Blood Res.
2023 Sep;58(3):138-144. 10.5045/br.2023.2023122.
ABO blood group and rhesus factor association with inpatient COVID-19 mortality and severity: a two-year retrospective review
- Affiliations
-
- 1Department of Internal Medicine, Arrowhead Regional Medical Center, CA, USA.
- 2Department of General Surgery, Arrowhead Regional Medical Center, CA, USA.
- 3Department of Critical Care Medicine, Arrowhead Regional Medical Center, CA, USA.
- 4Department of Graduate Medical Education, Arrowhead Regional Medical Center, CA, USA.
- 5School of Medicine, California University of Science and Medicine, Colton, CA, USA.
- KMID: 2546315
- DOI: http://doi.org/10.5045/br.2023.2023122
Abstract
- Background
Early reports have indicated a relationship between ABO and rhesus blood group types and infection with SARS-CoV-2. We aim to examine blood group type associations with COVID-19 mortality and disease severity.
Methods
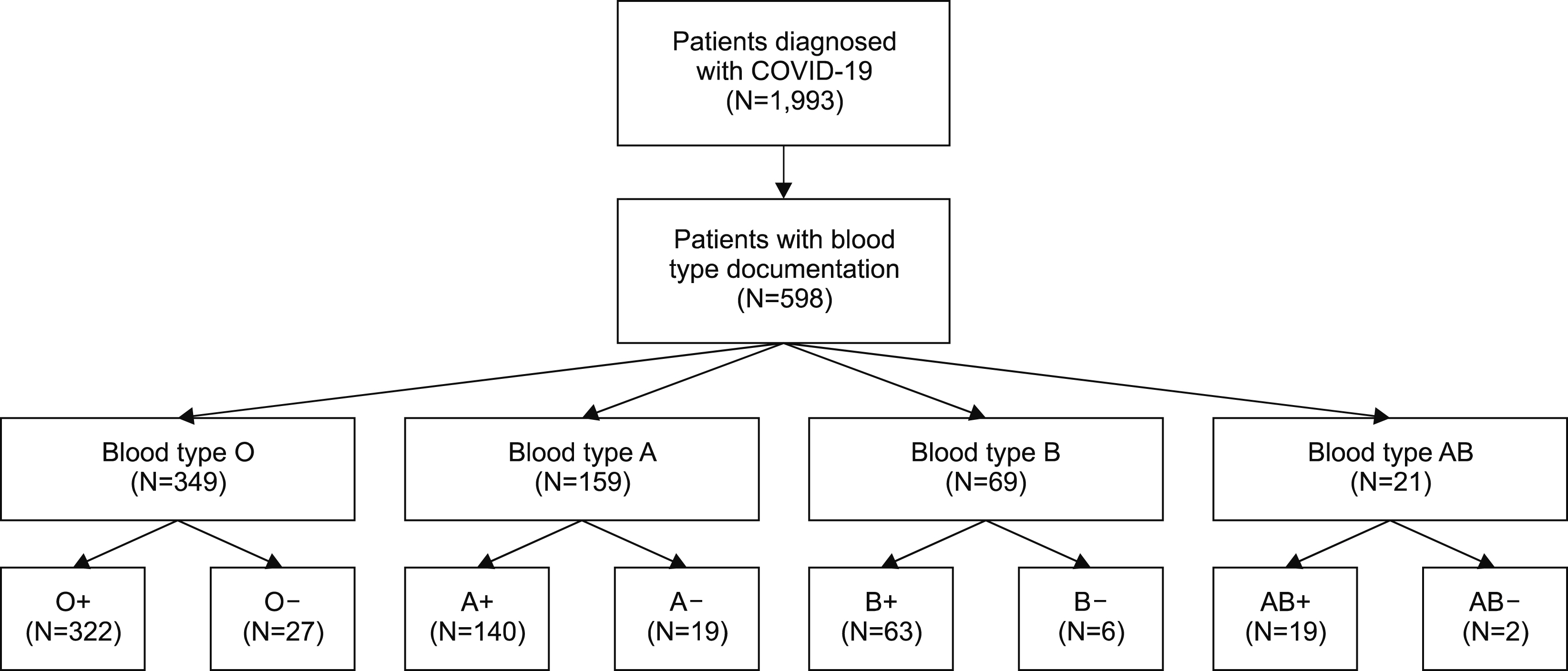
This is a retrospective chart review of patients ages 18 years or older admitted to the hospital with COVID-19 between January 2020 and December 2021. The primary outcome was COVID-19 mortality with respect to ABO blood group type. The secondary outcomes were 1. Severity of COVID-19 with respect to ABO blood group type, and 2. Rhesus factor association with COVID-19 mortality and disease severity. Disease severity was defined by degree of supplemental oxygen requirements (ambient air, low-flow, high-flow, non-invasive mechanical ventilation, and invasive mechanical ventilation).
Results
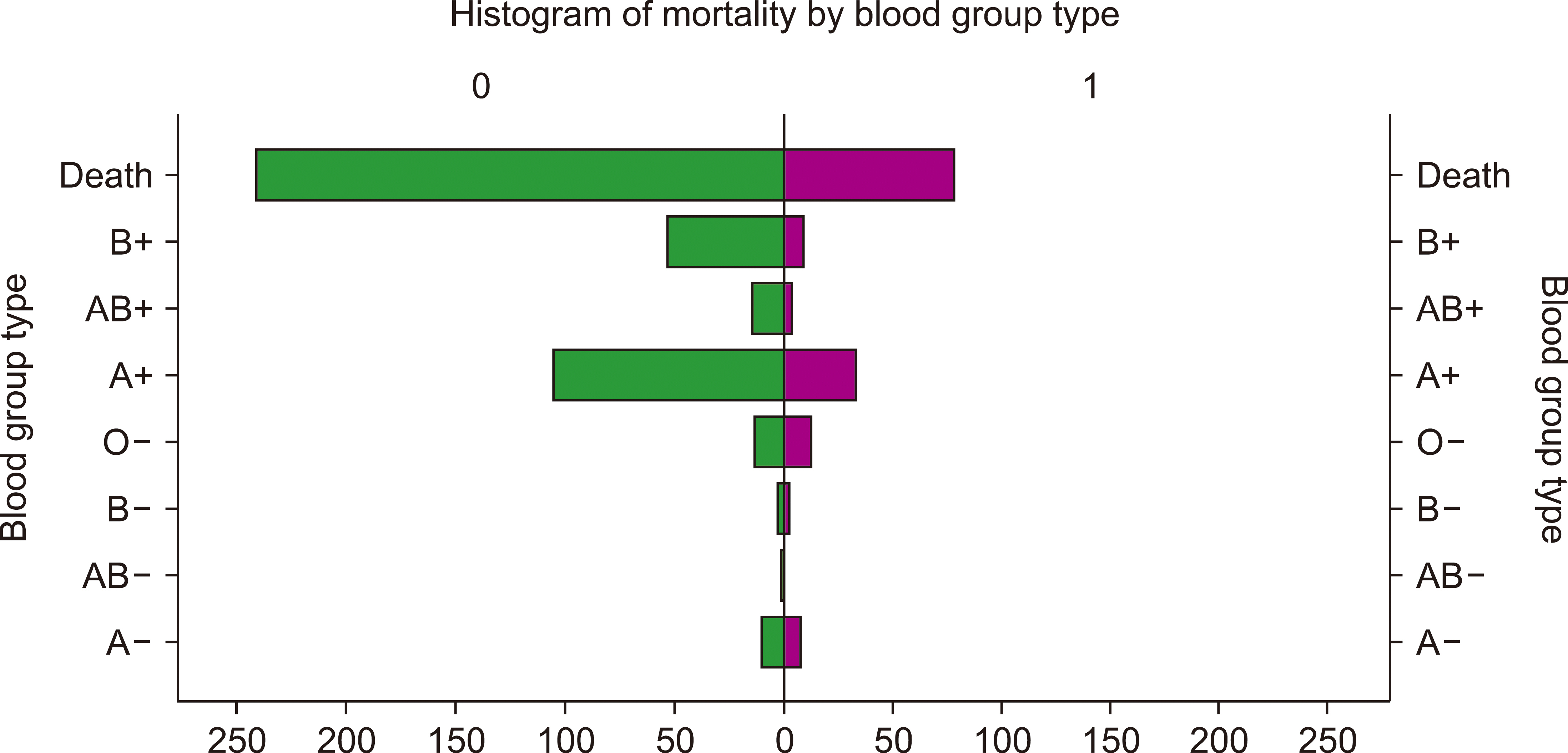
The blood type was collected on 596 patients with more than half (54%, N=322) being O+. The ABO blood type alone was not statistically associated with mortality (P=0.405), while the RH blood type was statistically associated with mortality (P<0.001). There was statistically significant association between combined ABO and RH blood type and mortality (P=0.014). Out of the mortality group, the O+ group had the highest mortality (52.3%), followed by A+ (22.8%). The combined ABO and RH blood type was statistically significantly associated with degree of supplemental oxygen requirements (P =0.005). The Kaplan-Meier curve demonstrated that Rh- patients had increased mortality.
Conclusion
ABO blood type is not associated with COVID-19 severity and mortality. Rhesus factor status is associated with COVID-19 severity and mortality. Rhesus negative patients were associated with increased mortality risk.
Figure
Reference
-
1. Fan Q, Zhang W, Li B, Li DJ, Zhang J, Zhao F. 2020; Association between ABO blood group system and COVID-19 susceptibility in Wuhan. Front Cell Infect Microbiol. 10:404. DOI: 10.3389/fcimb.2020.00404. PMID: 32793517. PMCID: PMC7385064. PMID: a710bec4e5124e02be76c61b6ddaca1f.
Article2. Wu BB, Gu DZ, Yu JN, Yang J, Shen WQ. 2020; Association between ABO blood groups and COVID-19 infection, severity and demise: a systematic review and meta-analysis. Infect Genet Evol. 84:104485. DOI: 10.1016/j.meegid.2020.104485. PMID: 32739464. PMCID: PMC7391292.
Article3. Zaidi FZ, Zaidi ARZ, Abdullah SM, Zaidi SZA. 2020; COVID-19 and the ABO blood group connection. Transfus Apher Sci. 59:102838. DOI: 10.1016/j.transci.2020.102838. PMID: 32513613. PMCID: PMC7834841.
Article4. Hoiland RL, Fergusson NA, Mitra AR, et al. 2020; The association of ABO blood group with indices of disease severity and multiorgan dysfunction in COVID-19. Blood Adv. 4:4981–9. DOI: 10.1182/bloodadvances.2020002623. PMID: 33057633. PMCID: PMC7594392.
Article5. Gutiérrez-Valencia M, Leache L, Librero J, Jericó C, Enguita Germán M, García-Erce JA. 2022; ABO blood group and risk of COVID-19 infection and complications: a systematic review and meta-analysis. Transfusion. 62:493–505. DOI: 10.1111/trf.16748. PMID: 34773411. PMCID: PMC8661771.
Article6. Jericó C, Zalba-Marcos S, Quintana-Díaz M, et al. 2022; Relationship between ABO blood group distribution and COVID-19 infection in patients admitted to the ICU: a multicenter observational Spanish study. J Clin Med. 11:3042. DOI: 10.3390/jcm11113042. PMID: 35683430. PMCID: PMC9181327. PMID: 6d9c6f6017a04f2f99b08ffcb72d41bc.
Article7. Balaouras G, Eusebi P, Kostoulas P. 2022; Systematic review and meta-analysis of the effect of ABO blood group on the risk of SARS-CoV-2 infection. PLoS One. 17:e0271451. DOI: 10.1371/journal.pone.0271451. PMID: 35901063. PMCID: PMC9333251. PMID: f56180babf894de7b61818620c884ec5.
Article8. Franchini M, Cruciani M, Mengoli C, et al. 2021; ABO blood group and COVID-19: an updated systematic literature review and meta-analysis. Blood Transfus. 19:317–26.9. Kabrah SM, Kabrah AM, Flemban AF, Abuzerr S. 2021; Systematic review and meta-analysis of the susceptibility of ABO blood group to COVID-19 infection. Transfus Apher Sci. 60:103169. DOI: 10.1016/j.transci.2021.103169. PMID: 34045120. PMCID: PMC8139534.
Article10. Liu N, Zhang T, Ma L, et al. 2021; The impact of ABO blood group on COVID-19 infection risk and mortality: a systematic review and meta-analysis. Blood Rev. 48:100785. DOI: 10.1016/j.blre.2020.100785. PMID: 33309392. PMCID: PMC7834371.
Article11. Zhao J, Yang Y, Huang H, et al. 2021; Relationship between the ABO blood group and the coronavirus disease 2019 (COVID-19) susceptibility. Clin Infect Dis. 73:328–31. DOI: 10.1093/cid/ciaa1150. PMID: 32750119. PMCID: PMC7454371.
Article12. Goel R, Bloch EM, Pirenne F, et al. 2021; ABO blood group and COVID-19: a review on behalf of the ISBT COVID-19 Working Group. Vox Sang. 116:849–61. DOI: 10.1111/vox.13076. PMID: 33578447. PMCID: PMC8014128.
Article13. Pereira E, Felipe S, de Freitas R, et al. 2022; ABO blood group and link to COVID-19: a comprehensive review of the reported associations and their possible underlying mechanisms. Microb Pathog. 169:105658. DOI: 10.1016/j.micpath.2022.105658. PMID: 35764188. PMCID: PMC9233352.
Article14. Soo KM, Chung KM, Mohd Azlan MAA, et al. 2022; The association of ABO and Rhesus blood type with the risks of developing SARS-CoV-2 infection: a meta-analysis. Trop Biomed. 39:126–34. DOI: 10.47665/tb.39.1.015. PMID: 35507935.
Article15. Ratiani L, Sanikidze TV, Ormotsadze G, Pachkoria E, Sordia G. 2022; Role of ABO blood groups in susceptibility and severity of COVID-19 in the Georgian population. Indian J Crit Care Med. 26:487–90. DOI: 10.5005/jp-journals-10071-24169. PMID: 35656053. PMCID: PMC9067498.
Article16. Kerbage A, Haddad SF, Nasr L, et al. 2022; Impact of ABO and Rhesus blood groups on COVID-19 susceptibility and severity: a case-control study. J Med Virol. 94:1162–6. DOI: 10.1002/jmv.27444. PMID: 34755349. PMCID: PMC8662239.
Article17. Hafez W, Ahmed S, Abbas N, et al. 2022; ABO blood group in relation to COVID-19 susceptibility and clinical outcomes: a retrospective observational study in the United Arab Emirates. Life (Basel). 12:1157. DOI: 10.3390/life12081157. PMID: 36013335. PMCID: PMC9410437. PMID: bade0f8edd2c42638d63a2ede02f6dac.
Article18. Zietz M, Zucker J, Tatonetti NP. 2020; Associations between blood type and COVID-19 infection, intubation, and death. Nat Commun. 11:5761. DOI: 10.1038/s41467-020-19623-x. PMID: 33188185. PMCID: PMC7666188. PMID: fee6c7193bca4afdb6a44c97ae4c21a0.
Article19. Rana R, Ranjan V, Kumar N. 2021; Association of ABO and Rh blood group in susceptibility, severity, and mortality of coronavirus disease 2019: a hospital-based study from Delhi, India. Front Cell Infect Microbiol. 11:767771. DOI: 10.3389/fcimb.2021.767771. PMID: 34796130. PMCID: PMC8593001. PMID: 252b60b4f7984013b5559a0f9169b8e1.
Article20. Anderson JL, May HT, Knight S, Bair TL, Horne BD, Knowlton KU. 2022; Association of Rhesus factor blood type with risk of SARS-CoV-2 infection and COVID-19 severity. Br J Haematol. 197:573–5. DOI: 10.1111/bjh.18086. PMID: 35106763.
Article21. Bokhary DH, Bokhary NH, Seadawi LE, Moafa AM, Khairallah HH, Bakhsh AA. 2022; Variation in COVID-19 disease severity and clinical outcomes between different ABO blood groups. Cureus. 14:e21838. DOI: 10.7759/cureus.21838. PMID: 35291516. PMCID: PMC8896246.
Article22. Arac E, Solmaz I, Akkoc H, et al. 2020; Association between the Rh blood group and the COVID-19 susceptibility. Int J Hematol Oncol. 30:81–6. DOI: 10.4999/uhod.204247.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Psychiatric Inpatient Care During the COVID-19 Pandemic: A Review
- Prognostic Factors for Survival or Severity After COVID-19 Infection in Cancer Patients: A Systematic Review and Meta-Analysis
- Convalescent Plasma Therapy in Coronavirus Disease 2019: a Case Report and Suggestions to Overcome Obstacles
- Management of Patients with Chronic Liver Disease: The Era of the COVID-19 Pandemic
- Methylprednisolone pulse therapy for critically ill patients with COVID-19: a cohort study