J Korean Neurosurg Soc.
2023 Jul;66(4):426-437. 10.3340/jkns.2022.0233.
Ultrasonic Osteotome Assisted Posterior Endoscopic Cervical Foraminotomy in the Treatment of Cervical Spondylotic Radiculopathy Due to Osseous Foraminal Stenosis
- Affiliations
-
- 1Department of Neurosurgery, Minhang Hospital, Fudan University, Shanghai, China
- 2Department of Neurosurgery, Zhongshan Hospital, Fudan University, Shanghai, China
- KMID: 2543534
- DOI: http://doi.org/10.3340/jkns.2022.0233
Abstract
Objective
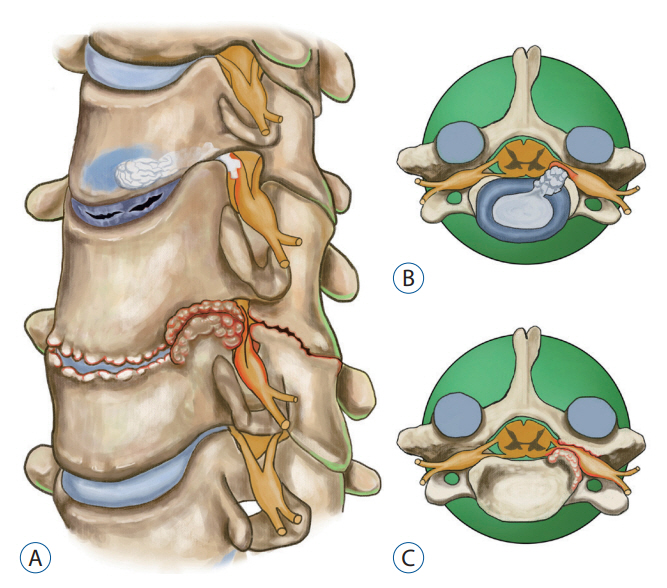
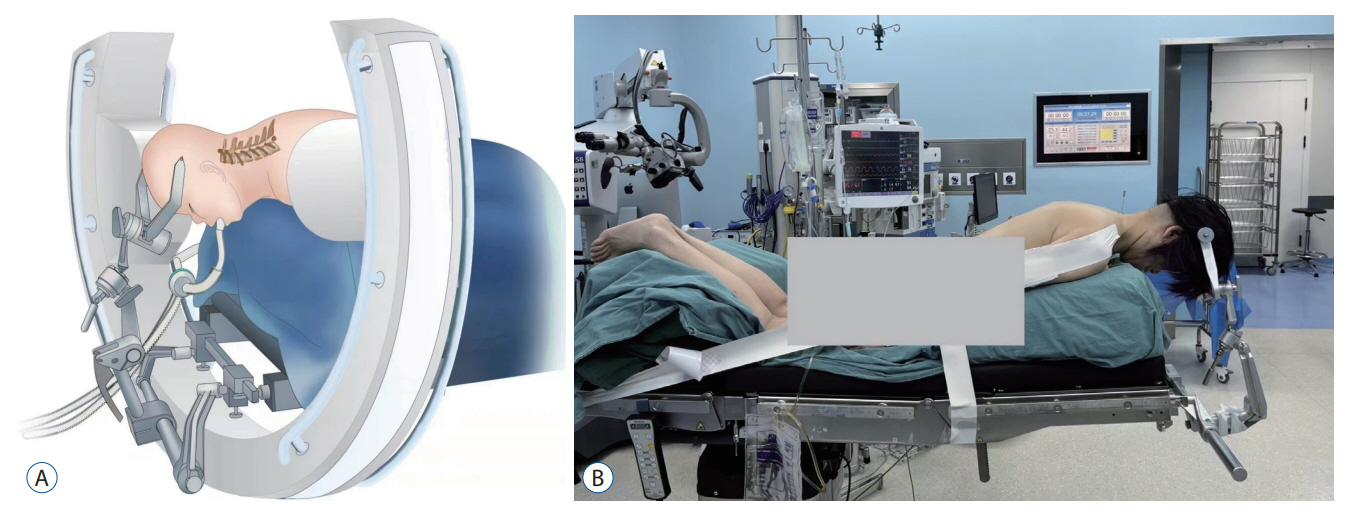
: To investigate the efficacy and safety of the posterior endoscopic cervical foraminotomy (PECF) using ultrasonic osteotome for the treatment of cervical osseous foraminal stenosis,focusing on introduction of the advantages of ultrasonic osteotome in partial pediculectomy and ventral osteophyte resection in PECF.
Methods
: Nineteen patients with cervical osseous foraminal stenosis who underwent PECF using ultrasonic osteotome in our institution between April 2018 and April 2021 were enrolled in this study. All the patients were followed up more than 12 months. The patients’ medical data, as well as pre- and postoperative radiologic findings were thoroughly investigated. The visual analogue score (VAS), Japanese Orthopaedic Association (JOA) score, cervical dysfunction index (Neck disability index, NDI), and modified MacNab criteria were used to assess the surgical efficacy.
Results
: All the patients were successfully treated with PECF using ultrasonic osteotome. The pre- and postoperative VAS, NDI, and JOA scores were significantly improved (p<0.05). According to the modified MacNab criteria, 17 patients were assessed as “excellent”, two patients were assessed as “good” at the last follow-up. There was no dura tear, nerve root damage, incision infection, neck deformity, or other complications.
Conclusion
: Adequate nerve root decompression can be accomplished successfully with the help of ultrasonic osteotome in PECF, which has the advantage of reducing the probability of damage to the nerve root and dura mater, in addition to the original merits of endoscopic surgery.
Keyword
Figure
Reference
-
References
1. Albert TJ, Vacarro A. Postlaminectomy kyphosis. Spine (Phila Pa 1976). 23:2738–2745. 1998.2. Al-Mahfoudh R, Qattan E, Ellenbogen JR, Wilby M, Barrett C, Pigott T. Applications of the ultrasonic bone cutter in spinal surgery--our preliminary experience. Br J Neurosurg. 28:56–60. 2014.3. Bydon M, Macki M, Xu R, Ain MC, Ahn ES, Jallo GI. Spinal decompression in achondroplastic patients using high-speed drill versus ultrasonic bone curette: technical note and outcomes in 30 cases. J Pediatr Orthop. 34:780–786. 2014.4. Desai MJ, Padmanabhan G, Simbasivan A, Kamanga-Sollo GG, Dharmappa A. Directional preference following epidural steroid injection in three patients with acute cervical radiculopathy. Pain Pract. 13:559–565. 2013.5. Epstein NE. A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int. 10:100. 2019.6. Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. Anterior cervical discectomy and fusion associated complications. Spine (Phila Pa 1976). 32:2310–2317. 2007.
Article7. Gokaslan ZL, Telfeian AE, Wang MY. Introduction: endoscopic spine surgery. Neurosurg Focus. 40:E1. 2016.
Article8. Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE Jr, et al. Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosurg Spine. 25:285–291. 2016.
Article9. Hazer DB, Yaşar B, Rosberg HE, Akbaş A. Technical aspects on the use of ultrasonic bone shaver in spine surgery: experience in 307 patients. Biomed Res Int. 2016:8428530. 2016.
Article10. Kim HS, Wu PH, Lee YJ, Kim DH, Kim JY, Lee JH, et al. Safe route for cervical approach: partial pediculotomy, partial vertebrotomy approach for posterior endoscopic cervical foraminotomy and discectomy. World Neurosurg. 140:e273–e282. 2020.
Article11. Klaassen Z, Tubbs RS, Apaydin N, Hage R, Jordan R, Loukas M. Vertebral spinal osteophytes. Anat Sci Int. 86:1–9. 2011.
Article12. Komp M, Oezdemir S, Hahn P, Ruetten S. Full-endoscopic posterior foraminotomy surgery for cervical disc herniations. Oper Orthop Traumatol. 30:13–24. 2018.
Article13. Lee DG, Park CK, Lee DC. Clinical and radiological results of posterior cervical foraminotomy at two or three levels: a 3-year follow-up. Acta Neurochir (Wien). 159:2369–2377. 2017.
Article14. Li ZZ, Cao Z, Zhao HL, Shang WL, Hou SX. Ultrasonic osteotome assisted full-endoscopic en block resection of thoracic ossified ligamentum flavum: technical note and 2 years follow-up. Pain Physician. 24:E239–E248. 2021.15. Massel DH, Mayo BC, Bohl DD, Narain AS, Hijji FY, Fineberg SJ, et al. Improvements in neck and arm pain following an anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 42:E825–E832. 2017.
Article16. Mok JK, Sheha ED, Samuel AM, McAnany SJ, Vaishnav AS, Albert TJ, et al. Evaluation of current trends in treatment of single-level cervical radiculopathy. Clin Spine Surg. 32:E241–E245. 2019.
Article17. Oh HS, Hwang BW, Park SJ, Hsieh CS, Lee SH. Percutaneous endoscopic cervical discectomy (PECD): an analysis of outcome, causes of reoperation. World Neurosurg. 102:583–592. 2017.
Article18. Papavero L, Kothe R. Minimally invasive posterior cervical foraminotomy for treatment of radiculopathy : an effective, time-tested, and cost-efficient motion-preservation technique. Oper Orthop Traumatol. 30:36–45. 2018.
Article19. Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic cervical posterior foraminotomy for the operation of lateral disc herniations using 5.9-mm endoscopes: a prospective, randomized, controlled study. Spine (Phila Pa 1976). 33:940–948. 2008.
Article20. Selvanathan SK, Beagrie C, Thomson S, Corns R, Deniz K, Derham C, et al. Anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of brachialgia: the Leeds spinal unit experience (2008-2013). Acta Neurochir (Wien). 157:1595–1600. 2015.
Article21. Shriver MF, Lewis DJ, Kshettry VR, Rosenbaum BP, Benzel EC, Mroz TE. Dysphagia rates after anterior cervical diskectomy and fusion: a systematic review and meta-analysis. Global Spine J. 7:95–103. 2017.
Article22. Tong Y, Huang Z, Hu C, Fan Z, Bian F, Yang F, et al. A comparison study of posterior cervical percutaneous endoscopic ventral bony decompression and simple dorsal decompression treatment in cervical spondylotic radiculopathy caused by cervical foraminal and/or lateral spinal stenosis: a clinical retrospective study. BMC Musculoskelet Disord. 21:290. 2020.
Article23. Wan Q, Zhang D, Li S, Liu W, Wu X, Ji Z, et al. Posterior percutaneous full-endoscopic cervical discectomy under local anesthesia for cervical radiculopathy due to soft-disc herniation: a preliminary clinical study. J Neurosurg Spine. 29:351–357. 2018.
Article24. Xiao CM, Yu KX, Deng R, Long QY, Chu L, Xiong Y, et al. Modified Khole percutaneous endoscopic surgery for cervical foraminal stenosis: partial pediculectomy approach. Pain Physician. 22:E407–E416. 2019.25. Yamazaki S, Kokubun S, Ishii Y, Tanaka Y. Courses of cervical disc herniation causing myelopathy or radiculopathy: an analysis based on computed tomographic discograms. Spine (Phila Pa 1976). 28:1171–1175. 2003.
Article26. Ye ZY, Kong WJ, Xin ZJ, Fu Q, Ao J, Cao GR, et al. Clinical observation of posterior percutaneous full-endoscopic cervical foraminotomy as a treatment for osseous foraminal stenosis. World Neurosurg. 106:945–952. 2017.
Article27. Yu L, Wen JK, Wang S, Wang WH, Yu JM, Ye XJ. Removal of calcified lumbar disc herniation with endoscopic-matched ultrasonic osteotome - our preliminary experience. Br J Neurosurg. 34:80–85. 2020.
Article28. Yu Y, Jiang Y, Xu F, Mao Y, Yuan L, Li C. Percutaneous full-endoscopic C2 ganglionectomy for the treatment of intractable occipital neuralgia: technical note. Oper Neurosurg (Hagerstown). 21:E472–E478. 2021.
Article29. Zheng C, Huang X, Yu J, Ye X. Posterior percutaneous endoscopic cervical diskectomy: a single-center experience of 252 cases. World Neurosurg. 120:e63–e67. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Posterior Cervical Inclinatory Foraminotomy for Spondylotic Radiculopathy Preliminary
- Posterior Endoscopic Cervical Decompression: Review and Technical Note
- Endoscope Assisted Anterior Cervical Foraminotomy
- Posterior Cervical Microscopic Foraminotomy and Discectomy with Laser for Unilateral Radiculopathy
- Comparison of Surgical Results between Soft Ruptured Disc and Foraminal Stenosis Patients in Posterior Cervical Laminoforaminotomy