J Stroke.
2023 May;25(2):291-298. 10.5853/jos.2023.00213.
Timing and Predictors of Recanalization After Anticoagulation in Cerebral Venous Thrombosis
- Affiliations
-
- 1Department of Neurology, University of Colorado School of Medicine, Aurora, CO, USA
- 2Department of Neurology, Warren Alpert School of Medicine at Brown University, Providence, RI, USA
- 3Clinical and Translational Neuroscience Unit, Department of Neurology, Feil Family Brain and Mind Research Institute, Weill Cornell Medicine, New York, NY, USA
- 4Department of Neurology, Yale University School of Medicine, New Haven, CT, USA
- 5Department of Neurology, University of Florida, Gainesville, FL, USA; and Department of Neurology, Cedars-Sinai Medical Center, Los Angeles, CA, USA
- 6Department of Neurology and Stroke Research Center Bern, University of Bern and University Hospital Bern, Bern, Switzerland
- 7University Institute of Diagnostic and Interventional Neuroradiology, Bern University Hospital, Inselspital, Bern, Switzerland
- 8Department of Neurology and Neurosurgery, Medical University of South Carolina, Charleston, SC, USA
- 9Department of Neurology, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
- 10Department of Medicine and Surgery, University of Perugia, Perugia, Italy
- 11Neurology–Stroke Unit, IRCCS MultiMedica, Milano, Italy
- 12Department of Neurology and UCLA Stroke Center, Los Angeles, CA, USA
- KMID: 2542480
- DOI: http://doi.org/10.5853/jos.2023.00213
Abstract
- Background and Purpose
Vessel recanalization after cerebral venous thrombosis (CVT) is associated with favorable outcomes and lower mortality. Several studies examined the timing and predictors of recanalization after CVT with mixed results. We aimed to investigate predictors and timing of recanalization after CVT.
Methods
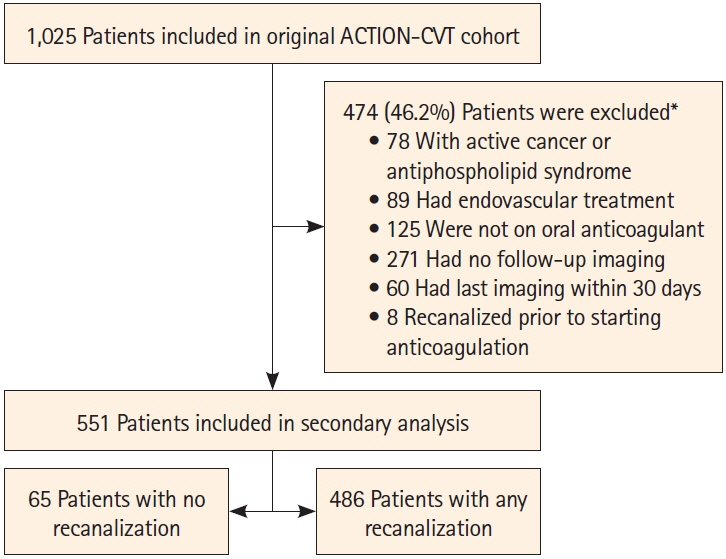
We used data from the multicenter, international AntiCoagulaTION in the Treatment of Cerebral Venous Thrombosis (ACTION-CVT) study of consecutive patients with CVT from January 2015 to December 2020. Our analysis included patients that had undergone repeat venous neuroimaging more than 30 days after initiation of anticoagulation treatment. Prespecified variables were included in univariate and multivariable analyses to identify independent predictors of failure to recanalize.
Results
Among the 551 patients (mean age, 44.4±16.2 years, 66.2% women) that met inclusion criteria, 486 (88.2%) had complete or partial, and 65 (11.8%) had no recanalization. The median time to first follow-up imaging study was 110 days (interquartile range, 60–187). In multivariable analysis, older age (odds ratio [OR], 1.05; 95% confidence interval [CI], 1.03–1.07), male sex (OR, 0.44; 95% CI, 0.24–0.80), and lack of parenchymal changes on baseline imaging (OR, 0.53; 95% CI, 0.29–0.96) were associated with no recanalization. The majority of improvement in recanalization (71.1%) occurred before 3 months from initial diagnosis. A high percentage of complete recanalization (59.0%) took place within the first 3 months after CVT diagnosis.
Conclusion
Older age, male sex, and lack of parenchymal changes were associated with no recanalization after CVT. The majority recanalization occurred early in the disease course suggesting limited further recanalization with anticoagulation beyond 3 months. Large prospective studies are needed to confirm our findings.
Figure
Reference
-
References
1. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F; ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis. Stroke. 2004; 35:664–670.
Article2. Saposnik G, Barinagarrementeria F, Brown RD Jr, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; 42:1158–1192.
Article3. Ferro JM, Coutinho JM, Dentali F, Kobayashi A, Alasheev A, Canhão P, et al. Safety and efficacy of dabigatran etexilate vs dose-adjusted warfarin in patients with cerebral venous thrombosis: a randomized clinical trial. JAMA Neurol. 2019; 76:1457–1465.
Article4. Stevens SM, Woller SC, Kreuziger LB, Bounameaux H, Doerschug K, Geersing GJ, et al. Antithrombotic therapy for VTE disease: second update of the chest guideline and expert panel report. Chest. 2021; 160:e545–e608.5. Ferro JM, Bendszus M, Jansen O, Coutinho JM, Dentali F, Kobayashi A, et al. Recanalization after cerebral venous thrombosis. A randomized controlled trial of the safety and efficacy of dabigatran etexilate versus dose-adjusted warfarin in patients with cerebral venous and dural sinus thrombosis. Int J Stroke. 2022; 17:189–197.
Article6. Aguiar de Sousa D, Lucas Neto L, Canhão P, Ferro JM. Recanalization in cerebral venous thrombosis. Stroke. 2018; 49:1828–1835.
Article7. Arauz A, Vargas-González JC, Arguelles-Morales N, Barboza MA, Calleja J, Martínez-Jurado E, et al. Time to recanalisation in patients with cerebral venous thrombosis under anticoagulation therapy. J Neurol Neurosurg Psychiatry. 2016; 87:247–251.
Article8. Herweh C, Griebe M, Geisbüsch C, Szabo K, Neumaier-Probst E, Hennerici MG, et al. Frequency and temporal profile of recanalization after cerebral vein and sinus thrombosis. Eur J Neurol. 2016; 23:681–687.
Article9. Gazioglu S, Eyuboglu I, Yildirim A, Aydin CO, Alioglu Z. Cerebral venous sinus thrombosis: clinical features, long-term outcome and recanalization. J Clin Neurosci. 2017; 45:248–251.
Article10. Putaala J, Hiltunen S, Salonen O, Kaste M, Tatlisumak T. Recanalization and its correlation to outcome after cerebral venous thrombosis. J Neurol Sci. 2010; 292:11–15.11. Krajícˇková D, Klzo L, Krajina A, Vyšata O, Herzig R, Vališ M. Cerebral venous sinus thrombosis: clinical characteristics and factors influencing clinical outcome. Clin Appl Thromb Hemost. 2016; 22:665–672.12. Aguiar de Sousa D, Lucas Neto L, Arauz A, Sousa AL, Gabriel D, Correia M, et al. Early recanalization in patients with cerebral venous thrombosis treated with anticoagulation. Stroke. 2020; 51:1174–1181.
Article13. Yaghi S, Shu L, Bakradze E, Salehi Omran S, Giles JA, Amar JY, et al. Direct oral anticoagulants versus warfarin in the treatment of cerebral venous thrombosis (ACTION-CVT): a multicenter international study. Stroke. 2022; 53:728–738.14. Sayar Z, Moll R, Isenberg D, Cohen H. Thrombotic antiphospholipid syndrome: a practical guide to diagnosis and management. Thromb Res. 2021; 198:213–221.
Article15. Lyman GH, Carrier M, Ay C, Di Nisio M, Hicks LK, Khorana AA, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021; 5:927–974.
Article16. Bates SM, Greer IA, Hirsh J, Ginsberg JS. Use of antithrombotic agents during pregnancy: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126(3 Suppl):627S–644S.17. Salehi Omran S, Hartman A, Zakai NA, Navi BB. Thrombophilia testing after ischemic stroke: why, when, and what? Stroke. 2021; 52:1874–1884.18. Ferro JM, Canhão P, Bousser MG, Stam J, Barinagarrementeria F; ISCVT Investigators. Cerebral vein and dural sinus thrombosis in elderly patients. Stroke. 2005; 36:1927–1932.
Article19. Liberman AL, Gialdini G, Bakradze E, Chatterjee A, Kamel H, Merkler AE. Misdiagnosis of cerebral vein thrombosis in the emergency department. Stroke. 2018; 49:1504–1506.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Three cases of mesenteric venous thrombosis treated by different modalities
- Treatment of the Superior Sagittal Sinus Thrombosis with the Mechanical Thrombectomy Using Stent-Retriever Device
- Predictor of Recanalization in Lower Extremity Deep Vein Thrombosis
- A Case of Deep Cerebral Venous Thrombosis Associated with Iron Deficiency Anemia
- Thrombosis and Recanalization of Small Saccular Cerebral Aneurysm : Two Case Reports and a Suggestion for Possible Mechanism