J Rhinol.
2023 Jul;30(2):69-79. 10.18787/jr.2023.00015.
Prognostic Factors for Survival or Severity After COVID-19 Infection in Cancer Patients: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Otorhinolaryngology, Yonsei University Wonju College of Medicine, Wonju, Republic of Korea
- 2Department of Otorhinolaryngology-Head and Neck Surgery, College of Medicine, Konkuk University, Seoul, Republic of Korea
- KMID: 2544616
- DOI: http://doi.org/10.18787/jr.2023.00015
Abstract
- Background and Objectives
Cancer organizations worldwide have recently released care guidelines for cancer patients with coronavirus disease 2019 (COVID-19). Several studies have reported higher mortality rates in cancer patients with COVID-19. However, drawing robust conclusions remains challenging due to a lack of research on clinical prognostic factors in this patient group.
Methods
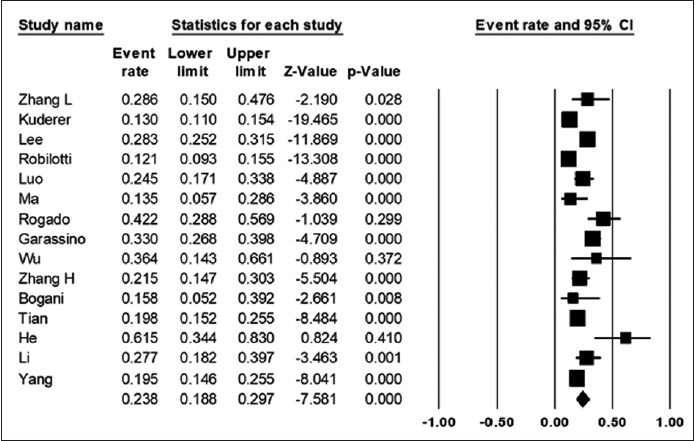
A comprehensive literature search was conducted using the PubMed, Embase, and Cochrane databases. We searched the keywords in the following combination: (“COVID-19” or “coronavirus” or “wuhan virus”) and (“cancer”). The search was performed on August 1, 2020, and only papers written in English were included in this study. We collected data from 3,215 cancer patients with COVID-19 from 16 studies and analyzed overall mortality after COVID-19 infection in cancer patients compared to controls, as well as prognostic factors for severity and mortality after COVID-19 infection. The prognostic factors analyzed encompassed demographics, comorbidities, symptoms, cancer treatment within 4 weeks of COVID-19 diagnosis, and treatment for COVID-19 infection.
Results
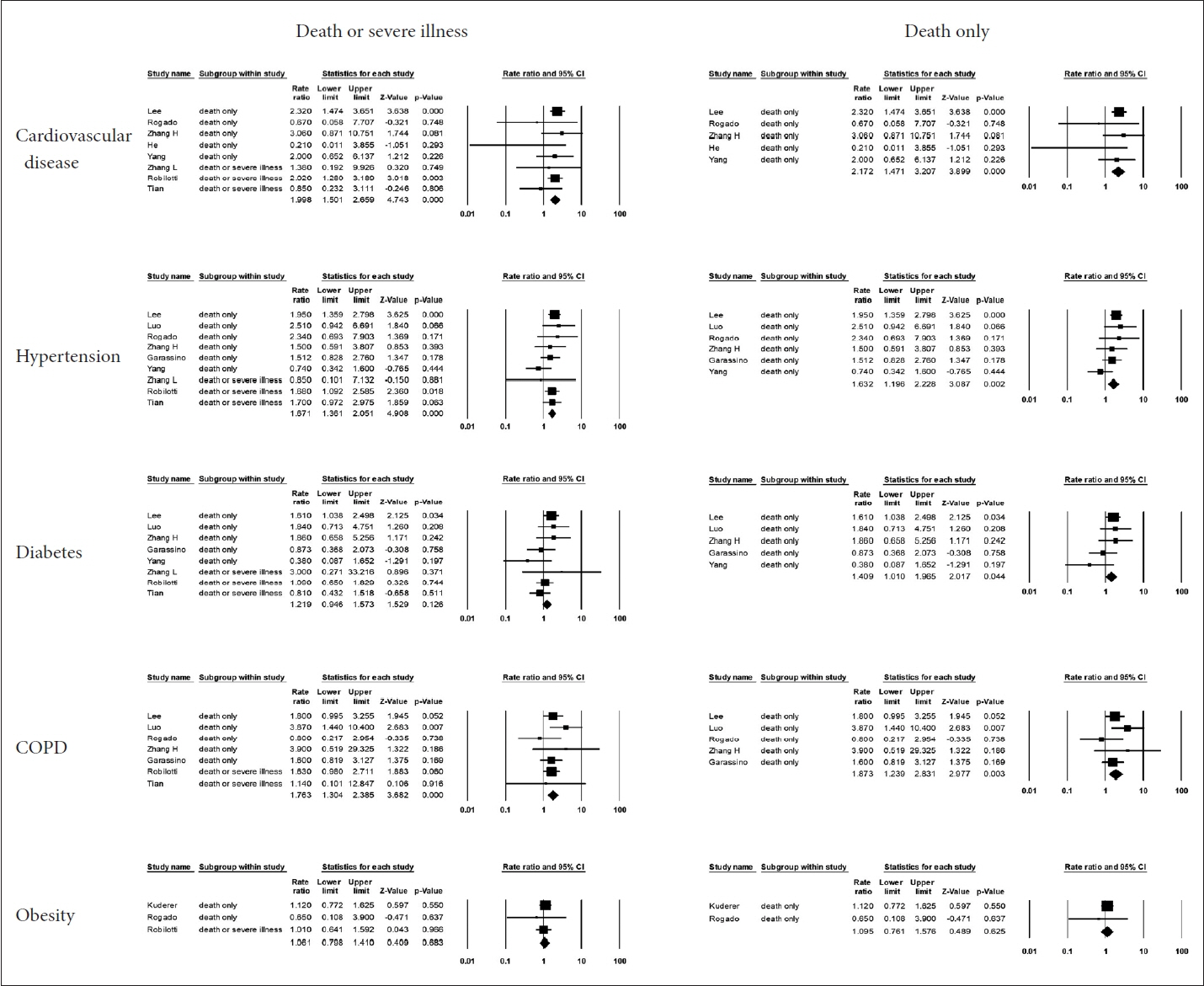
This meta-analysis evaluated mortality rates and related prognostic factors in cancer patients infected with COVID-19. First, 15 of the 16 studies reported mortality data; 663 patients died among a total of 3,215 people, resulting in a combined mortality rate of 21%. Second, the following poor prognostic factors were identified: male sex, older age (≥65 years), respiratory symptoms (e.g., cough and dyspnea), and other comorbidities (e.g., cardiovascular disease, hypertension, and chronic obstructive pulmonary disease).
Conclusion
The mortality of cancer patients infected with COVID-19 can reach about 20%.
Keyword
Figure
Reference
-
References
1. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020; 395(10223):470–3.2. Bakouny Z, Hawley JE, Choueiri TK, Peters S, Rini BI, Warner JL, et al. COVID-19 and cancer: current challenges and perspectives. Cancer Cell. 2020; 38(5):629–46.3. Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020; 55(5):2000547.4. Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, et al. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020; 31(8):1088–9.5. He W, Chen L, Chen L, Yuan G, Fang Y, Chen W, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020; 34(6):1637–45.6. Rubinstein SM, Steinharter JA, Warner J, Rini BI, Peters S, Choueiri TK. The COVID-19 and cancer consortium: a collaborative effort to understand the effects of COVID-19 on patients with cancer. Cancer Cell. 2020; 37(6):738–41.7. Whisenant JG, Trama A, Torri V, De Toma A, Viscardi G, Cortellini A, et al. TERAVOLT: thoracic cancers international COVID-19 collaboration. Cancer Cell. 2020; 37(6):742–5.8. UK Coronavirus Cancer Monitoring Project Team. The UK coronavirus cancer monitoring project: protecting patients with cancer in the era of COVID-19. Lancet Oncol. 2020; 21(5):622–4.9. Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020; 31(7):894–901.10. Kuderer NM, Choueiri TK, Shah DP, Shyr Y, Rubinstein SM, Rivera DR, et al. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet. 2020; 395(10241):1907–18.11. Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020; 395(10241):1919–26.12. Robilotti EV, Babady NE, Mead PA, Rolling T, Perez-Johnston R, Bernardes M, et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med. 2020; 26(8):1218–23.13. Luo J, Rizvi H, Preeshagul IR, Egger JV, Hoyos D, Bandlamudi C, et al. COVID-19 in patients with lung cancer. Ann Oncol. 2020; 31(10):1386–96.14. Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020; 21(3):335–7.15. Ma J, Yin J, Qian Y, Wu Y. Clinical characteristics and prognosis in cancer patients with COVID-19: a single center’s retrospective study. J Infect. 2020; 81(2):318–56.16. Rogado J, Obispo B, Pangua C, Serrano-Montero G, Martín Marino A, Pérez-Pérez M, et al. Covid-19 transmission, outcome and associated risk factors in cancer patients at the first month of the pandemic in a Spanish hospital in Madrid. Clin Transl Oncol. 2020; 22(12):2364–8.17. Garassino MC, Whisenant JG, Huang LC, Trama A, Torri V, Agustoni F, et al. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol. 2020; 21(7):914–22.18. Wu Q, Chu Q, Zhang H, Yang B, He X, Zhong Y, et al. Clinical outcomes of coronavirus disease 2019 (COVID-19) in cancer patients with prior exposure to immune checkpoint inhibitors. Cancer Commun (Lond). 2020; 40(8):374–9.19. Zhang H, Wang L, Chen Y, Wu Q, Chen G, Shen X, et al. Outcomes of novel coronavirus disease 2019 (COVID-19) infection in 107 patients with cancer from Wuhan, China. Cancer. 2020; 126(17):4023–31.20. Bogani G, Ditto A, Bosio S, Brusadelli C, Raspagliesi F. Cancer patients affected by COVID-19: experience from Milan, Lombardy. Gynecol Oncol. 2020; 158(2):262–5.21. Tian J, Yuan X, Xiao J, Zhong Q, Yang C, Liu B, et al. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020; 21(7):893–903.22. Li Q, Chen L, Li Q, He W, Yu J, Chen L, et al. Cancer increases risk of in-hospital death from COVID-19 in persons <65 years and those not in complete remission. Leukemia. 2020; 34(9):2384–91.23. Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K, et al. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol. 2020; 21(7):904–13.24. ElGohary GM, Hashmi S, Styczynski J, Kharfan-Dabaja MA, Alblooshi RM, de la Cámara R, et al. The risk and prognosis of COVID-19 infection in cancer patients: a systematic review and meta-analysis. Hematol Oncol Stem Cell Ther. 2022; 15(2):45–53.25. Piroth L, Cottenet J, Mariet AS, Bonniaud P, Blot M, Tubert-Bitter P, et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2021; 9(3):251–9.26. Hanna TP, King WD, Thibodeau S, Jalink M, Paulin GA, HarveyJones E, et al. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ. 2020; 371:m4087.27. Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020; 8(4):420–2.28. Lou E, Teoh D, Brown K, Blaes A, Holtan SG, Jewett P, et al. Perspectives of cancer patients and their health during the COVID-19 pandemic. PLoS One. 2020; 15(10):e0241741.29. Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, et al. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (COVID-19) pandemic: an international collaborative group. Oncologist. 2020; 25(6):e936–45.30. Yu J, Ouyang W, Chua MLK, Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol. 2020; 6(7):1108–10.31. Al-Quteimat OM, Amer AM. The impact of the COVID-19 pandemic on cancer patients. Am J Clin Oncol. 2020; 43(6):452–5.32. National Institutes of Health. Special considerations in adults and children with cancer [Internet]. Bethesda, MD: National Institutes of Health;2023. [cited 2020 June 1]. Available from: https://www.covid19-treatmentguidelines.nih.gov/special-populations/cancer/.33. Derosa L, Melenotte C, Griscelli F, Gachot B, Marabelle A, Kroemer G, et al. The immuno-oncological challenge of COVID-19. Nat Cancer. 2020; 1(10):946–64.34. Bi J, Ma H, Zhang D, Huang J, Yang D, Wang Y, et al. Does chemotherapy reactivate SARS-CoV-2 in cancer patients recovered from prior COVID-19 infection? Eur Respir J. 2020; 56(4):2002672.35. Centers for Disease Control and Prevention. COVID-19 treatments and medications [Internet]. Atlanta, GA: Centers for Disease Control and Prevention;2023. [cited 2020 June 1]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/therapeutic-options.html.36. Gautret P, Lagier JC, Parola P, Hoang VT, Meddeb L, Mailhe M, et al. Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial. Int J Antimicrob Agents. 2020; 56(1):105949.37. Boulware DR, Pullen MF, Bangdiwala AS, Pastick KA, Lofgren SM, Okafor EC, et al. A randomized trial of hydroxychloroquine as postexposure prophylaxis for Covid-19. N Engl J Med. 2020; 383(6):517–25.38. Cavalcanti AB, Zampieri FG, Rosa RG, Azevedo LCP, Veiga VC, Avezum A, et al. Hydroxychloroquine with or without azithromycin in mild-to-moderate Covid-19. N Engl J Med. 2020; 383(21):2041–52.39. Recovery Collaborative Group, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021; 384(8):693–704.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies
- Predictors of Mortality in Patients with COVID-19: A Systematic Review and Meta-analysis
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- Clinical and Laboratory Features of Pediatric Patients with COVID-19: Systematic Review and Meta-analysis
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis