Blood Res.
2023 Mar;58(1):2-12. 10.5045/br.2023.2022192.
Effects of immune system cells in GvHD and corresponding therapeutic strategies
- Affiliations
-
- 1Department of Hematology, Tarbiat Modarres University of Medical Science, Tehran, Iran
- KMID: 2541059
- DOI: http://doi.org/10.5045/br.2023.2022192
Abstract
- Allogeneic tissue transplantation is one of the most effective treatments for several diseases and injuries, in particular, malignant and non-malignant hematological conditions. Following this procedure, transplanted tissue encounters various complications, one of the most serious being graft-versus-host disease (GvHD). The management of GvHD directly affects the success of transplantation and the survival rate of the patient; therefore, many studies have focused on GvHD prevention and control. This review briefly explains the transplantation process, causes of graft rejection, and importance of the human leukocyte antigen system. Initially, we address the pathophysiology and immunobiology of GvHD, the cells involved in this complication, the differences between chronic and acute GvHD, and the importance of graft-versus-leukemia. Interestingly, various types of immune cells are involved in GvHD pathogenesis. After explaining how these cells affect the GvHD process, we discuss the studies conducted to control and reduce GvHD symptoms.
Keyword
Figure
Reference
-
1. Sepetyi DP. 2020. Foundations of bioethics and biosafety: educational manual for independent work of students of the 1-st course of II international faculty [PhD dissertation]. Zaporizhzhia State Medical University;Zaporizhzhia, Ukraine: DOI: 10.2307/j.ctv14t48dw.10.2. Deshmukh CD, Baheti AM. 2020; Need, process and importance of organ transplantation. Asian J Pharm Pharmacol. 6:126–31. DOI: 10.31024/ajpp.2020.6.2.6.
Article3. Summers C, Sheth VS, Bleakley M. 2020; Minor histocompatibility antigen-specific T cells. Front Pediatr. 8:284. DOI: 10.3389/fped.2020.00284. PMID: 32582592. PMCID: PMC7283489. PMID: 37039864fddf445e856974d2baa770f3.
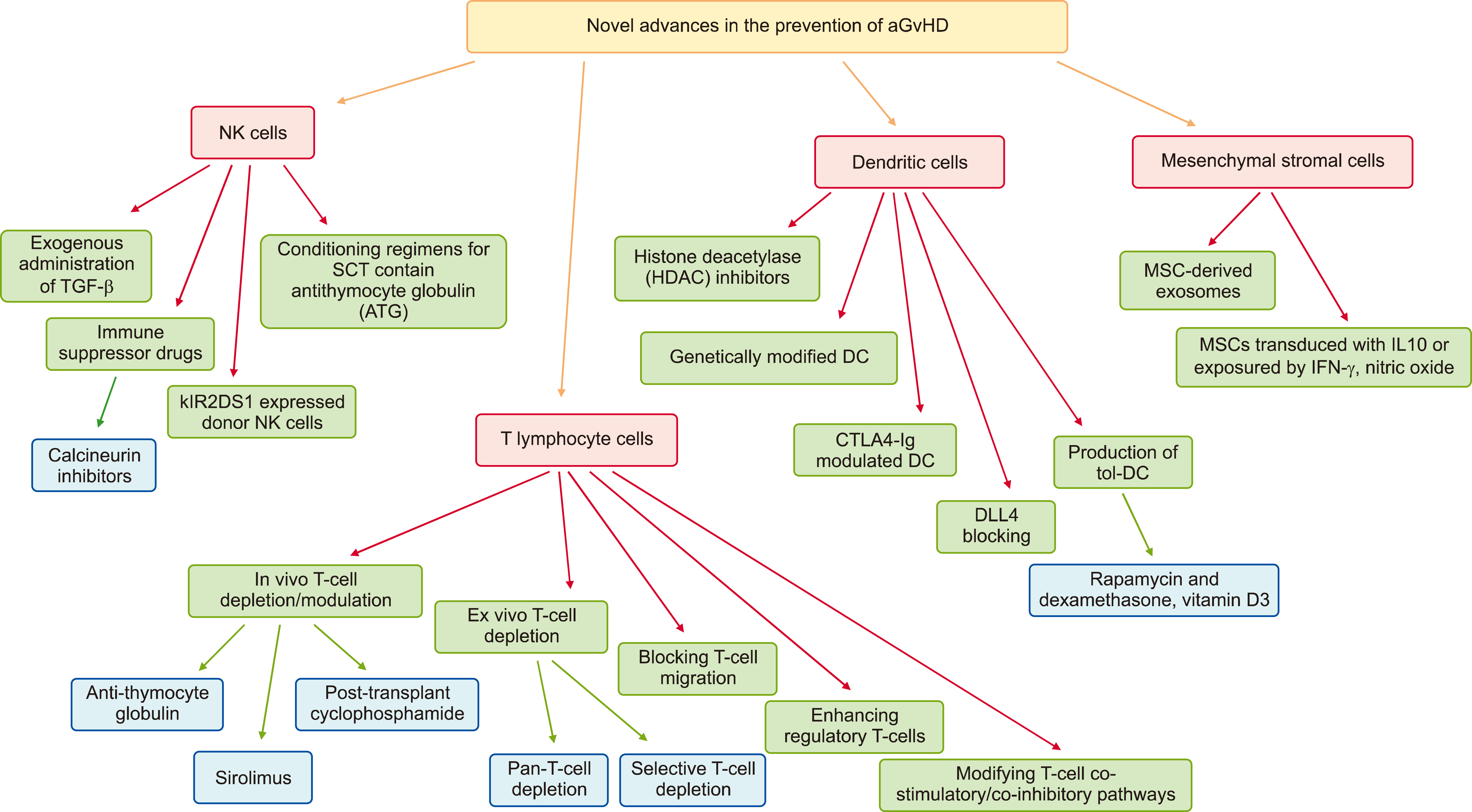
Article4. Socie G, Zeiser R, Blazar BR. 2018. Immune biology of allogeneic hematopoietic stem cell transplantation: models in discovery and translation. Academic Press;Cambridge, MA: DOI: 10.1016/c2016-0-03916-5.5. Zaghi E, Calvi M, Di Vito C, Mavilio D. 2019; Innate immune responses in the outcome of haploidentical hematopoietic stem cell trans-plantation to cure hematologic malignancies. Front Immunol. 10:2794. DOI: 10.3389/fimmu.2019.02794. PMID: 31849972. PMCID: PMC6892976. PMID: d7f0285922e740bfa336830ed555257a.
Article6. Perkey E, Maillard I. 2018; New insights into graft-versus-host disease and graft rejection. Annu Rev Pathol. 13:219–45. DOI: 10.1146/annurev-pathol-020117-043720. PMID: 29099650.
Article7. Gooptu M, Koreth J. 2020; Translational and clinical advances in acute graft-versus-host disease. Haematologica. 105:2550–60. DOI: 10.3324/haematol.2019.240309. PMID: 33054103. PMCID: PMC7604566.
Article8. Ryu J, Jhun J, Park MJ, et al. 2020; FTY720 ameliorates GvHD by blocking T lymphocyte migration to target organs and by skin fibrosis inhibition. J Transl Med. 18:225. DOI: 10.1186/s12967-020-02386-w. PMID: 32505218. PMCID: PMC7276082. PMID: 4b85431c3473421485553751faad8771.
Article9. Yu H, Tian Y, Wang Y, Mineishi S, Zhang Y. 2019; Dendritic cell regulation of graft-vs.-host disease: immunostimulation and tolerance. Front Immunol. 10:93. DOI: 10.3389/fimmu.2019.00093. PMID: 30774630. PMCID: PMC6367268. PMID: f6785630e3e648a0b9f648c7328d1a79.
Article10. Jaeger S. 2011. Hematopoietic stem cell research and transplantation: genesis, development and prospects for the 21st century [PhD dissertation]. Drew University;Madison, NJ:11. Banerjee S, Parasramka MA, Paruthy SB. Bharti AC, Aggarwal BB, editors. 2018. Garcinol: preclinical perspective underpinning chemo-and radiosensitization of cancer. Role of nutraceuticals in cancer chemosensitization. Elsevier;Philadelphia, PA: p. 297–324. DOI: 10.1016/B978-0-12-812373-7.00015-2. PMID: 29407111.
Article12. Sallman DA, Chaudhury A, Nguyen J, Zhang L. 2020. Handbook of hematologic malignancies. Demos Medical Publishing;New York, NY: p. 393. DOI: 10.1891/9780826149770.13. Nakamura R, Forman SJ. 2014; Reduced intensity conditioning for allogeneic hematopoietic cell transplantation: considerations for evidence-based GVHD prophylaxis. Expert Rev Hematol. 7:407–21. DOI: 10.1586/17474086.2014.898561. PMID: 24702163.
Article14. Dunne T. 2021. The effect of dual policy interventions on the rate of central venous catheter associated infections in adult stem cell transplant patients with hematological malignancy in Newfoundland and Labrador [thesis]. Memorial University of Newfoundland;St. John's, Canada:
Article15. Kuba A, Raida L. 2018; Graft versus host disease: from basic pathogenic principles to DNA damage response and cellular senescence. Mediators Inflamm. 2018:9451950. DOI: 10.1155/2018/9451950. PMID: 29785172. PMCID: PMC5896258. PMID: 8cc74fed7dde4cd88b7a30f50469dc9b.
Article16. Gooptu M, Antin JH. 2021; GVHD prophylaxis 2020. Front Immunol. 12:605726. DOI: 10.3389/fimmu.2021.605726. PMID: 33897681. PMCID: PMC8059368. PMID: e0cef7331d65442798a15c997248e682.
Article17. Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. 2019; Post-transplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Invest. 129:2357–73. DOI: 10.1172/JCI124218. PMID: 30913039. PMCID: PMC6546453.
Article18. Slavik JM, Lim DG, Burakoff SJ, Hafler DA. 2001; Uncoupling p70(s6) kinase activation and proliferation: rapamycin-resistant proliferation of human CD8(+) T lymphocytes. J Immunol. 166:3201–9. DOI: 10.4049/jimmunol.166.5.3201. PMID: 11207273.
Article19. Cutler C, Stevenson K, Kim HT, et al. 2008; Sirolimus is associated with veno-occlusive disease of the liver after myeloablative allogeneic stem cell transplantation. Blood. 112:4425–31. DOI: 10.1182/blood-2008-07-169342. PMID: 18776081. PMCID: PMC2597119.
Article20. Cutler C, Henry NL, Magee C, et al. 2005; Sirolimus and thrombotic microangiopathy after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 11:551–7. DOI: 10.1016/j.bbmt.2005.04.007. PMID: 15983555.
Article21. Solomon SR, Sanacore M, Zhang X, et al. 2014; Calcineurin inhibitor-free graft-versus-host disease prophylaxis with post-transplantation cyclophosphamide and brief-course sirolimus following reduced- intensity peripheral blood stem cell transplantation. Biol Blood Marrow Transplant. 20:1828–34. DOI: 10.1016/j.bbmt.2014.07.020. PMID: 25064745.22. Champlin RE, Passweg JR, Zhang MJ, et al. 2000; T-cell depletion of bone marrow transplants for leukemia from donors other than HLA-identical siblings: advantage of T-cell antibodies with narrow specificities. Blood. 95:3996–4003. PMID: 10845940.23. Wagner JE, Donnenberg AD, Noga SJ, et al. 1988; Lymphocyte depletion of donor bone marrow by counterflow centrifugal elutriation: results of a phase I clinical trial. Blood. 72:1168–76. DOI: 10.1182/blood.V72.4.1168.1168. PMID: 3048436.
Article24. Daniele N, Scerpa MC, Caniglia M, et al. 2012; Transplantation in the onco-hematology field: focus on the manipulation of αβ and γδ T cells. Pathol Res Pract. 208:67–73. DOI: 10.1016/j.prp.2011.10.006. PMID: 22115749.
Article25. Saad A, Lamb LS. 2017; Ex vivo T-cell depletion in allogeneic hemato-poietic stem cell transplant: past, present and future. Bone Marrow Transplant. 52:1241–8. DOI: 10.1038/bmt.2017.22. PMID: 28319073. PMCID: PMC5589981.
Article26. Pierini A, Alvarez M, Negrin RS. 2016; NK cell and CD4+FoxP3+ regulatory T cell based therapies for hematopoietic stem cell engraftment. Stem Cells Int. 2016:9025835. DOI: 10.1155/2016/9025835. PMID: 26880996. PMCID: PMC4736409. PMID: f22795edbb1d41fda7851087b48b6627.
Article27. Mankarious M, Matthews NC, Snowden JA, Alfred A. 2020; Extra-corporeal photopheresis (ECP) and the potential of novel biomarkers in optimizing management of acute and chronic graft vs. host disease (GvHD). Front Immunol. 11:81. DOI: 10.3389/fimmu.2020.00081. PMID: 32082329. PMCID: PMC7005102. PMID: 9d15e559695c4625ab1d2283f8c752fb.
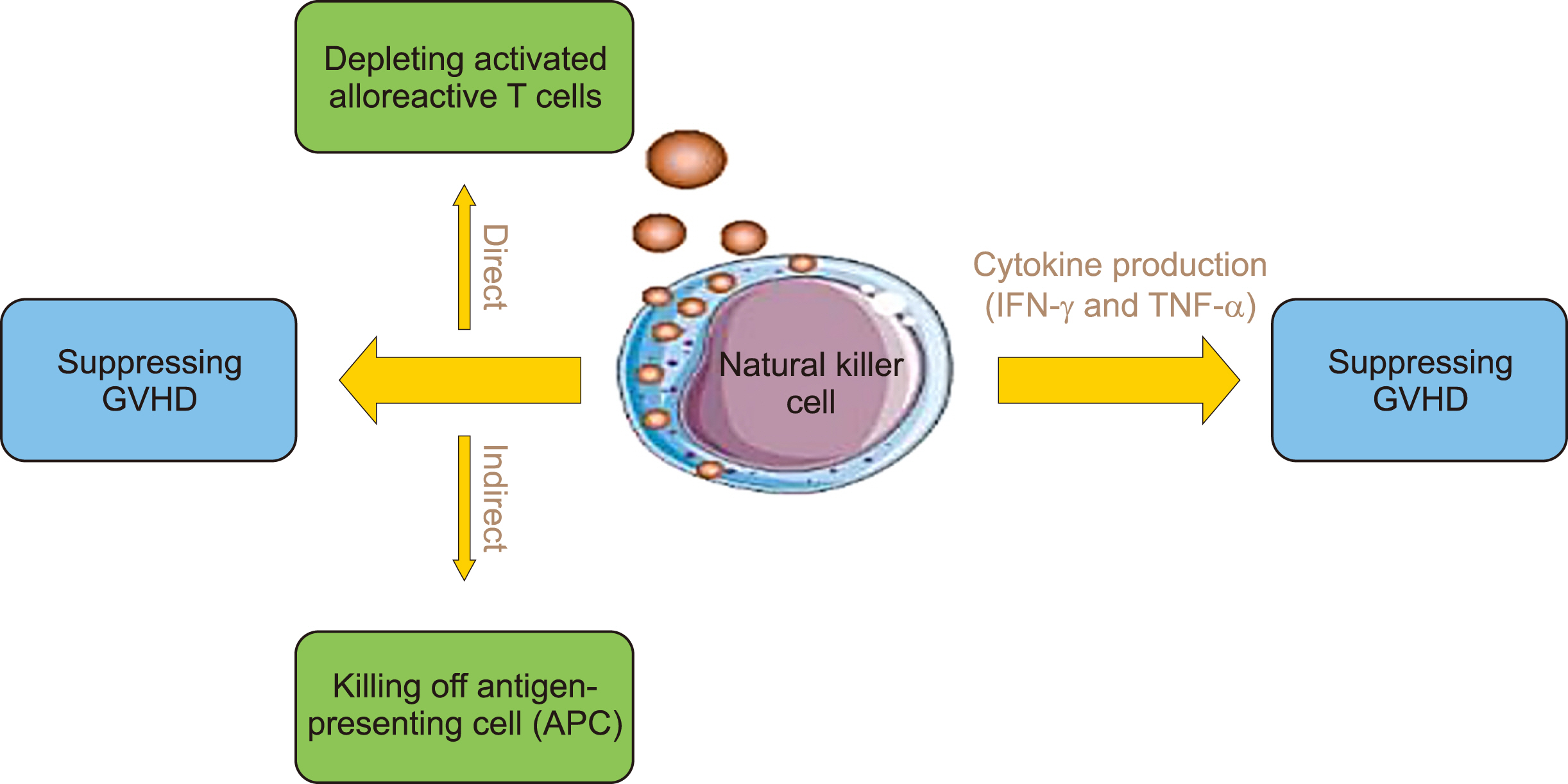
Article28. Simonetta F, Alvarez M, Negrin RS. 2017; Natural killer cells in graft-versus-host-disease after allogeneic hematopoietic cell transplantation. Front Immunol. 8:465. DOI: 10.3389/fimmu.2017.00465. PMID: 28487696. PMCID: PMC5403889. PMID: fd4335bb5bcd4101919bb44aac6b49fe.
Article29. Sheng L, Mu Q, Wu X, et al. 2020; Cytotoxicity of donor natural killer cells to allo-reactive T cells are related with acute graft-vs.-host-disease following allogeneic stem cell transplantation. Front Immunol. 11:1534. DOI: 10.3389/fimmu.2020.01534. PMID: 32849519. PMCID: PMC7411138. PMID: f7fff0794de24be48a4c78bd88f4a7f2.
Article30. Kheav VD, Busson M, Scieux C, et al. 2014; Favorable impact of natural killer cell reconstitution on chronic graft-versus-host disease and cytomegalovirus reactivation after allogeneic hematopoietic stem cell transplantation. Haematologica. 99:1860–7. DOI: 10.3324/haematol.2014.108407. PMID: 25085354. PMCID: PMC4258747.
Article31. Hu LJ, Zhao XY, Yu XX, et al. 2019; Quantity and quality reconstitution of NKG2A+ natural killer cells are associated with graft-versus- host disease after allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 25:1–11. DOI: 10.1016/j.bbmt.2018.08.008. PMID: 30142416.
Article32. Ullah MA, Hill GR, Tey SK. 2016; Functional reconstitution of natural killer cells in allogeneic hematopoietic stem cell transplantation. Front Immunol. 7:144. DOI: 10.3389/fimmu.2016.00144. PMID: 27148263. PMCID: PMC4831973. PMID: 4ac7cb40926b4b63b72b11db99f9d6f1.
Article33. Gao F, Ye Y, Gao Y, Huang H, Zhao Y. 2020; Influence of KIR and NK cell reconstitution in the outcomes of hematopoietic stem cell transplantation. Front Immunol. 11:2022. DOI: 10.3389/fimmu.2020.02022. PMID: 32983145. PMCID: PMC7493622. PMID: 18ff9102d1284f8fa1b9623881fc4819.
Article34. Akhavan Rahnama M, Soleimani M, Moradi N, Soufi Zomorrod M. 2017; Natural killer cell biology and its effect on graft versus host disease. Arch Med Lab Sci. 3:34–42.35. Kordelas L, Steckel NK, Horn PA, Beelen DW, Rebmann V. 2016; The activating NKG2C receptor is significantly reduced in NK cells after allogeneic stem cell transplantation in patients with severe graft-versus-host disease. Int J Mol Sci. 17:1797. DOI: 10.3390/ijms17111797. PMID: 27801784. PMCID: PMC5133798. PMID: 5d231179135e4e0581d34e6604c7e458.
Article36. Marofi F, Al-Awad AS, Sulaiman Rahman H, et al. 2021; CAR-NK cell: a new paradigm in tumor immunotherapy. Front Oncol. 11:673276. DOI: 10.3389/fonc.2021.673276. PMID: 34178661. PMCID: PMC8223062. PMID: 284a7d792cf64f698108ead3fa5b0fa5.
Article37. Nalle SC, Kwak HA, Edelblum KL, et al. 2014; Recipient NK cell inactivation and intestinal barrier loss are required for MHC- matched graft-versus-host disease. Sci Transl Med. 6:243ra87. DOI: 10.1126/scitranslmed.3008941. PMID: 24990882. PMCID: PMC4161673.
Article38. Ullrich E, Salzmann-Manrique E, Bakhtiar S, et al. 2016; Relation between acute GVHD and NK cell subset reconstitution following allogeneic stem cell transplantation. Front Immunol. 7:595. DOI: 10.3389/fimmu.2016.00595. PMID: 28066411. PMCID: PMC5177660.
Article39. Alvarez M, Bouchlaka MN, Sckisel GD, Sungur CM, Chen M, Murphy WJ. 2014; Increased antitumor effects using IL-2 with anti-TGF-β reveals competition between mouse NK and CD8 T cells. J Immunol. 193:1709–16. DOI: 10.4049/jimmunol.1400034. PMID: 25000978. PMCID: PMC4241855.
Article40. Barao I, Hanash AM, Hallett W, et al. 2006; Suppression of natural killer cell-mediated bone marrow cell rejection by CD4+ CD25+ regulatory T cells. Proc Natl Acad Sci U S A. 103:5460–5. DOI: 10.1073/pnas.0509249103. PMID: 16567639. PMCID: PMC1459377.41. Vacca P, Montaldo E, Croxatto D, et al. 2016; NK cells and other innate lymphoid cells in hematopoietic stem cell transplantation. Front Immunol. 7:188. DOI: 10.3389/fimmu.2016.00188. PMID: 27242795. PMCID: PMC4870263. PMID: 15b56aee13e6469b83e0dfda3aca0d74.
Article42. Bendall LJ, Bradstock KF. 2014; G-CSF: from granulopoietic stimulant to bone marrow stem cell mobilizing agent. Cytokine Growth Factor Rev. 25:355–67. DOI: 10.1016/j.cytogfr.2014.07.011. PMID: 25131807.
Article43. Minculescu L, Fischer-Nielsen A, Haastrup E, et al. 2020; Improved relapse-free survival in patients with high natural killer cell doses in grafts and during early immune reconstitution after allogeneic stem cell transplantation. Front Immunol. 11:1068. DOI: 10.3389/fimmu.2020.01068. PMID: 32547559. PMCID: PMC7273963. PMID: f35fe4bc13244fdfbb64076efd61d0ef.
Article44. Chang YJ, Zhao XY, Huang XJ. 2018; Strategies for enhancing and preserving anti-leukemia effects without aggravating graft- versus-host disease. Front Immunol. 9:3041. DOI: 10.3389/fimmu.2018.03041. PMID: 30619371. PMCID: PMC6308132. PMID: 1a7a73d389014a468cc373337079deca.45. Zhang P, Yang S, Zou Y, et al. 2019; NK cell predicts the severity of acute graft-versus-host disease in patients after allogeneic stem cell transplantation using antithymocyte globulin (ATG) in pretreat-ment scheme. BMC Immunol. 20:46. DOI: 10.1186/s12865-019-0326-8. PMID: 31818250. PMCID: PMC6902350. PMID: ca34effc4ecd42bd9de9305eaac09b2a.
Article46. Van Elssen CHMJ, Ciurea SO. 2020; NK cell alloreactivity in acute myeloid leukemia in the post-transplant cyclophosphamide era. Am J Hematol. 95:1590–8. DOI: 10.1002/ajh.25983. PMID: 32857869.
Article47. Bosch M, Dhadda M, Hoegh-Petersen M, et al. 2012; Immune re-constitution after anti-thymocyte globulin-conditioned hemato-poietic cell transplantation. Cytotherapy. 14:1258–75. DOI: 10.3109/14653249.2012.715243. PMID: 22985195. PMCID: PMC3681879.
Article48. Penack O, Fischer L, Gentilini C, et al. 2007; The type of ATG matters-natural killer cells are influenced differentially by Thymoglobulin, Lymphoglobulin and ATG-Fresenius. Transpl Immunol. 18:85–7. DOI: 10.1016/j.trim.2007.05.001. PMID: 18005849.49. Heatley SL, Mullighan CG, Doherty K, et al. 2018; Activating KIR haplotype influences clinical outcome following HLA-matched sibling hematopoietic stem cell transplantation. HLA. 92:74–82. DOI: 10.1111/tan.13327. PMID: 29943500.
Article50. Ruggeri L, Vago L, Eikema DJ, et al. 2021; Natural killer cell alloreactivity in HLA-haploidentical hematopoietic transplantation: a study on behalf of the CTIWP of the EBMT. Bone Marrow Transplant. 56:1900–7. DOI: 10.1038/s41409-021-01259-0. PMID: 33767404.
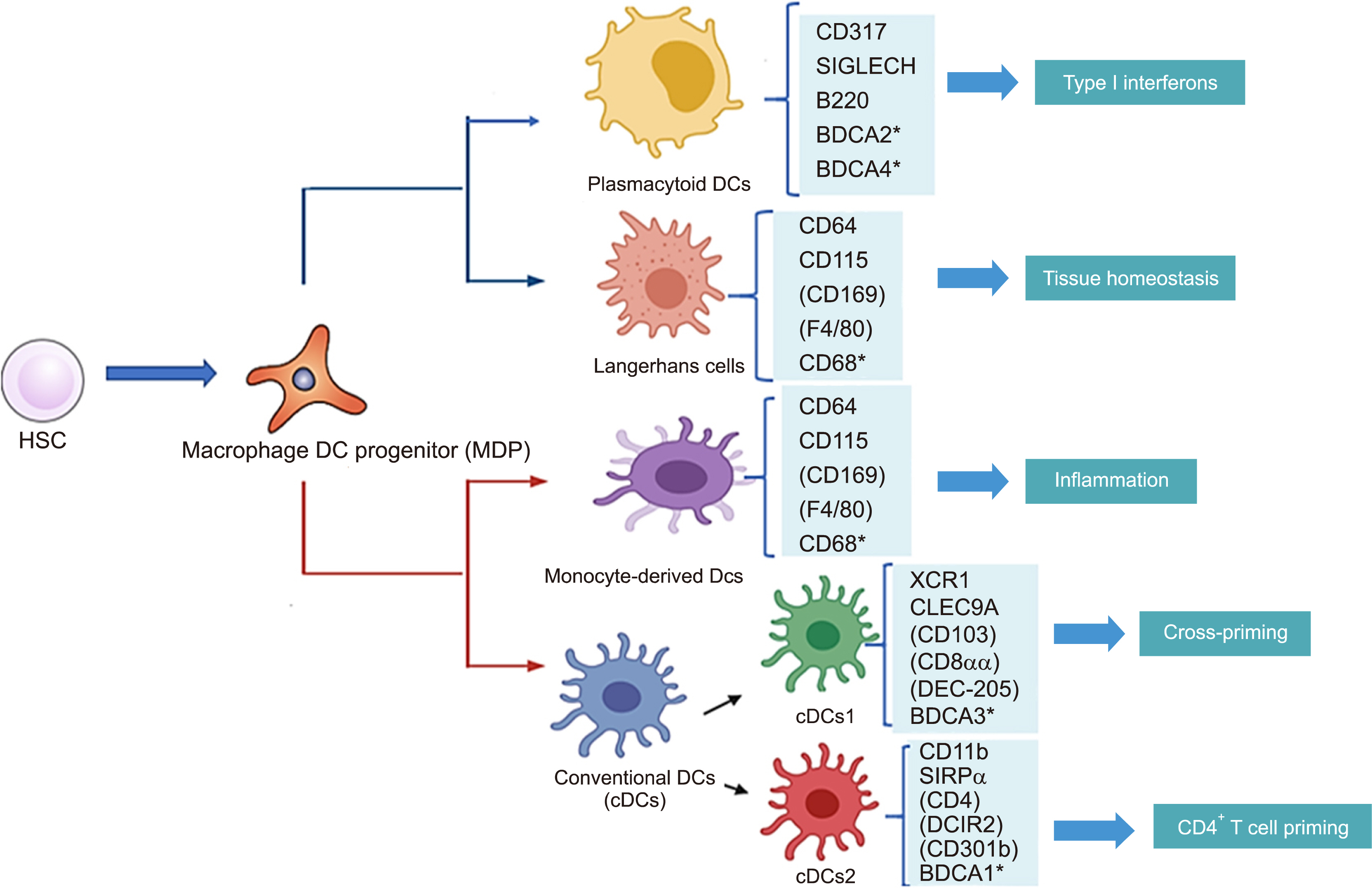
Article51. Merad M, Sathe P, Helft J, Miller J, Mortha A. 2013; The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu Rev Immunol. 31:563–604. DOI: 10.1146/annurev-immunol-020711-074950. PMID: 23516985. PMCID: PMC3853342.
Article52. Thomson AW, Metes DM, Ezzelarab MB, Raïch-Regué D. 2019; Regulatory dendritic cells for human organ transplantation. Transplant Rev (Orlando). 33:130–6. DOI: 10.1016/j.trre.2019.05.001. PMID: 31130302. PMCID: PMC6599577.53. Balan S, Saxena M, Bhardwaj N. 2019; Dendritic cell subsets and locations. Int Rev Cell Mol Biol. 348:1–68. DOI: 10.1016/bs.ircmb.2019.07.004. PMID: 31810551.
Article54. Giebel B, Kordelas L, Börger V. 2017; Clinical potential of mesenchymal stem/stromal cell-derived extracellular vesicles. Stem Cell Investig. 4:84. DOI: 10.21037/sci.2017.09.06. PMID: 29167805. PMCID: PMC5676188.55. Constantino J, Gomes C, Falcão A, Neves BM, Cruz MT. 2017; Dendritic cell-based immunotherapy: a basic review and recent advances. Immunol Res. 65:798–810. DOI: 10.1007/s12026-017-8931-1. PMID: 28660480.
Article56. Torres-Aguilar H, Aguilar-Ruiz SR, González-Pérez G, et al. 2010; Tolerogenic dendritic cells generated with different immuno-suppressive cytokines induce antigen-specific anergy and regulatory properties in memory CD4+ T cells. J Immunol. 184:1765–75. DOI: 10.4049/jimmunol.0902133. PMID: 20083662.
Article57. Anderson BE, McNiff JM, Jain D, Blazar BR, Shlomchik WD, Shlomchik MJ. 2005; Distinct roles for donor- and host-derived antigen-presenting cells and costimulatory molecules in murine chronic graft-versus-host disease: requirements depend on target organ. Blood. 105:2227–34. DOI: 10.1182/blood-2004-08-3032. PMID: 15522961.
Article58. Zhuang Q, Cai H, Cao Q, Li Z, Liu S, Ming Y. 2020; Tolerogenic dendritic cells: the pearl of immunotherapy in organ transplantation. Front Immunol. 11:552988. DOI: 10.3389/fimmu.2020.552988. PMID: 33123131. PMCID: PMC7573100. PMID: bbe1173f035049b8b89ab83d6325ad8e.
Article59. Stenger EO, Turnquist HR, Mapara MY, Thomson AW. 2012; Dendritic cells and regulation of graft-versus-host disease and graft-versus- leukemia activity. Blood. 119:5088–103. DOI: 10.1182/blood-2011-11-364091. PMID: 22403259. PMCID: PMC3369606.60. Tian Y, Meng L, Wang Y, et al. 2021; Graft-versus-host disease depletes plasmacytoid dendritic cell progenitors to impair tolerance induction. J Clin Invest. 131:e136774. DOI: 10.1172/JCI136774. PMID: 33090973. PMCID: PMC7773406.
Article61. Liang W, Chen X, Zhang S, et al. 2021; Mesenchymal stem cells as a double-edged sword in tumor growth: focusing on MSC-derived cytokines. Cell Mol Biol Lett. 26:3. DOI: 10.1186/s11658-020-00246-5. PMID: 33472580. PMCID: PMC7818947. PMID: 3cdfe2a033a84edf8a509de3c0502671.
Article62. Ringdén O, Gustafsson B, Sadeghi B. 2020; Mesenchymal stromal cells in pediatric hematopoietic cell transplantation a review and a pilot study in children treated with decidua stromal cells for acute graft-versus-host disease. Front Immunol. 11:567210. DOI: 10.3389/fimmu.2020.567210. PMID: 33193339. PMCID: PMC7604265. PMID: 012253a2f15b436799e05579532a9163.
Article63. Phinney DG. 2012; Functional heterogeneity of mesenchymal stem cells: implications for cell therapy. J Cell Biochem. 113:2806–12. DOI: 10.1002/jcb.24166. PMID: 22511358.
Article64. Crippa S, Bernardo ME. 2018; Mesenchymal stromal cells: role in the BM niche and in the support of hematopoietic stem cell trans-plantation. Hemasphere. 2:e151. DOI: 10.1097/HS9.0000000000000151. PMID: 31723790. PMCID: PMC6745957. PMID: 6bfa8f1e0a8e4eb2b62cb62a4a2a55f8.
Article65. Conrad S, Younsi A, Bauer C, Geburek F, Skutella T. Pham PV, editor. 2019. Mesenchymal stem cell-derived extracellular vesicles as mediators of anti- inflammatory effects. Stem cell transplantation for autoimmune diseases and inflammation. Springer;Philadelphia, PA: p. 89–123. DOI: 10.1007/978-3-030-23421-8_6.
Article66. Winer JP, Janmey PA, McCormick ME, Funaki M. 2009; Bone marrow- derived human mesenchymal stem cells become quiescent on soft substrates but remain responsive to chemical or mechanical stimuli. Tissue Eng Part A. 15:147–54. DOI: 10.1089/ten.tea.2007.0388. PMID: 18673086.67. Maumus M, Rozier P, Boulestreau J, Jorgensen C, Noël D. 2020; Mesenchymal stem cell-derived extracellular vesicles: opportunities and challenges for clinical translation. Front Bioeng Biotechnol. 8:997. DOI: 10.3389/fbioe.2020.00997. PMID: 33015001. PMCID: PMC7511661. PMID: e4b6b7075d9f4d198fd9c468b251587f.
Article68. Cheung TS, Bertolino GM, Giacomini C, Bornhäuser M, Dazzi F, Galleu A. 2020; Mesenchymal stromal cells for graft versus host disease: mechanism-based biomarkers. Front Immunol. 11:1338. DOI: 10.3389/fimmu.2020.01338. PMID: 32670295. PMCID: PMC7330053. PMID: 7285e8577afd49409d7815f303b6382f.
Article69. Vanherwegen AS, Cook DP, Ferreira GB, Gysemans C, Mathieu C. 2019; Vitamin D-modulated dendritic cells delay lethal graft-versus- ost disease through induction of regulatory T cells. J Steroid Biochem Mol Biol. 188:103–10. DOI: 10.1016/j.jsbmb.2018.12.013. PMID: 30605776.70. Ballini A, Cantore S, Scacco S, Coletti D, Tatullo M. 2018; Mesenchymal stem cells as promoters, enhancers, and playmakers of the trans-lational regenerative medicine 2018. Stem Cells Int. 2018:927401. DOI: 10.1155/2018/6927401. PMID: 30510586. PMCID: PMC6232791. PMID: 204d0bb084f54a99be485903a5c51958.
Article71. Charbord P. 2010; Bone marrow mesenchymal stem cells: historical overview and concepts. Hum Gene Ther. 21:1045–56. DOI: 10.1089/hum.2010.115. PMID: 20565251. PMCID: PMC4823383.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Pre-conditioning Dose on the Immune Kinetics and Cytokine Production in the Leukocytes Infiltrating GVHD Tissues after MHC-matched Transplantation
- Intervention with costimulatory pathways as a therapeutic approach for graft-versus-host disease
- Interactions between Immune Cells and Tumor Cells
- The Strategies for the Prevention of Chronic GVHD in Hematopoietic Stem Cell Transplantation
- Roles of Host Nonhematopoietic Cells in Autoimmunity and Donor Cell Engraftment in Graft-versus-host Disease