar interbody fusion (LLIF). Clin Spine Surg. 30:E784–E790. 2017.
Article22. Regev GJ, Haloman S, Chen L, Dhawan M, Lee YP, Garfin SR, et al. Incidence and prevention of intervertebral cage overhang with minimally invasive lateral approach fusions. Spine (Phila Pa 1976). 35:1406–1411. 2010.
Article23. Wang Z, Liu L, Xu XH, Cao MD, Lu H, Zhang KB. The OLIF working corridor based on magnetic resonance imaging: a retrospective research. J Orthop Surg Res. 15:141. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Radiographic Alignment between Bilateral and Unilateral Interbody Cages in Patients Undergoing Transforaminal Lumbar Interbody Fusion
- Do Obliquity and Position of the Oblique Lumbar Interbody Fusion Cage Influence the Degree of Indirect Decompression of Foraminal Stenosis?
- Effect of Cage in Radiological Differences between Direct and Oblique Lateral Interbody Fusion Techniques
- Anterior Cage Migration during Transforaminal Lumbar Interbody Fusion: A Case Report and Review of the Literature
- Usefulness of Oblique Lateral Interbody Fusion at L5–S1 Level Compared to Transforaminal Lumbar Interbody Fusion