J Korean Neurosurg Soc.
2019 Jul;62(4):432-441. 10.3340/jkns.2018.0142.
Effect of Cage in Radiological Differences between Direct and Oblique Lateral Interbody Fusion Techniques
- Affiliations
-
- 1Department of Neurosurgery, Chung-Ang University Hospital, Seoul, Korea. nspsw@cau.ac.kr
- KMID: 2463674
- DOI: http://doi.org/10.3340/jkns.2018.0142
Abstract
OBJECTIVE
Few studies have reported direct comparative data of lumbar spine angles between direct lateral interbody fusion (DLIF) and oblique lateral interbody fusion (OLIF). The purpose of this study was to investigate the clinical and radiological outcomes of DLIF and OLIF, and determine influential factors.
METHODS
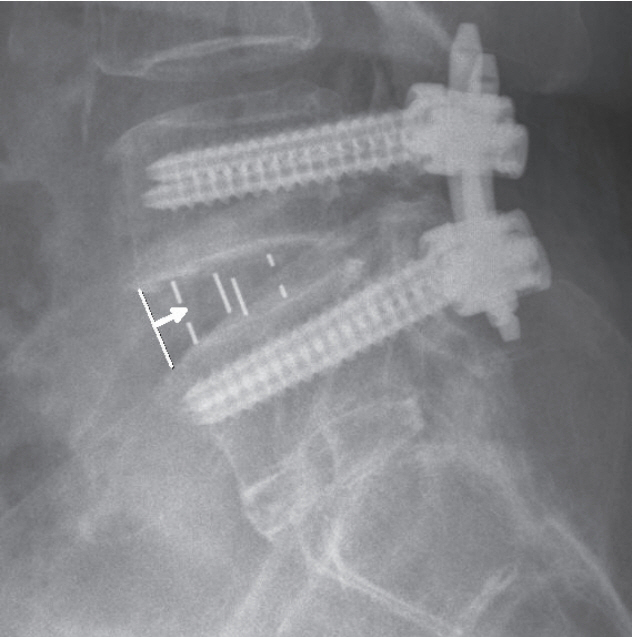
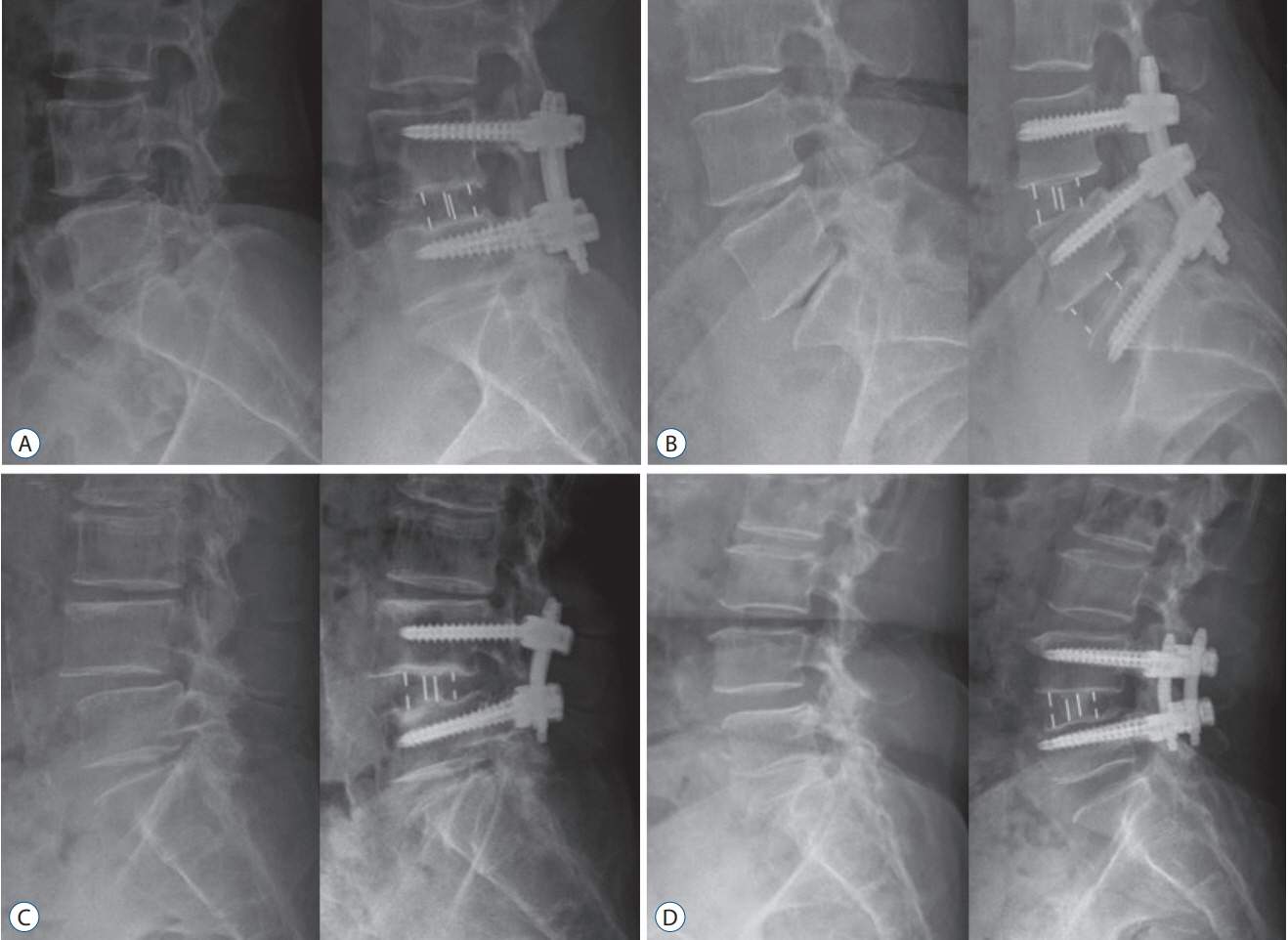
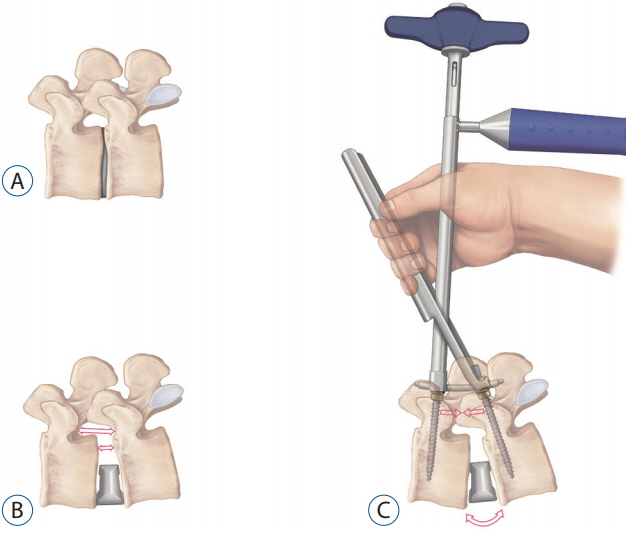
The same surgeon performed DLIF from May 2011 to August 2014 (n=201) and OLIF from September 2014 to September 2016 (n=142). Radiological parameters, cage height, cage angle (CA), cage width (CW), and cage location were assessed. We checked the cage location as the distance (mm) from the anterior margin of the disc space to the anterior metallic indicator of the cage in lateral images.
RESULTS
There were significant differences in intervertebral foramen height (FH; 22.0±2.4 vs. 21.0±2.1 mm, p<0.001) and sagittal disc angle (SDA; 8.7±3.3 vs. 11.3±3.2Ëš, p<0.001) between the DLIF and OLIF groups at 7 days postoperatively. CA (9.6±3.0 vs. 8.1±2.9Ëš, p<0.001) and CW (21.2±1.6 vs. 19.2±1.9 mm, p<0.001) were significantly larger in the OLIF group compared to the DLIF group. The cage location of the OLIF group was significantly more anterior than the DLIF group (6.7±3.0 vs. 9.1±3.6 mm, p<0.001). Cage subsidence at 1 year postoperatively was significantly worse in the DLIF group compared to the OLIF group (1.0±1.5 vs. 0.4±1.1 mm, p=0.001). Cage location was significantly correlated with postoperative FH (β=0.273, p<0.001) and postoperative SDA (β=-0.358, p<0.001). CA was significantly correlated with postoperative FH (β=-0.139, p=0.044) and postoperative SDA (β=0.236, p=0.001). Cage location (β=0.293, p<0.001) and CW (β=-0.225, p<0.001) were significantly correlated with cage subsidence.
CONCLUSION
The cage location, CA, and CW seem to be important factors which result in the different-radiological outcomes between DLIF and OLIF.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Factors Affecting Cage Obliquity and the Relationship between Cage Obliquity and Radiological Outcomes in Oblique Lateral Interbody Fusion at the L4-L5 Level
CheolWon Jang, SungHwan Hwang, Tae Kyung Jin, Hyung Jin Shin, Byung-Kyu Cho
J Korean Neurosurg Soc. 2023;66(6):703-715. doi: 10.3340/jkns.2023.0071.
Reference
-
References
1. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine (Phila Pa 1976). 42:55–62. 2017.
Article2. Acosta FL, Liu J, Slimack N, Moller D, Fessler R, Koski T. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 15:92–96. 2011.
Article3. Barone G, Scaramuzzo L, Zagra A, Giudici F, Perna A, Proietti L. Adult spinal deformity: effectiveness of interbody lordotic cages to restore disc angle and spino-pelvic parameters through completely mini-invasive trans-psoas and hybrid approach. Eur spine J. 26(Suppl 4):457–463. 2017.
Article4. Bridwell KH, Lenke LG, McEnery KW, Baldus C, Blanke K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine (Phila Pa 1976). 20:1410–1418. 1995.
Article5. Briski DC, Goel VK, Waddell BS, Serhan H, Kodigudla MK, Palepu V, et al. Does spanning a lateral lumbar interbody cage across the vertebral ring apophysis increase loads required for failure and mitigate endplate violation. Spine (Phila Pa 1976). 42:E1158–E1164. 2017.
Article6. Chang J, Kim JS, Jo H. Ventral dural injury after oblique lumbar interbody fusion. World Neurosurgery. 98:881.e1–881.e4. 2017.
Article7. Cheung KM, Zhang YG, Lu DS, Luk KD, Leong JC. Reduction of disc space distraction after anterior lumbar interbody fusion with autologous iliac crest graft. Spine (Phila Pa 1976). 28:1385–1389. 2003.
Article8. Cho JH, Joo YS, Lim C, Hwang CJ, Lee DH, Lee CS. Effect of one- or two-level posterior lumbar interbody fusion on global sagittal balance. Spine J. 17:1794–1802. 2017.
Article9. Davis TT, Hynes RA, Fung DA, Spann SW, MacMillan M, Kwon B, et al. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs in the lateral position: an anatomic study. J Neurosurg Spine. 21:785–793. 2014.
Article10. Elowitz EH, Yanni DS, Chwajol M, Starke RM, Perin NI. Evaluation of indirect decompression of the lumbar spinal canal following minimally invasive lateral transpsoas interbody fusion: radiographic and outcome analysis. Minim Invasive Neurosurg. 54:201–206. 2011.
Article11. Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 40:E175–E182. 2015.
Article12. Hijji FY, Narain AS, Bohl DD, Ahn J, Long WW, DiBattista JV, et al. Lateral lumbar interbody fusion: a systematic review of complication rates. Spine J. 17:1412–1419. 2017.
Article13. Jin J, Ryu KS, Hur JW, Seong JH, Kim JS, Cho HJ. Comparative study of the difference of perioperative complication and radiologic results: MISDLIF (minimally invasive direct lateral lumbar interbody fusion) versus MIS-OLIF (minimally invasive oblique lateral lumbar interbody fusion). Clin Spine Surg. 31:31–36. 2018.
Article14. Johnson RD, Valore A, Villaminar A, Comisso M, Balsano M. Pelvic parameters of sagittal balance in extreme lateral interbody fusion for degenerative lumbar disc disease. J Clin Neurosci. 20:576–581. 2013.
Article15. Kepler CK, Huang RC, Sharma AK, Meredith DS, Metitiri O, Sama AA, et al. Factors influencing segmental lumbar lordosis after lateral transpsoas interbody fusion. Orthop Surg. 4:71–75. 2012.
Article16. Kepler CK, Sharma AK, Huang RC, Meredith DS, Girardi FP, Cammisa FP Jr, et al. Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine. 16:329–333. 2012.
Article17. Kim JS, Lee HS, Shin DA, Kim KN, Yoon DH. Correction of coronal imbalance in degenerative lumbar spine disease following direct lateral interbody fusion (DLIF). Korean J Spine. 9:176–180. 2012.
Article18. Kim SJ, Lee YS, Kim YB, Park SW, Hung VT. Clinical and radiological outcomes of a new cage for direct lateral lumbar interbody fusion. Korean J Spine. 11:145–151. 2014.
Article19. Le TV, Baaj AA, Dakwar E, Burkett CJ, Murray G, Smith DA, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 37:1268–1273. 2012.
Article20. Lee HJ, Kim JS, Ryu KS, Park CK. Ureter injury as a complication of oblique lumbar interbody fusion. World Neurosurgery. 102:693.e7–693.e14. 2017.
Article21. Lee YS, Park SW, Kim YB. Direct lateral lumbar interbody fusion: clinical and radiological outcomes. J Korean Neurosurg Soc. 55:248–254. 2014.
Article22. Li JX, Phan K, Mobbs R. Oblique lumbar interbody fusion: technical aspects, operative outcomes, and complications. World Neurosurgery. 98:113–123. 2017.
Article23. Malham GM, Parker RM, Goss B, Blecher CM, Ballok ZE. Indirect foraminal decompression is independent of metabolically active facet arthropathy in extreme lateral interbody fusion. Spine (Phila Pa 1976). 39:E1303–E1310. 2014.
Article24. Marchi L, Abdala N, Oliveira L, Amaral R, Coutinho E, Pimenta L. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 19:110–118. 2013.
Article25. McAfee PC, Regan JJ, Geis WP, Fedder IL. Minimally invasive anterior retroperitoneal approach to the lumbar spine. Emphasis on the lateral BAK. Spine (Phila Pa 1976). 23:1476–1484. 1998.
Article26. Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine (Phila Pa 1976). 35(26 Suppl):S331–S337. 2010.
Article27. Ould-Slimane M, Lenoir T, Dauzac C, Rillardon L, Hoffmann E, Guigui P, et al. Influence of transforaminal lumbar interbody fusion procedures on spinal and pelvic parameters of sagittal balance. Eur Spine J. 21:1200–1206. 2012.
Article28. Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme lateral interbody fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. Spine J. 6:435–443. 2006.
Article29. Park SH, Park WM, Park CW, Kang KS, Lee YK, Lim SR. Minimally invasive anterior lumbar interbody fusion followed by percutaneous translaminar facet screw fixation in elderly patients. J Neurosurg Spine. 10:610–616. 2009.
Article30. Park SJ, Lee CS, Chung SS, Kang SS, Park HJ, Kim SH. The ideal cage position for achieving both indirect neural decompression and segmental angle restoration in lateral lumbar interbody fusion (LLIF). Clin Spine Surg. 30:E784–E790. 2017.
Article31. Phan K, Rao PJ, Scherman DB, Dandie G, Mobbs RJ. Lateral lumbar interbody fusion for sagittal balance correction and spinal deformity. J Clin Neurosci. 22:1714–1721. 2015.
Article32. Satake K, Kanemura T, Yamaguchi H, Segi N, Ouchida J. Predisposing factors for intraoperative endplate injury of extreme lateral interbody fusion. Asian Spine J. 10:907–914. 2016.
Article33. Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 24:242–250. 2011.34. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. 6:89–97. 2012.
Article35. St Clair S, Tan JS, Lieberman I. Oblique lumbar interbody fixation: a biomechanical study in human spines. J Spinal Disord Tech. 25:183–189. 2012.36. Tempel ZJ, Gandhoke GS, Bonfield CM, Okonkwo DO, Kanter AS. Radiographic and clinical outcomes following combined lateral lumbar interbody fusion and posterior segmental stabilization in patients with adult degenerative scoliosis. Neurosurg Focus. 36:E11. 2014.
Article37. Tokuhashi Y, Ajiro Y, Umezawa N. Subsidence of metal interbody cage after posterior lumbar interbody fusion with pedicle screw fixation. Orthopedics. 32:2009.
Article38. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 17:545–553. 2017.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pearls and Pitfalls of Oblique Lateral Interbody Fusion: A Comprehensive Narrative Review
- Factors Affecting Cage Obliquity and the Relationship between Cage Obliquity and Radiological Outcomes in Oblique Lateral Interbody Fusion at the L4-L5 Level
- Application of Lateral Approach for the Removal of Migrated Interbody Cage: Taphole and Fixing Technique
- The Navigated Oblique Lumbar Interbody Fusion: Accuracy Rate, Effect on Surgical Time, and Complications
- Repeated Migration of a Fusion Cage after Posterior Lumbar Interbody Fusion