Korean J Pain.
2023 Oct;36(4):441-449. 10.3344/kjp.23162.
Involvement of the spinal γγ-aminobutyric acid receptor in the analgesic effects of intrathecally injected hypertonic saline in spinal nerve-ligated rats
- Affiliations
-
- 1Department of Dental Anesthesiology, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Korea
- 2Department of Anesthesiology and Pain Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Anesthesiology and Pain Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2546706
- DOI: http://doi.org/10.3344/kjp.23162
Abstract
- Background
Hypertonic saline is used for treating chronic pain; however, clinical studies that aid in optimizing therapeutic protocols are lacking. We aimed to determine the concentration of intrathecally injected hypertonic saline at which the effect reaches its peak as well as the underlying γ-aminobutyric acid (GABA) receptor-related antinociceptive mechanism.
Methods
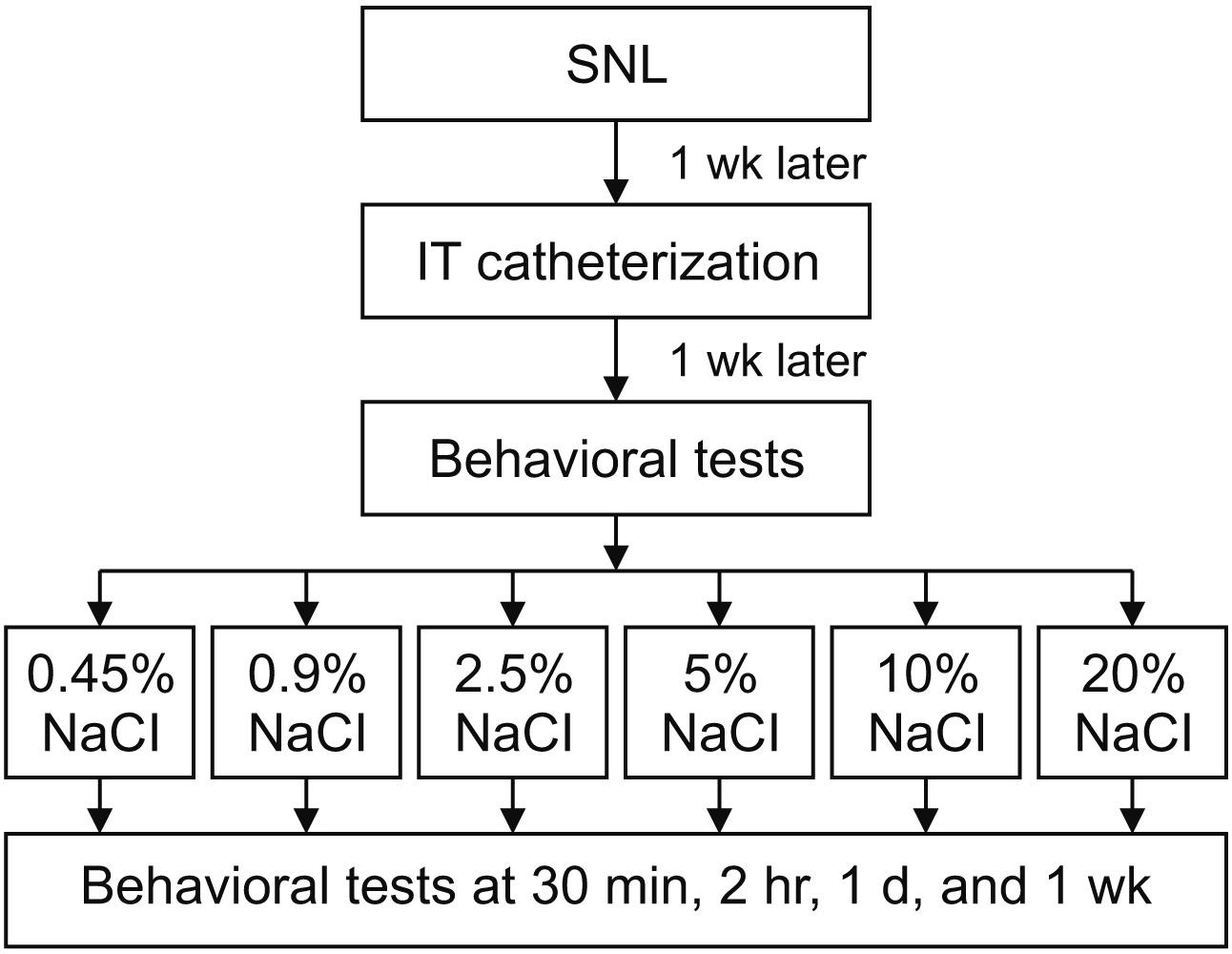
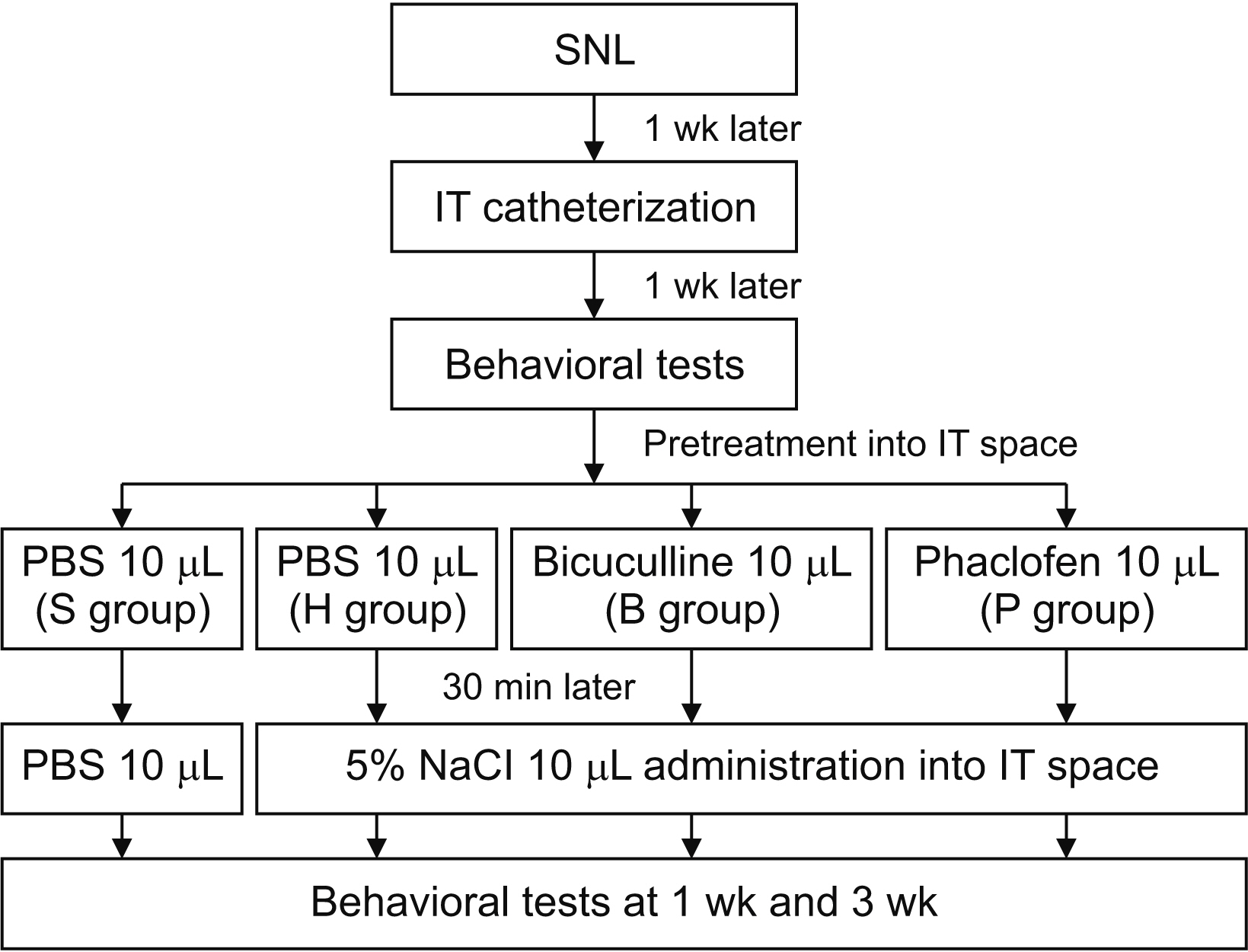
Spinal nerve ligation (SNL; left L5 and L6) was performed to induce neuropathic pain in rats weighing 250–300 g. Experiment 1: one week after implanting the intrathecal catheter, 60 rats were assigned randomly to intrathecal injection with 0.45%, 0.9%, 2.5%, 5%, 10%, and 20% NaCl, followed by behavioral testing at baseline and after 30 minutes, 2 hours, 1 day, and 1 week to determine the minimal concentration which produced maximal analgesia. Experiment 2: after determining the optimal intrathecal hypertonic saline concentration, 60 rats were randomly divided into four groups: Sham, hypertonic saline without pretreatment, and hypertonic saline after pretreatment with one of two GABA receptor antagonists (GABAA [bicuculline], or GABAB [phaclofen]). Behavioral tests were performed at weeks 1 and 3 following each treatment.
Results
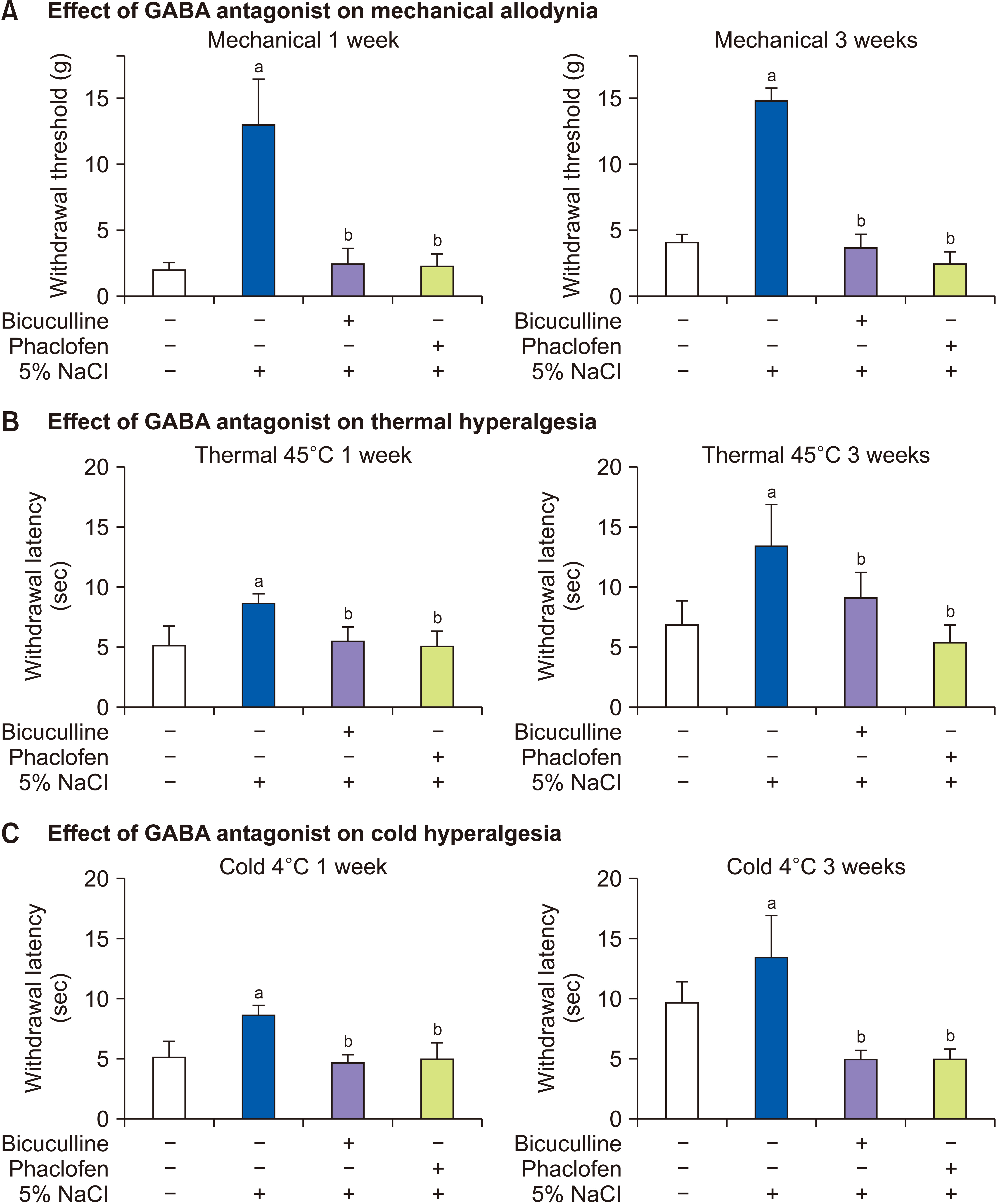
Hypertonic saline at concentrations greater than 5% alleviated SNL-induced mechanical allodynia and had a significant therapeutic effect, while showing a partial time- and dose-dependent antinociceptive effect on thermal and cold hyperalgesia. However, pretreatment with GABA receptor antagonists inhibited the antinociceptive effect of 5% NaCl.
Conclusions
This study indicates that the optimal concentration of hypertonic saline for controlling mechanical allodynia in neuropathic pain is 5%, and that its analgesic effect is related to GABAA and GABAB receptors.
Keyword
Figure
Reference
-
1. Hitchcock E. 1969; Osmolytic neurolysis for intractable facial pain. Lancet. 1:434–6. DOI: 10.1016/S0140-6736(69)91479-2. PMID: 4179502.
Article2. Hitchcock E, Prandini MN. 1973; Hypertonic saline in management of intractable pain. Lancet. 1:310–2. DOI: 10.1016/S0140-6736(73)91552-3. PMID: 4119183.
Article3. Lucas JT, Ducker TB, Perot PL Jr. 1975; Adverse reactions to intrathecal saline injection for control of pain. J Neurosurg. 42:557–61. DOI: 10.3171/jns.1975.42.5.0557. PMID: 1173818.
Article4. Thompson GE. 1971; Pulmonary edema complicating intrathecal hypertonic saline injection for intractable pain. Anesthesiology. 35:425–7. DOI: 10.1097/00000542-197110000-00020. PMID: 4107152.
Article5. Racz GB, Heavner JE, Singleton W, Carline M. Racz GB, editor. 1989. Hypertonic saline and corticosteroid injected epidurally for pain control. Techniques of neurolysis. Springer US;p. 73–86. DOI: 10.1007/978-1-4899-6721-3_7.6. Joo EY, Koh WU, Choi SS, Choi JH, Ahn HS, Yun HJ, et al. 2017; Efficacy of adjuvant 10% hypertonic saline in transforaminal epidural steroid injection: a retrospective analysis. Pain Physician. 20:E107–14. DOI: 10.36076/ppj.2017.1.E107. PMID: 28072802.7. Koh WU, Choi SS, Park SY, Joo EY, Kim SH, Lee JD, et al. 2013; Transforaminal hypertonic saline for the treatment of lumbar lateral canal stenosis: a double-blinded, randomized, active-control trial. Pain Physician. 16:197–211. DOI: 10.36076/ppj.2013/16/197. PMID: 23703407.8. Lee Y, Kim S, Shin JW, Leem JG, Choi SS. 2021; Adjuvant administration of hypertonic saline in lumbar epidural intervention may be associated with successful response in patients with probable neuropathic radicular pain Screened by Douleur Neuropathique 4. Int J Med Sci. 18:2736–42. DOI: 10.7150/ijms.59695. PMID: 34104106. PMCID: PMC8176191.
Article9. Karm MH, Kim CS, Kim DH, Lee D, Kim Y, Shin JW, et al. 2023; Effectiveness of percutaneous epidural neuroplasty using a balloon catheter in patients with chronic spinal stenosis accompanying mild spondylolisthesis: a longitudinal cohort study. Korean J Pain. 36:184–94. DOI: 10.3344/kjp.22289. PMID: 36514933. PMCID: PMC10043794.
Article10. Heavner JE, Racz GB, Raj P. 1999; Percutaneous epidural neuroplasty: prospective evaluation of 0.9% NaCl versus 10% NaCl with or without hyaluronidase. Reg Anesth Pain Med. 24:202–7. DOI: 10.1016/S1098-7339(99)90128-1. PMID: 10338168.11. Manchikanti L, Rivera JJ, Pampati V, Damron KS, McManus CD, Brandon DE, et al. 2004; One day lumbar epidural adhesiolysis and hypertonic saline neurolysis in treatment of chronic low back pain: a randomized, double-blind trial. Pain Physician. 7:177–86. DOI: 10.36076/ppj.2004/7/177. PMID: 16868590.12. Choi EJ, Yoo YJ, Lee PB, Kim YC, Lee SC, Moon JY. 2017; A retrospective study to evaluate the effect of concentration of hypertonic saline on efficacy and safety of epidural adhesiolysis. Anesth Analg. 124:2021–9. DOI: 10.1213/ANE.0000000000001925. PMID: 28448392.
Article13. Lee F, Jamison DE, Hurley RW, Cohen SP. 2014; Epidural lysis of adhesions. Korean J Pain. 27:3–15. DOI: 10.3344/kjp.2014.27.1.3. PMID: 24478895. PMCID: PMC3903797.
Article14. Watanabe M, Maemura K, Kanbara K, Tamayama T, Hayasaki H. 2002; GABA and GABA receptors in the central nervous system and other organs. Int Rev Cytol. 213:1–47. DOI: 10.1016/S0074-7696(02)13011-7. PMID: 11837891.
Article15. Jensen ML, Timmermann DB, Johansen TH, Schousboe A, Varming T, Ahring PK. 2002; The beta subunit determines the ion selectivity of the GABAA receptor. J Biol Chem. 277:41438–47. DOI: 10.1074/jbc.M205645200. PMID: 12177063.16. Sieghart W, Sperk G. 2002; Subunit composition, distribution and function of GABA(A) receptor subtypes. Curr Top Med Chem. 2:795–816. DOI: 10.2174/1568026023393507. PMID: 12171572.
Article17. Price TJ, Cervero F, Gold MS, Hammond DL, Prescott SA. 2009; Chloride regulation in the pain pathway. Brain Res Rev. 60:149–70. DOI: 10.1016/j.brainresrev.2008.12.015. PMID: 19167425. PMCID: PMC2903433.
Article18. Kim SH, Nam JS, Choi DK, Koh WW, Suh JH, Song JG, et al. 2011; Tumor necrosis factor-alpha and apoptosis following spinal nerve ligation injury in rats. Korean J Pain. 24:185–90. DOI: 10.3344/kjp.2011.24.4.185. PMID: 22220239. PMCID: PMC3248581.
Article19. Kim SH, Chung JM. 1992; An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain. 50:355–63. DOI: 10.1016/0304-3959(92)90041-9. PMID: 1333581.
Article20. Yaksh TL, Rudy TA. 1976; Chronic catheterization of the spinal subarachnoid space. Physiol Behav. 17:1031–6. DOI: 10.1016/0031-9384(76)90029-9. PMID: 14677603.
Article21. Chaplan SR, Bach FW, Pogrel JW, Chung JM, Yaksh TL. 1994; Quantitative assessment of tactile allodynia in the rat paw. J Neurosci Methods. 53:55–63. DOI: 10.1016/0165-0270(94)90144-9. PMID: 7990513.
Article22. Li Y, Dorsi MJ, Meyer RA, Belzberg AJ. 2000; Mechanical hyperalgesia after an L5 spinal nerve lesion in the rat is not dependent on input from injured nerve fibers. Pain. 85:493–502. DOI: 10.1016/S0304-3959(00)00250-5. PMID: 10781924.
Article23. Deuis JR, Dvorakova LS, Vetter I. 2017; Methods used to evaluate pain behaviors in rodents. Front Mol Neurosci. 10:284. DOI: 10.3389/fnmol.2017.00284. PMID: 28932184. PMCID: PMC5592204. PMID: f450b5fa74254e17af7228087c8fa228.
Article24. Biella GE, Groppetti A, Novelli A, Fernández-Sánchez MT, Manfredi B, Sotgiu ML. 2003; Neuronal sensitization and its behavioral correlates in a rat model of neuropathy are prevented by a cyclic analog of orphenadrine. J Neurotrauma. 20:593–601. DOI: 10.1089/089771503767168519. PMID: 12906743.
Article25. Malan TP, Mata HP, Porreca F. 2002; Spinal GABA(A) and GABA(B) receptor pharmacology in a rat model of neuropathic pain. Anesthesiology. 96:1161–7. DOI: 10.1097/00000542-200205000-00020. PMID: 11981157.26. Hara K, Haranishi Y, Kataoka K, Takahashi Y, Terada T, Nakamura M, et al. 2014; Chlorogenic acid administered intrathecally alleviates mechanical and cold hyperalgesia in a rat neuropathic pain model. Eur J Pharmacol. 723:459–64. DOI: 10.1016/j.ejphar.2013.10.046. PMID: 24184666.
Article27. Hitchcock E. 1967; Hypothermic subarachnoid irrigation for intractable pain. Lancet. 1:1133–5. DOI: 10.1016/S0140-6736(67)91709-6. PMID: 4164791.
Article28. King JS, Jewett DL, Sundberg HR. 1972; Differential blockade of cat dorsal root C fibers by various chloride solutions. J Neurosurg. 36:569–83. DOI: 10.3171/jns.1972.36.5.0569. PMID: 5067506.
Article29. Anderson SR, Racz GB, Heavner J. 2000; Evolution of epidural lysis of adhesions. Pain Physician. 3:262–70. DOI: 10.36076/ppj.2000/3/262. PMID: 16906184.
Article30. Gerdesmeyer L, Wagenpfeil S, Birkenmaier C, Veihelmann A, Hauschild M, Wagner K, et al. 2013; Percutaneous epidural lysis of adhesions in chronic lumbar radicular pain: a randomized, double-blind, placebo-controlled trial. Pain Physician. 16:185–96. DOI: 10.36076/ppj.2013/16/185. PMID: 23703406.31. Jewett DL, King JS. 1971; Conduction block of monkey dorsal rootlets by water and hypertonic saline solutions. Exp Neurol. 33:225–37. DOI: 10.1016/0014-4886(71)90116-6. PMID: 5000936.
Article32. Enna SJ, McCarson KE. 2006; The role of GABA in the mediation and perception of pain. Adv Pharmacol. 54:1–27. DOI: 10.1016/S1054-3589(06)54001-3. PMID: 17175808.
Article33. Zeilhofer HU, Benke D, Yevenes GE. 2012; Chronic pain states: pharmacological strategies to restore diminished inhibitory spinal pain control. Annu Rev Pharmacol Toxicol. 52:111–33. DOI: 10.1146/annurev-pharmtox-010611-134636. PMID: 21854227.
Article34. Hwang JH, Yaksh TL. 1997; The effect of spinal GABA receptor agonists on tactile allodynia in a surgically-induced neuropathic pain model in the rat. Pain. 70:15–22. DOI: 10.1016/S0304-3959(96)03249-6. PMID: 9106805.
Article35. Sokal DM, Chapman V. 2003; Effects of spinal administration of muscimol on C- and A-fibre evoked neuronal responses of spinal dorsal horn neurones in control and nerve injured rats. Brain Res. 962:213–20. DOI: 10.1016/S0006-8993(02)04057-X. PMID: 12543472.
Article36. Loomis CW, Khandwala H, Osmond G, Hefferan MP. 2001; Coadministration of intrathecal strychnine and bicuculline effects synergistic allodynia in the rat: an isobolographic analysis. J Pharmacol Exp Ther. 296:756–61. PMID: 11181903.37. Anseloni VC, Gold MS. 2008; Inflammation-induced shift in the valence of spinal GABA-A receptor-mediated modulation of nociception in the adult rat. J Pain. 9:732–8. DOI: 10.1016/j.jpain.2008.03.004. PMID: 18467182. PMCID: PMC2581496.
Article38. Sivilotti L, Woolf CJ. 1994; The contribution of GABAA and glycine receptors to central sensitization: disinhibition and touch-evoked allodynia in the spinal cord. J Neurophysiol. 72:169–79. DOI: 10.1152/jn.1994.72.1.169. PMID: 7965003.
Article39. Caba M, González-Mariscal G, Beyer C. 1994; Perispinal progestins enhance the antinociceptive effects of muscimol in the rat. Pharmacol Biochem Behav. 47:177–82. DOI: 10.1016/0091-3057(94)90128-7. PMID: 8115419.
Article40. Dirig DM, Yaksh TL. 1995; Intrathecal baclofen and muscimol, but not midazolam, are antinociceptive using the rat-formalin model. J Pharmacol Exp Ther. 275:219–27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differential expression of spinal γ-aminobutyric acid and opioid receptors modulates the analgesic effects of intrathecal curcumin on postoperative/inflammatory pain in rats
- The Role of Spinal Dopaminergic Transmission in the Analgesic Effect of Nefopam on Rat Inflammatory Pain
- Effects of cyclic nucleotides and glipizide on the cardiovascular response of baclofen in the rats
- The effect of inducing morphine tolerance on anti-allodynic action of gabapentin in spinal nerve-ligated rat
- The Analgesic Effect of Intrathecal Gabapentin in a Rat Model of Incisional Pain