Endocrinol Metab.
2023 Feb;38(1):34-42. 10.3803/EnM.2022.1649.
Overcoming Therapeutic Inertia as the Achilles’ Heel for Improving Suboptimal Diabetes Care: An Integrative Review
- Affiliations
-
- 1Department of Family Medicine, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Malaysia
- 2Clinical Research Unit, Hospital Pengajar Universiti Putra Malaysia (HPUPM Teaching Hospital), Persiaran MARDI-UPM, Malaysia
- 3Department of Dietetics, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia, Serdang, Malaysia
- 4Department of Primary Care Medicine, Faculty of Medicine, University of Malaya, Kuala Lumpur, Malaysia
- 5National Institute for Health Research Applied Research Collaboration East Midlands, Leicester Diabetes Centre, UK
- 6Diabetes Research Centre, Leicester General Hospital, University of Leicester, Leicester, UK
- KMID: 2539815
- DOI: http://doi.org/10.3803/EnM.2022.1649
Abstract
- The ultimate purpose of diabetes care is achieving the outcomes that patients regard as important throughout the life course. Despite advances in pharmaceuticals, nutraceuticals, psychoeducational programs, information technologies, and digital health, the levels of treatment target achievement in people with diabetes mellitus (DM) have remained suboptimal. This clinical care of people with DM is highly challenging, complex, costly, and confounded for patients, physicians, and healthcare systems. One key underlying problem is clinical inertia in general and therapeutic inertia (TI) in particular. TI refers to healthcare providers’ failure to modify therapy appropriately when treatment goals are not met. TI therefore relates to the prescribing decisions made by healthcare professionals, such as doctors, nurses, and pharmacists. The known causes of TI include factors at the level of the physician (50%), patient (30%), and health system (20%). Although TI is often multifactorial, the literature suggests that 28% of strategies are targeted at multiple levels of causes, 38% at the patient level, 26% at the healthcare professional level, and only 8% at the healthcare system level. The most effective interventions against TI are shorter intervals until revisit appointments and empowering nurses, diabetes educators, and pharmacists to review treatments and modify prescriptions.
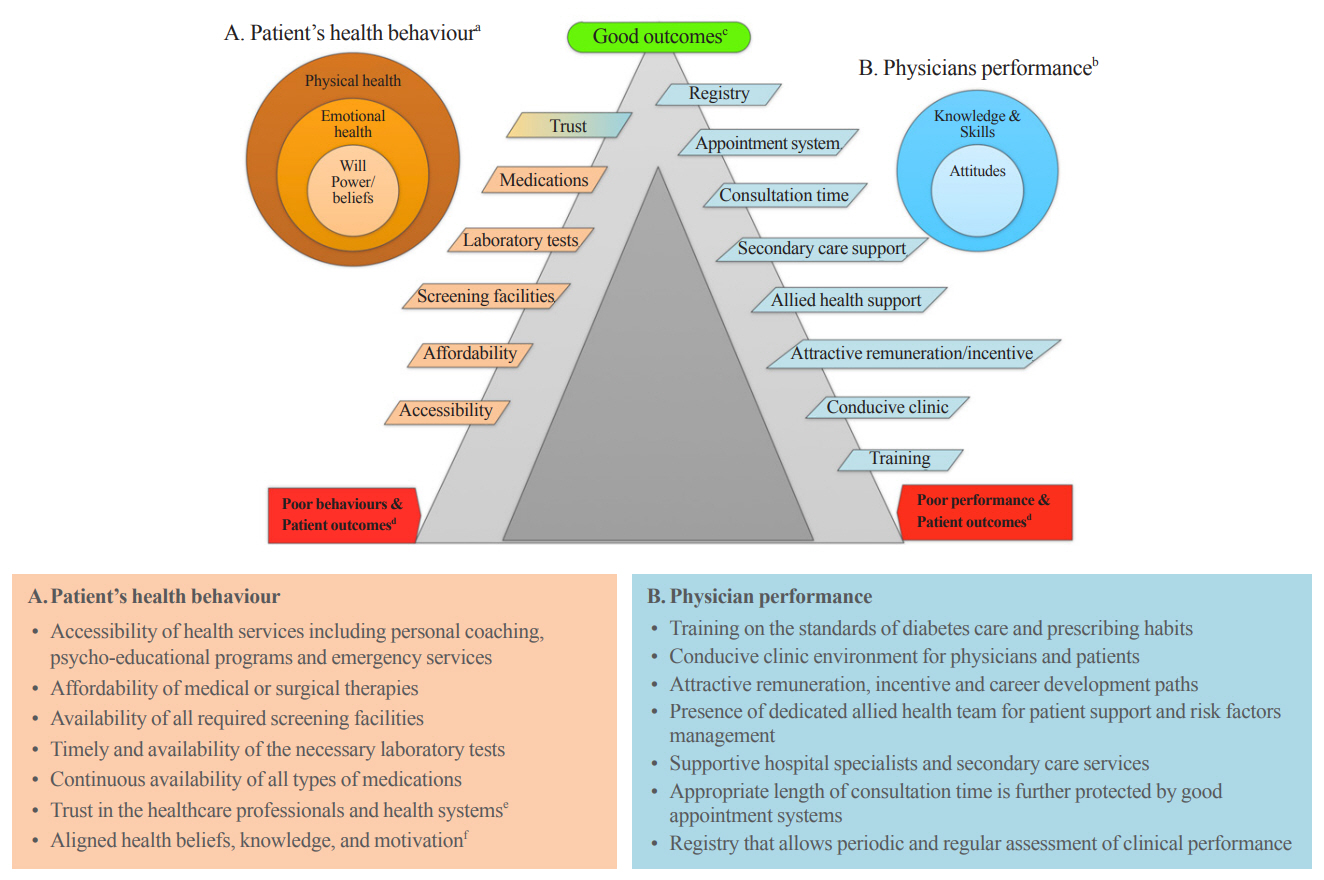
Figure
Reference
-
1. International Diabetes Federation. IDF Diabetes Atlas 2021. 10th ed. Brussels: IDF;2021. [cited 2023 Feb 9]. Available from: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf.2. Chan JC, Gagliardino JJ, Baik SH, Chantelot JM, Ferreira SR, Hancu N, et al. Multifaceted determinants for achieving glycemic control: the International Diabetes Management Practice Study (IDMPS). Diabetes Care. 2009; 32:227–33.3. Goh CC, Koh KH, Goh S, Koh Y, Tan NC. Achieving triple treatment goals in multi-ethnic Asian patients with type 2 diabetes mellitus in primary care. Malays Fam Physician. 2018; 13:10–8.4. Khunti K, Gomes MB, Pocock S, Shestakova MV, Pintat S, Fenici P, et al. Therapeutic inertia in the treatment of hyperglycaemia in patients with type 2 diabetes: a systematic review. Diabetes Obes Metab. 2018; 20:427–37.
Article5. Edelman SV, Polonsky WH. Type 2 diabetes in the real world: the elusive nature of glycemic control. Diabetes Care. 2017; 40:1425–32.
Article6. Hussain S, Chowdhury TA. The impact of comorbidities on the pharmacological management of type 2 diabetes mellitus. Drugs. 2019; 79:231–42.
Article7. Seidu S, Cos X, Brunton S, Harris SB, Jansson SP, Mata-Cases M, et al. 2022 Update to the position statement by Primary Care Diabetes Europe: a disease state approach to the pharmacological management of type 2 diabetes in primary care. Prim Care Diabetes. 2022; 16:223–44.
Article8. Gabbay RA, Kendall D, Beebe C, Cuddeback J, Hobbs T, Khan ND, et al. Addressing therapeutic inertia in 2020 and beyond: a 3-year initiative of the American Diabetes Association. Clin Diabetes. 2020; 38:371–81.
Article9. Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of hyperglycemia in type 2 diabetes, 2022: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022; 45:2753–86.
Article10. Chew BH, Vos RC, Widyahening IS, Khunti K. Editorial: Achieving efficient diabetes care through understanding the risk factors, markers, and patient experiences. Front Endocrinol (Lausanne). 2022; 13:854167.
Article11. Bailey CJ, Kodack M. Patient adherence to medication requirements for therapy of type 2 diabetes. Int J Clin Pract. 2011; 65:314–22.
Article12. Chan JC, So W, Ma RC, Tong PC, Wong R, Yang X. The complexity of vascular and non-vascular complications of diabetes: the Hong Kong Diabetes Registry. Curr Cardiovasc Risk Rep. 2011; 5:230–9.
Article13. Chew BH, Shariff-Ghazali S, Fernandez A. Psychological aspects of diabetes care: effecting behavioral change in patients. World J Diabetes. 2014; 5:796–808.
Article14. Khunti K, Kosiborod M, Ray KK. Legacy benefits of blood glucose, blood pressure and lipid control in individuals with diabetes and cardiovascular disease: time to overcome multifactorial therapeutic inertia? Diabetes Obes Metab. 2018; 20:1337–41.
Article15. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-Year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008; 359:1577–89.
Article16. Jermendy G. Vascular memory: can we broaden the concept of the metabolic memory? Cardiovasc Diabetol. 2012; 11:44.
Article17. American Diabetes Association. Standards of care in diabetes-2023. Diabetes Care. 2023; 46(Suppl 1):S1–291.18. Lee YK, Low WY, Ng CJ. Exploring patient values in medical decision making: a qualitative study. PLoS One. 2013; 8:e80051.
Article19. Reach G. Clinical inertia, uncertainty and individualized guidelines. Diabetes Metab. 2014; 40:241–5.
Article20. Chang S, Lee TH. Beyond evidence-based medicine. N Engl J Med. 2018; 379:1983–5.
Article21. Del Prato S, Felton AM, Munro N, Nesto R, Zimmet P, Zinman B, et al. Improving glucose management: ten steps to get more patients with type 2 diabetes to glycaemic goal. Int J Clin Pract. 2005; 59:1345–55.
Article22. McGill M, Felton AM; Global Partnership for Effective Diabetes Management. New global recommendations: a multidisciplinary approach to improving outcomes in diabetes. Prim Care Diabetes. 2007; 1:49–55.
Article23. Powell RE, Zaccardi F, Beebe C, Chen XM, Crawford A, Cuddeback J, et al. Strategies for overcoming therapeutic inertia in type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab. 2021; 23:2137–54.
Article24. Mata-Cases M, Franch-Nadal J, Gratacos M, Mauricio D. Therapeutic inertia: still a long way to go that cannot be postponed. Diabetes Spectr. 2020; 33:50–7.
Article25. Khunti S, Khunti K, Seidu S. Therapeutic inertia in type 2 diabetes: prevalence, causes, consequences and methods to overcome inertia. Ther Adv Endocrinol Metab. 2019; 10:204–2018819844694.
Article26. Khunti K, Davies MJ. Clinical inertia: time to reappraise the terminology? Prim Care Diabetes. 2017; 11:105–6.27. Safford MM, Shewchuk R, Qu H, Williams JH, Estrada CA, Ovalle F, et al. Reasons for not intensifying medications: differentiating “clinical inertia” from appropriate care. J Gen Intern Med. 2007; 22:1648–55.
Article28. Laiteerapong N, Ham SA, Gao Y, Moffet HH, Liu JY, Huang ES, et al. The legacy effect in type 2 diabetes: impact of early glycemic control on future complications (The Diabetes & Aging Study). Diabetes Care. 2019; 42:416–26.
Article29. Control Group, Turnbull FM, Abraira C, Anderson RJ, Byington RP, Chalmers JP, et al. Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia. 2009; 52:2288–98.
Article30. Ali SN, Dang-Tan T, Valentine WJ, Hansen BB. Evaluation of the clinical and economic burden of poor glycemic control associated with therapeutic inertia in patients with type 2 diabetes in the United States. Adv Ther. 2020; 37:869–82.
Article31. Karam SL, Dendy J, Polu S, Blonde L. Overview of therapeutic inertia in diabetes: prevalence, causes, and consequences. Diabetes Spectr. 2020; 33:8–15.
Article32. Seidu S, Kunutsor SK, Topsever P, Hambling CE, Cos FX, Khunti K. Deintensification in older patients with type 2 diabetes: a systematic review of approaches, rates and outcomes. Diabetes Obes Metab. 2019; 21:1668–79.
Article33. Shivashankar R, Kirk K, Kim WC, Rouse C, Tandon N, Narayan KM, et al. Quality of diabetes care in low- and middle-income Asian and Middle Eastern countries (1993-2012): 20-year systematic review. Diabetes Res Clin Pract. 2015; 107:203–23.34. Evans M, Engberg S, Faurby M, Fernandes JD, Hudson P, Polonsky W. Adherence to and persistence with antidiabetic medications and associations with clinical and economic outcomes in people with type 2 diabetes mellitus: a systematic literature review. Diabetes Obes Metab. 2022; 24:377–90.
Article35. Henriksen K, Battles JB, Marks ES, Lewin DI. Advances in patient safety: from research to implementation (Volume 2: concepts and methodology). Rockville: Agency for Healthcare Research and Quality (US);2005. Chapter, Clinical inertia and outpatient medical errors. [cited 2023 Feb 10]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK20513.36. Wrzal PK, Bunko A, Myageri V, Kukaswadia A, Neish CS, Ivers NM. Strategies to overcome therapeutic inertia in type 2 diabetes mellitus: a scoping review. Can J Diabetes. 2021; 45:273–81.
Article37. Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T, et al. A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol. 2012; 73:691–705.
Article38. Vermeire E, Wens J, Van Royen P, Biot Y, Hearnshaw H, Lindenmeyer A. Interventions for improving adherence to treatment recommendations in people with type 2 diabetes mellitus. Cochrane Database Syst Rev. 2005; 2005:CD003638.
Article39. Low LL, Tong SF, Low WY. Selection of treatment strategies among patients with type 2 diabetes mellitus in Malaysia: a grounded theory approach. PLoS One. 2016; 11:e0147127.
Article40. Kanumilli N, Brunton S, Cos X, Deed G, Kushner P, Lin P, et al. Global survey investigating causes of treatment inertia in type 2 diabetes cardiorenal risk management. J Diabetes Complications. 2021; 35:107813.
Article41. Chew BH, Hussain H, Supian ZA. Is therapeutic inertia present in hyperglycaemia, hypertension and hypercholesterolaemia management among adults with type 2 diabetes in three health clinics in Malaysia?: a retrospective cohort study. BMC Fam Pract. 2021; 22:111.
Article42. Ong SE, Koh JJ, Toh SE, Chia KS, Balabanova D, McKee M, et al. Assessing the influence of health systems on type 2 diabetes mellitus awareness, treatment, adherence, and control: a systematic review. PLoS One. 2018; 13:e0195086.
Article43. Rosenbaum L. Peers, professionalism, and improvement: reframing the quality question. N Engl J Med. 2022; 386:1850–4.
Article44. Egede LE, Walker RJ, Linde S, Campbell JA, Dawson AZ, Williams JS, et al. Nonmedical interventions for type 2 diabetes: evidence, actionable strategies, and policy opportunities. Health Aff (Millwood). 2022; 41:963–70.
Article45. Fitzpatrick C, Gillies C, Seidu S, Kar D, Ioannidou E, Davies MJ, et al. Effect of pragmatic versus explanatory interventions on medication adherence in people with cardiometabolic conditions: a systematic review and meta-analysis. BMJ Open. 2020; 10:e036575.
Article46. Wei X, Barnsley J, Zakus D, Cockerill R, Glazier R, Sun X. Evaluation of a diabetes management program in China demonstrated association of improved continuity of care with clinical outcomes. J Clin Epidemiol. 2008; 61:932–9.
Article47. Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018; 7:CD001271.
Article48. Hughes JD, Wibowo Y, Sunderland B, Hoti K. The role of the pharmacist in the management of type 2 diabetes: current insights and future directions. Integr Pharm Res Pract. 2017; 6:15–27.
Article49. Bosch M, Dijkstra R, Wensing M, van der Weijden T, Grol R. Organizational culture, team climate and diabetes care in small office-based practices. BMC Health Serv Res. 2008; 8:180.
Article50. Benzer JK, Mohr DC, Evans L, Young G, Meterko MM, Moore SC, et al. Team process variation across diabetes quality of care trajectories. Med Care Res Rev. 2016; 73:565–89.
Article51. Warde CM, Linzer M, Schorling JB, Moore EM, Poplau S. Balancing unbalanced lives: a practical framework for personal and organizational change. Mayo Clin Proc Innov Qual Outcomes. 2019; 3:97–100.52. Hermans MP, Elisaf M, Michel G, Muls E, Nobels F, Vandenberghe H, et al. Benchmarking is associated with improved quality of care in type 2 diabetes: the OPTIMISE randomized, controlled trial. Diabetes Care. 2013; 36:3388–95.53. Cho MK, Kim MY. Self-management nursing intervention for controlling glucose among diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021; 18:12750.
Article54. Katon W, Russo J, Lin EH, Heckbert SR, Karter AJ, Williams LH, et al. Diabetes and poor disease control: is comorbid depression associated with poor medication adherence or lack of treatment intensification? Psychosom Med. 2009; 71:965–72.
Article55. Nieuwlaat R, Wilczynski N, Navarro T, Hobson N, Jeffery R, Keepanasseril A, et al. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2014; 2014:CD000011.
Article56. Bingham JM, Black M, Anderson EJ, Li Y, Toselli N, Fox S, et al. Impact of telehealth interventions on medication adherence for patients with type 2 diabetes, hypertension, and/or dyslipidemia: a systematic review. Ann Pharmacother. 2021; 55:637–49.
Article57. Robson N, Hosseinzadeh H. Impact of telehealth care among adults living with type 2 diabetes in primary care: a systematic review and meta-analysis of randomised controlled trials. Int J Environ Res Public Health. 2021; 18:12171.
Article58. Camara S, Bouenizabila E, Hermans MP, Ahn SA, Rousseau MF. Novel determinants preventing achievement of major cardiovascular targets in type 2 diabetes. Diabetes Metab Syndr. 2014; 8:145–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Anterior Lateral Thigh Free Flap and Achilles Tendon Reconstruction Surgery for Contact Dermal Burn of Heel Including Achilles Tendon: A Case Report -Surgical Treatment for Functional Recovery-
- Analyses of Timing of Single Heel Raise and Muscle Power after Achilles Tendon Repair
- Rupture of Achilles Tendon after Steroid Injection in Achilles Tendinitis (A Report of Five Cases)
- Parastomal Hernia-the Achilles Heel of a Permanent Colostomy
- Correlation between a Rupture of the Hypovascular Zone and Early Single Heel Raising after Achilles Tendon Repair