Korean J Transplant.
2023 Mar;37(1):57-62. 10.4285/kjt.22.0050.
The first successful eculizumab rescue therapy of a kidney transplant recipient with atypical hemolytic uremic syndrome in South Korea: a case report
- Affiliations
-
- 1Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 2Research Institute for Transplantation, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Pathology, Yonsei University College of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2541313
- DOI: http://doi.org/10.4285/kjt.22.0050
Abstract
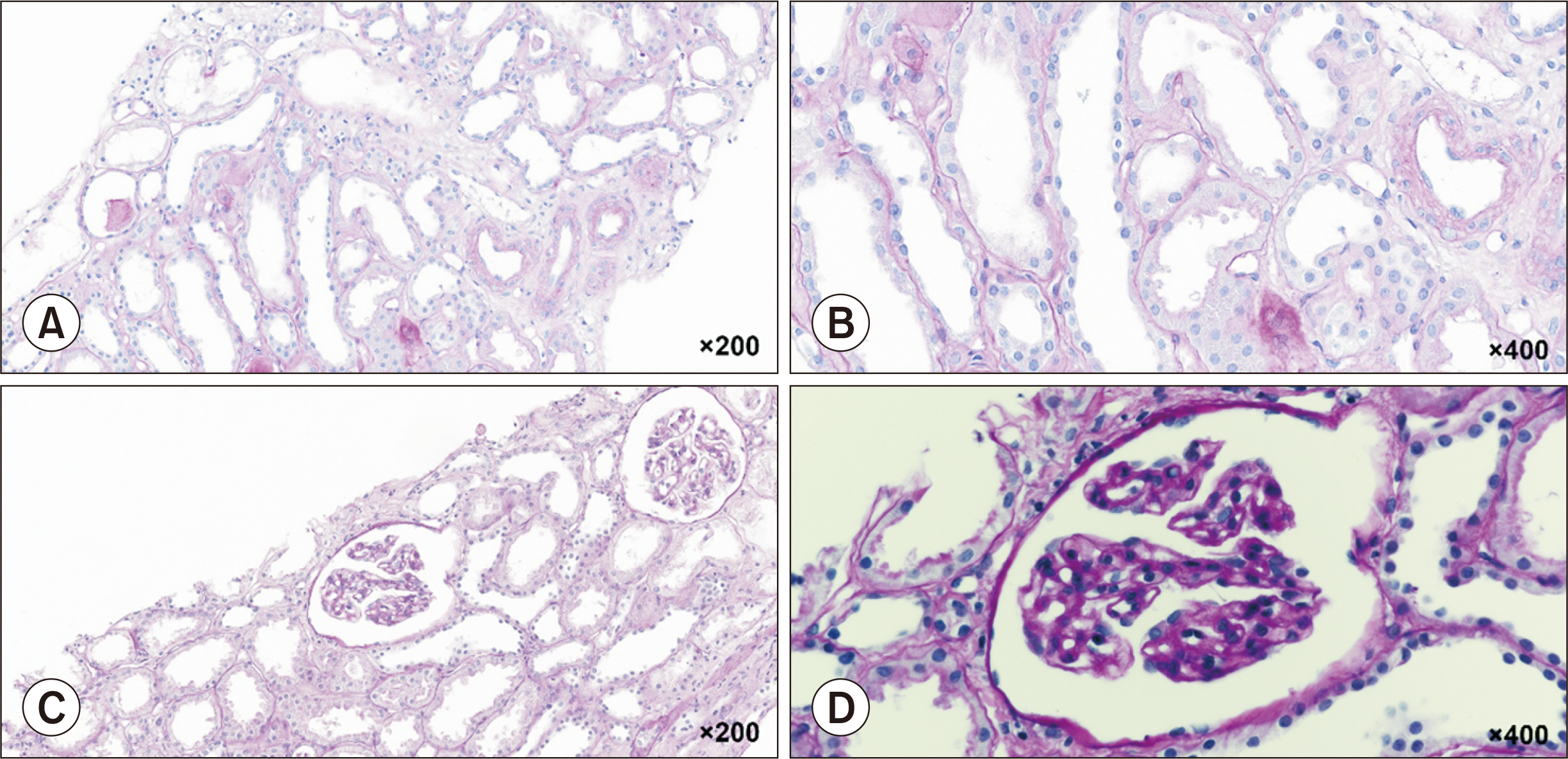
- Atypical hemolytic uremic syndrome (aHUS) is a form of thrombotic microangiopathy (TMA) that can result in end-stage renal disease. Patients with aHUS often have predisposing dysfunction in the complement pathway, and continuous activation of complement proteins can be triggered after transplantation. Here, we report the first successful case of aHUS treatment in a kidney transplant recipient with early use of a C5 inhibitor, eculizumab, in South Korea. The patient was a 32-year-old man, and the donor was his 60-year-old mother. The graft showed immediate good function. On postoperative day (POD) 3, the clinical diagnosis of TMA was made. Persistent renal dysfunction despite 10 plasma exchange (PE) sessions prompted eculizumab treatment on POD 18 under suspicion of aHUS. Next-generation sequencing reported gene mutations classified as variants of unknown significance in coagulation-associated genes. The patient was discharged after three doses of eculizumab with serum creatinine of 1.82 mg/dL. In total, 16 doses of eculizumab were administered. At the last follow-up, 21 months after eculizumab discontinuation, the graft was well functioning. De novo TMA after kidney transplantation can be caused by sustained activation of the complement pathway, and early eculizumab treatment appears important in the successful treatment of aHUS refractory to PE.
Keyword
Figure
Reference
-
1. Noris M, Remuzzi G. 2009; Atypical hemolytic-uremic syndrome. N Engl J Med. 361:1676–87. DOI: 10.1056/NEJMra0902814. PMID: 19846853.2. Le Clech A, Simon-Tillaux N, Provôt F, Delmas Y, Vieira-Martins P, Limou S, et al. 2019; Atypical and secondary hemolytic uremic syndromes have a distinct presentation and no common genetic risk factors. Kidney Int. 95:1443–52. DOI: 10.1016/j.kint.2019.01.023. PMID: 30982675.3. Ávila A, Gavela E, Sancho A. 2021; Thrombotic microangiopathy after kidney transplantation: an underdiagnosed and potentially reversible entity. Front Med (Lausanne). 8:642864. DOI: 10.3389/fmed.2021.642864. PMID: 33898482. PMCID: PMC8063690.4. Le Quintrec M, Lionet A, Kamar N, Karras A, Barbier S, Buchler M, et al. 2008; Complement mutation-associated de novo thrombotic microangiopathy following kidney transplantation. Am J Transplant. 8:1694–701. DOI: 10.1111/j.1600-6143.2008.02297.x. PMID: 18557729.
Article5. Portoles J, Huerta A, Arjona E, Gavela E, Agüera M, Jiménez C, et al. 2020; Characteristics, management and outcomes of atypical haemolytic uraemic syndrome in kidney transplant patients: a retrospective national study. Clin Kidney J. 14:1173–80. DOI: 10.1093/ckj/sfaa096. PMID: 33841863. PMCID: PMC8023214.6. Cavero T, Rabasco C, López A, Román E, Ávila A, Sevillano Á, et al. 2017; Eculizumab in secondary atypical haemolytic uraemic syndrome. Nephrol Dial Transplant. 32:466–74. DOI: 10.1093/ndt/gfw453. PMID: 28339660. PMCID: PMC5410989.7. Wilson CH, Brown AL, White SA, Goodship TH, Sheerin NS, Manas DM. 2011; Successful treatment of de novo posttransplant thrombotic microangiopathy with eculizumab. Transplantation. 92:e42–3. DOI: 10.1097/TP.0b013e318230c0bd. PMID: 21989273.8. Garg N, Rennke HG, Pavlakis M, Zandi-Nejad K. 2018; De novo thrombotic microangiopathy after kidney transplantation. Transplant Rev (Orlando). 32:58–68. DOI: 10.1016/j.trre.2017.10.001. PMID: 29157988.
Article9. Bu F, Zhang Y, Wang K, Borsa NG, Jones MB, Taylor AO, et al. 2018; Genetic analysis of 400 patients refines understanding and implicates a new gene in atypical hemolytic uremic syndrome. J Am Soc Nephrol. 29:2809–19. DOI: 10.1681/ASN.2018070759. PMID: 30377230. PMCID: PMC6287871.10. Brocklebank V, Wood KM, Kavanagh D. 2018; Thrombotic microangiopathy and the kidney. Clin J Am Soc Nephrol. 13:300–17. DOI: 10.2215/CJN.00620117. PMID: 29042465. PMCID: PMC5967417.11. Legendre CM, Licht C, Muus P, Greenbaum LA, Babu S, Bedrosian C, et al. 2013; Terminal complement inhibitor eculizumab in atypical hemolytic-uremic syndrome. N Engl J Med. 368:2169–81. DOI: 10.1056/NEJMoa1208981. PMID: 23738544.12. Goldenberg NA, Manco-Johnson MJ. 2008; Protein C deficiency. Haemophilia. 14:1214–21. DOI: 10.1111/j.1365-2516.2008.01838.x. PMID: 19141162.13. Amara U, Flierl MA, Rittirsch D, Klos A, Chen H, Acker B, et al. 2010; Molecular intercommunication between the complement and coagulation systems. J Immunol. 185:5628–36. DOI: 10.4049/jimmunol.0903678. PMID: 20870944. PMCID: PMC3123139.14. Goodship TH, Cook HT, Fakhouri F, Fervenza FC, Frémeaux-Bacchi V, Kavanagh D, et al. 2017; Atypical hemolytic uremic syndrome and C3 glomerulopathy: conclusions from a "Kidney Disease: Improving Global Outcomes" (KDIGO) Controversies Conference. Kidney Int. 91:539–51. DOI: 10.1016/j.kint.2016.10.005. PMID: 27989322.15. Fayek SA, Allam SR, Martinez E, Pan G, Dao A, Rofaiel G. 2020; Atypical hemolytic uremic syndrome after kidney transplantation: lessons learned from the good, the bad, and the ugly. A case series with literature review. Transplant Proc. 52:146–52. DOI: 10.1016/j.transproceed.2019.10.015. PMID: 31924403.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Eculizumab as rescue therapy in a kidney transplant recipient with atypical hemolytic uremic syndrome: a case report
- Atypical hemolytic uremic syndrome and eculizumab therapy in children
- Rapid Resolution of Atypical Hemolytic Uremic Syndrome by Eculizumab Treatment
- Eculizumab therapy for recurrent atypical hemolytic uremic syndrome after kidney transplantation in atypical hemolytic uremic syndrome: a case report
- An abscess formation on the transplanted graft and its successfully treatment in kidney transplantation recipient with de novo atypical hemolytic uremic syndrome treated with eculizumab: a case report