Clin Endosc.
2023 Mar;56(2):245-251. 10.5946/ce.2021.076.
Colorectal carcinoma and chronic inflammatory demyelinating polyneuropathy: is there a possible paraneoplastic association?
- Affiliations
-
- 1Loyola University Medical Center, Maywood, IL, USA
- 2Allama Iqbal Medical College, Lahore, Pakistan
- 3Services Institute of Medical Sciences, Lahore, Pakistan
- 4Marshfield Clinic, Marshfield, WI, USA
- 5Islamic International Medical College, Rawalpindi, Pakistan
- 6Sunrise Hospital and Medical Center, Las Vegas, NV, USA
- KMID: 2540743
- DOI: http://doi.org/10.5946/ce.2021.076
Abstract
- A plethora of paraneoplastic syndromes have been reported as remote effects of colorectal carcinoma (CRC). However, there is a dearth of data pertaining to the association of this cancer with demyelinating neuropathies. Herein, we describe the case of a young woman diagnosed with chronic inflammatory demyelinating polyneuropathy (CIDP). Treatment with intravenous immunoglobulins and prednisone did not improve her condition, and her neurological symptoms worsened. Subsequently, she was readmitted with exertional dyspnea, lightheadedness, malaise, and black stools. Colonoscopy revealed a necrotic mass in the ascending colon, which directly invaded the second part of the duodenum. Pathologic results confirmed the diagnosis of locally advanced CRC. Upon surgical resection of the cancer, her CIDP showed dramatic resolution without any additional therapy. Patients with CRC may develop CIDP as a type of paraneoplastic syndrome. Clinicians should remain cognizant of this potential association, as it is of paramount importance for the necessary holistic clinical management.
Keyword
Figure
Reference
-
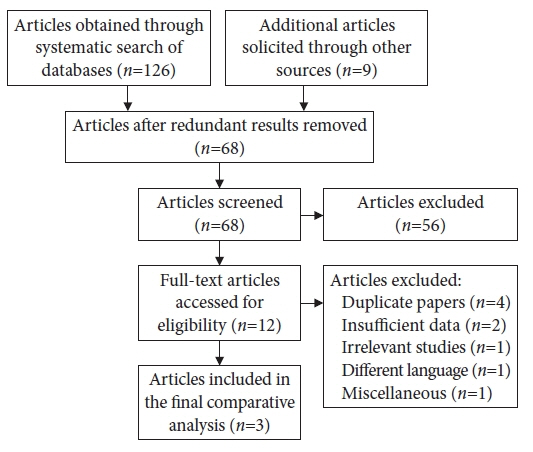
1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.2. Dyck PJ, Lais AC, Ohta M, et al. Chronic inflammatory polyradiculoneuropathy. Mayo Clin Proc. 1975; 50:621–637.3. Broers MC, Bunschoten C, Nieboer D, et al. Incidence and prevalence of chronic inflammatory demyelinating polyradiculoneuropathy: a systematic review and meta-analysis. Neuroepidemiology. 2019; 52:161–172.4. Malik A, Berry R, Fung BM, et al. Association between chronic inflammatory demyelinating polyneuropathy and gastrointestinal malignancies. Clin J Gastroenterol. 2021; 14:1–13.5. Rajabally YA, Attarian S. Chronic inflammatory demyelinating polyneuropathy and malignancy: a systematic review. Muscle Nerve. 2018; 57:875–883.6. Antoine JC, Mosnier JF, Lapras J, et al. Chronic inflammatory demyelinating polyneuropathy associated with carcinoma. J Neurol Neurosurg Psychiatry. 1996; 60:188–190.7. Ayyappan S, Day T, Kiers L. Distal acquired demyelinating symmetric (DADS) neuropathy associated with colorectal adenocarcinoma. Muscle Nerve. 2015; 51:928–931.8. Galassi G, Luppi G. Distal acquired demyelinating symmetric neuropathy associated with colorectal adenocarcinoma: should it be termed paraneoplastic? Muscle Nerve. 2016; 53:658–659.9. Bell CE, Seetharam S. Identification of the Schwann cell as a peripheral nervous system cell possessing a differentiation antigen expressed by a human lung tumor. J Immunol. 1977; 118:826–831.10. Kudo M, Noguchi T. Immunoreactive myelin basic protein in tumor cells associated with carcinomatous neuropathy. Am J Clin Pathol. 1985; 84:741–743.11. Altermatt HJ, Rodriguez M, Scheithauer BW, et al. Paraneoplastic anti-Purkinje and type I anti-neuronal nuclear autoantibodies bind selectively to central, peripheral, and autonomic nervous system cells. Lab Invest. 1991; 65:412–420.12. Fuller GN, Spies JM, Pollard JD, et al. Demyelinating neuropathies triggered by melanoma immunotherapy. Neurology. 1994; 44:2404–2405.13. Henry K. Paraneoplastic syndromes: definitions, classification, pathophysiology and principles of treatment. Semin Diagn Pathol. 2019; 36:204–210.14. Jameson JL, Longo DL. Paraneoplastic syndromes: endocrinologic/hematologic. In : Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, editors. Harrison’s Principles of Internal Medicine. 20th ed. McGraw-Hill Education;2018.15. Bunschoten C, Jacobs BC, Van den Bergh PYK, et al. Progress in diagnosis and treatment of chronic inflammatory demyelinating polyradiculoneuropathy. Lancet Neurol. 2019; 18:784–794.16. Van den Bergh PYK, Hadden RDM, Bouche P, et al. European Federation of Neurological Societies/Peripheral Nerve Society guideline on management of chronic inflammatory demyelinating polyradiculoneuropathy: report of a joint task force of the European Federation of Neurological Societies and the Peripheral Nerve Society-first revision. Eur J Neurol. 2010; 17:356–363.17. Breiner A, Brannagan TH. Comparison of sensitivity and specificity among 15 criteria for chronic inflammatory demyelinating polyneuropathy. Muscle Nerve. 2014; 50:40–46.18. Kuwabara S, Misawa S. Chronic inflammatory demyelinating polyneuropathy. Adv Exp Med Biol. 2019; 1190:333–343.19. Benson AB, Venook AP, Al-Hawary MM, et al. NCCN guidelines insights: colon cancer, version 2.2018. J Natl Compr Canc Netw. 2018; 16:359–369.20. Kakushadze Z, Raghubanshi R, Yu W. Estimating cost savings from early cancer diagnosis. Data. 2017; 2:30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Relaxation (Pseudomyotonia) as the Only Clinical Manifestation of Chronic Inflammatory Demyelinating Polyneuropathy
- Interpretation of Electrodiagnostic Tests in Chronic Inflammatory Demyelinating Polyneuropathy: Classification Using Nerve Conduction Study
- Subacute Inflammatory Demyelinating Polyneuropathy Combined with Optic Neuritis
- Chronic Inflammatory Demyelinating Polyneuropathy Combined With Limited Cutaneous Systemic Sclerosis
- Chronic Inflammatory Demyelinating Polyneuropathy Developed during Interferon-beta Therapy in a Patient with Multiple Sclerosis