Guideline for the Surgical Management of Locally Invasive Differentiated Thyroid Cancer From the Korean Society of Head and Neck Surgery
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Otolaryngology-Head and Neck Surgery, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Otolaryngology-Head and Neck Surgery, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Otolaryngology-Head and Neck Surgery, Hanyang University College of Medicine, Seoul, Korea
- 5Department of Otolaryngology-Head and Neck Surgery, Korea University College of Medicine, Seoul, Korea
- 6Department of Otolaryngology-Head and Neck Surgery, Kosin University College of Medicine, Busan, Korea
- 7Department of Otolaryngology-Head and Neck Surgery, Dong-A University College of Medicine, Busan, Korea
- 8Department of Otolaryngology-Head and Neck Surgery, Soonchunhyang University College of Medicine, Asan, Korea
- 9Department of Otolaryngology-Head and Neck Surgery, Dongguk University College of Medicine, Goyang, Korea
- 10Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Inje University, Busan, Korea
- 11Department of Otolaryngology-Head and Neck Surgery, School of Medicine, Kyungpook National University, Daegu, Korea
- 12Department of Otolaryngology-Head and Neck Surgery, CHA University School of Medicine, Seongnam, Korea
- 13Department of Otolaryngology-Head and Neck Surgery, National Cancer Center, Goyang, Korea
- 14Department of Otolaryngology-Head and Neck Surgery, Ajou University School of Medicine, Suwon, Korea
- 15Department of Otolaryngology-Head and Neck Surgery, Hallym University College of Medicine, Chuncheon, Korea
- 16Department of Otolaryngology-Head and Neck Surgery, Chung-Ang University College of Medicine, Seoul, Korea
- 17Department of Otolaryngology-Head and Neck Surgery, Chonnam National University Medical School, Kwangju, Korea
- 18Department of Otolaryngology-Head and Neck Surgery, Konyang University College of Medicine, Daejeon, Korea
- 19Department of Otolaryngology-Head and Neck Surgery, Jeonbuk National University Medical School, Jeonju, Korea
- 20Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Kyung Hee University, Seoul, Korea
- 21Department of Otolaryngology-Head and Neck Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- 22Department of Otolaryngology-Head and Neck Surgery, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2539764
- DOI: http://doi.org/10.21053/ceo.2022.01732
Abstract
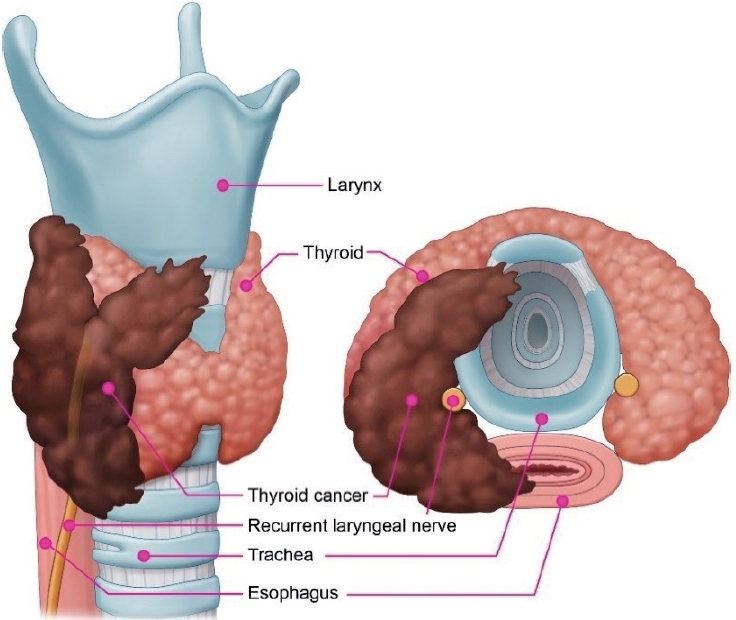
- The aim of this study was to develop evidence-based recommendations for determining the surgical extent in patients with locally invasive differentiated thyroid cancer (DTC). Locally invasive DTC with gross extrathyroidal extension invading surrounding anatomical structures may lead to several functional deficits and poor oncological outcomes. At present, the optimal extent of surgery in locally invasive DTC remains a matter of debate, and there are no adequate guidelines. On October 8, 2021, four experts searched the PubMed, Embase, and Cochrane Library databases; the identified papers were reviewed by 39 experts in thyroid and head and neck surgery. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach was used to assess the quality of evidence, and to develop and report recommendations. The strength of a recommendation reflects the confidence of a guideline panel that the desirable effects of an intervention outweigh any undesirable effects, across all patients for whom the recommendation is applicable. After completing the draft guidelines, Delphi questionnaires were completed by members of the Korean Society of Head and Neck Surgery. Twenty-seven evidence-based recommendations were made for several factors, including the preoperative workup; surgical extent of thyroidectomy; surgery for cancer invading the strap muscles, recurrent laryngeal nerve, laryngeal framework, trachea, or esophagus; and surgery for patients with central and lateral cervical lymph node involvement. Evidence-based guidelines were devised to help clinicians make safer and more efficient clinical decisions for the optimal surgical treatment of patients with locally invasive DTC.
Figure
Cited by 3 articles
-
Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Overview and Summary 2024
Young Joo Park, Eun Kyung Lee, Young Shin Song, Bon Seok Koo, Hyungju Kwon, Keunyoung Kim, Mijin Kim, Bo Hyun Kim, Won Gu Kim, Won Bae Kim, Won Woong Kim, Jung-Han Kim, Hee Kyung Kim, Hee Young Na, Shin Je Moon, Jung-Eun Moon, Sohyun Park, Jun-Ook Park, Ji-In Bang, Kyorim Back, Youngduk Seo, Dong Yeob Shin, Su-Jin Shin, Hwa Young Ahn, So Won Oh, Seung Hoon Woo, Ho-Ryun Won, Chang Hwan Ryu, Jee Hee Yoon, Ka Hee Yi, Min Kyoung Lee, Sang-Woo Lee, Seung Eun Lee, Sihoon Lee, Young Ah Lee, Joon-Hyop Lee, Ji Ye Lee, Jieun Lee, Cho Rok Lee, Dong-Jun Lim, Jae-Yol Lim, Yun Kyung Jeon, Kyong Yeun Jung, Ari Chong, Yun Jae Chung, Chan Kwon Jung, Kwanhoon Jo, Yoon Young Cho, A Ram Hong, Chae Moon Hong, Ho-Cheol Kang, Sun Wook Kim, Woong Youn Chung, Do Joon Park, Dong Gyu Na
Int J Thyroidol. 2024;17(1):1-20. doi: 10.11106/ijt.2024.17.1.1.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 2. Surgical Management of Thyroid Cancer 2024
Yoon Young Cho, Cho Rok Lee, Ho-Cheol Kang, Bon Seok Koo, Hyungju Kwon, Sun Wook Kim, Won Woong Kim, Jung-Han Kim, Dong Gyu Na, Young Joo Park, Kyorim Back, Young Shin Song, Seung Hoon Woo, Ho-Ryun Won, Chang Hwan Ryu, Jee Hee Yoon, Min Kyoung Lee, Eun Kyung Lee, Joon-Hyop Lee, Ji Ye Lee, Dong-Jun Lim, Jae-Yol Lim, Yun Jae Chung, Chan Kwon Jung, Jun-Ook Park, Hee Kyung Kim
Int J Thyroidol. 2024;17(1):30-52. doi: 10.11106/ijt.2024.17.1.30.Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 5. Evaluation of Recurrence Risk Postoperatively and Initial Risk Stratification in Differentiated Thyroid Cancer 2024
Eun Kyung Lee, Young Shin Song, Ho-Cheol Kang, Sun Wook Kim, Dong Gyu Na, Shin Je Moon, Dong-Jun Lim, Kyong Yeun Jung, Yun Jae Chung, Chan Kwon Jung, Young Joo Park
Int J Thyroidol. 2024;17(1):68-96. doi: 10.11106/ijt.2024.17.1.68.
Reference
-
1. Brauckhoff M. Classification of aerodigestive tract invasion from thyroid cancer. Langenbecks Arch Surg. 2014; Feb. 399(2):209–16.
Article2. McCaffrey TV, Bergstralh EJ, Hay ID. Locally invasive papillary thyroid carcinoma: 1940-1990. Head Neck. 1994; Mar-Apr. 16(2):165–72.
Article3. Nixon IJ, Simo R, Newbold K, Rinaldo A, Suarez C, Kowalski LP, et al. Management of invasive differentiated thyroid cancer. Thyroid. 2016; Sep. 26(9):1156–66.
Article4. Amin MB, Edge SB, Greene FL, Byrd DR, Brookland RK, Washington MK, et al. AJCC cancer staging manual. Springer;2017.5. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986; Dec. 61(12):978–96.
Article6. Shah JP, Loree TR, Dharker D, Strong EW, Begg C, Vlamis V. Prognostic factors in differentiated carcinoma of the thyroid gland. Am J Surg. 1992; Dec. 164(6):658–61.
Article7. Shaha AR, Shah JP, Loree TR. Patterns of failure in differentiated carcinoma of the thyroid based on risk groups. Head Neck. 1998; Jan. 20(1):26–30.
Article8. Djalilian M, Beahrs OH, Devine KD, Weiland LH, DeSanto LW. Intraluminal involvement of the larynx and trachea by thyroid cancer. Am J Surg. 1974; Oct. 128(4):500–4.
Article9. Cody HS, Shah JP. Locally invasive, well-differentiated thyroid cancer: 22 years’ experience at Memorial Sloan-Kettering Cancer Center. Am J Surg. 1981; Oct. 142(4):480–3.10. Batsakis JG. Laryngeal involvement by thyroid disease. Ann Otol Rhinol Laryngol. 1987; Nov-Dec. 96(6):718–9.11. Andersen PE, Kinsella J, Loree TR, Shaha AR, Shah JP. Differentiated carcinoma of the thyroid with extrathyroidal extension. Am J Surg. 1995; Nov. 170(5):467–70.
Article12. Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg. 2002; Aug. 26(8):879–85.
Article13. Segal K, Shpitzer T, Hazan A, Bachar G, Marshak G, Popovtzer A. Invasive well-differentiated thyroid carcinoma: effect of treatment modalities on outcome. Otolaryngol Head Neck Surg. 2006; May. 134(5):819–22.
Article14. Hotomi M, Sugitani I, Toda K, Kawabata K, Fujimoto Y. A novel definition of extrathyroidal invasion for patients with papillary thyroid carcinoma for predicting prognosis. World J Surg. 2012; Jun. 36(6):1231–40.
Article15. Lang BH, Lo CY, Wong KP, Wan KY. Should an involved but functioning recurrent laryngeal nerve be shaved or resected in a locally advanced papillary thyroid carcinoma. Ann Surg Oncol. 2013; Sep. 20(9):2951–7.
Article16. Kebebew E, Clark OH. Differentiated thyroid cancer: “complete” rational approach. World J Surg. 2000; Aug. 24(8):942–51.
Article17. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; Jan. 26(1):1–133.
Article18. Perros P, Boelaert K, Colley S, Evans C, Evans RM, Gerrard Ba G, et al. Guidelines for the management of thyroid cancer. Clin Endocrinol (Oxf). 2014; Jul. 81 Suppl 1:1–122.19. Yi KH, Lee EK, Kang HC, Kim SW, Kim IJ, Park SY, et al. 2016 Revised Korean Thyroid Association management guidelines for patients with thyroid nodules and thyroid cancer. Int J Thyroidol. 2016; Nov. 9(2):59–126.
Article20. Patel KN, Yip L, Lubitz CC, Grubbs EG, Miller BS, Shen W, et al. The American Association of Endocrine Surgeons Guidelines for the definitive surgical management of thyroid disease in adults. Ann Surg. 2020; Mar. 271(3):e21–93.
Article21. Kim SY, Park JE, Lee YJ, Seo HJ, Sheen SS, Hahn S, et al. Testing a tool for assessing the risk of bias for nonrandomized studies showed moderate reliability and promising validity. J Clin Epidemiol. 2013; Apr. 66(4):408–14.
Article22. Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Med Res Methodol. 2007; Feb. 7:10.
Article23. Russell MD, Kamani D, Randolph GW. Modern surgery for advanced thyroid cancer: a tailored approach. Gland Surg. 2020; Feb. 9(Suppl 2):S105–19.
Article24. Maher DI, Goare S, Forrest E, Grodski S, Serpell JW, Lee JC. Routine preoperative laryngoscopy for thyroid surgery is not necessary without risk factors. Thyroid. 2019; Nov. 29(11):1646–52.
Article25. Randolph GW, Kamani D. The importance of preoperative laryngoscopy in patients undergoing thyroidectomy: voice, vocal cord function, and the preoperative detection of invasive thyroid malignancy. Surgery. 2006; Mar. 139(3):357–62.26. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on Cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (eighth edition): what changed and why. Thyroid. 2017; Jun. 27(6):751–6.27. Shimamoto K, Satake H, Sawaki A, Ishigaki T, Funahashi H, Imai T. Preoperative staging of thyroid papillary carcinoma with ultrasonography. Eur J Radiol. 1998; Nov. 29(1):4–10.
Article28. Shin JH, Baek JH, Chung J, Ha EJ, Kim JH, Lee YH, et al. Ultrasonography diagnosis and imaging-based management of thyroid nodules: revised Korean Society of Thyroid Radiology consensus statement and recommendations. Korean J Radiol. 2016; May-Jun. 17(3):370–95.
Article29. Lee YC, Jung AR, Sohn YM, Kim EJ, Eun YG. Ultrasonographic features associated with false-negative and false-positive results of extrathyroidal extensions in papillary thyroid microcarcinoma. Eur Arch Otorhinolaryngol. 2018; Nov. 275(11):2817–22.
Article30. Moon SJ, Kim DW, Kim SJ, Ha TK, Park HK, Jung SJ. Ultrasound assessment of degrees of extrathyroidal extension in papillary thyroid microcarcinoma. Endocr Pract. 2014; Oct. 20(10):1037–43.31. King AD, Ahuja AT, To EW, Tse GM, Metreweli C. Staging papillary carcinoma of the thyroid: magnetic resonance imaging vs ultrasound of the neck. Clin Radiol. 2000; Mar. 55(3):222–6.32. Tomoda C, Uruno T, Takamura Y, Ito Y, Miya A, Kobayashi K, et al. Ultrasonography as a method of screening for tracheal invasion by papillary thyroid cancer. Surg Today. 2005; 35(10):819–22.
Article33. Seo YL, Yoon DY, Lim KJ, Cha JH, Yun EJ, Choi CS, et al. Locally advanced thyroid cancer: can CT help in prediction of extrathyroidal invasion to adjacent structures. AJR Am J Roentgenol. 2010; Sep. 195(3):W240–4.34. Takashima S, Takayama F, Wang Q, Kawakami S, Saito A, Kobayashi S, et al. Differentiated thyroid carcinomas: prediction of tumor invasion with MR imaging. Acta Radiol. 2000; Jul. 41(4):377–83.
Article35. Clark OH. Thyroid nodules and thyroid cancer: surgical aspects. West J Med. 1980; Jul. 133(1):1–8.36. Takashima S, Takayama F, Wang J, Kobayashi S, Kadoya M. Using MR imaging to predict invasion of the recurrent laryngeal nerve by thyroid carcinoma. AJR Am J Roentgenol. 2003; Mar. 180(3):837–42.37. Tovi F, Goldstein J. Locally aggressive differentiated thyroid carcinoma. J Surg Oncol. 1985; Jun. 29(2):99–104.38. Czaja JM, McCaffrey TV. The surgical management of laryngotracheal invasion by well-differentiated papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 1997; May. 123(5):484–90.39. Watanabe A, Saka H, Sakai S, Hirao T, Hattori T, Shimokata K. Bronchoscopic and cytopathological findings of tracheobronchial involvement in esophageal carcinoma. Endoscopy. 1990; Nov. 22(6):273–5.
Article40. Choi TK, Siu KF, Lam KH, Wong J. Bronchoscopy and carcinoma of the esophagus I: findings of bronchoscopy in carcinoma of the esophagus. Am J Surg. 1984; Jun. 147(6):757–9.41. Choi TK, Siu KF, Lam KH, Wong J. Bronchoscopy and carcinoma of the esophagus II: carcinoma of the esophagus with tracheobronchial involvement. Am J Surg. 1984; Jun. 147(6):760–2.42. Koike E, Yamashita H, Noguchi S, Ohshima A, Yamashita H, Watanabe S, et al. Endoscopic ultrasonography in patients with thyroid cancer: its usefulness and limitations for evaluating esophagopharyngeal invasion. Endoscopy. 2002; Jun. 34(6):457–60.
Article43. Koike E, Yamashita H, Noguchi S, Yamashita H, Ohshima A, Watanabe S, et al. Bronchoscopic diagnosis of thyroid cancer with laryngotracheal invasion. Arch Surg. 2001; Oct. 136(10):1185–9.
Article44. Lee YJ, Kim DW, Park HK, Kim DH, Jung SJ, Oh M, et al. Pre-operative ultrasound diagnosis of nodal metastasis in papillary thyroid carcinoma patients according to nodal compartment. Ultrasound Med Biol. 2015; May. 41(5):1294–300.
Article45. Hwang HS, Orloff LA. Efficacy of preoperative neck ultrasound in the detection of cervical lymph node metastasis from thyroid cancer. Laryngoscope. 2011; Mar. 121(3):487–91.
Article46. Choi JS, Chung WY, Kwak JY, Moon HJ, Kim MJ, Kim EK. Staging of papillary thyroid carcinoma with ultrasonography: performance in a large series. Ann Surg Oncol. 2011; Dec. 18(13):3572–8.
Article47. Zhao H, Li H. Meta-analysis of ultrasound for cervical lymph nodes in papillary thyroid cancer: diagnosis of central and lateral compartment nodal metastases. Eur J Radiol. 2019; Mar. 112:14–21.48. Kuna SK, Bracic I, Tesic V, Kuna K, Herceg GH, Dodig D. Ultrasonographic differentiation of benign from malignant neck lymphadenopathy in thyroid cancer. J Ultrasound Med. 2006; Dec. 25(12):1531–7.49. Al-Hilli Z, Strajina V, McKenzie TJ, Thompson GB, Farley DR, Regina Castro M, et al. Thyroglobulin measurement in fine-needle aspiration improves the diagnosis of cervical lymph node metastases in papillary thyroid carcinoma. Ann Surg Oncol. 2017; Mar. 24(3):739–44.
Article50. Konca Degertekin C, Yalcin MM, Cerit T, Ozkan C, Kalan I, Iyidir OT, et al. Lymph node fine-needle aspiration washout thyroglobulin in papillary thyroid cancer: diagnostic value and the effect of thyroglobulin antibodies. Endocr Res. 2016; Nov. 41(4):281–9.51. Grani G, Fumarola A. Thyroglobulin in lymph node fine-needle aspiration washout: a systematic review and meta-analysis of diagnostic accuracy. J Clin Endocrinol Metab. 2014; Jun. 99(6):1970–82.52. Xu Y, Wu D, Wu W, Jiang J, Xi C, Ye N, et al. Diagnostic value of cytology, thyroglobulin, and combination of them in fine-needle aspiration of metastatic lymph nodes in patients with differentiated thyroid cancer: a systematic review and network meta-analysis. Medicine (Baltimore). 2019; Nov. 98(45):e17859.53. Zhang X, Howell JM, Huang Y. Cervical lymph node fine-needle aspiration and needle-wash thyroglobulin reflex test for papillary thyroid carcinoma. Endocr Pathol. 2018; Dec. 29(4):346–50.
Article54. Cignarelli M, Ambrosi A, Marino A, Lamacchia O, Campo M, Picca G, et al. Diagnostic utility of thyroglobulin detection in fine-needle aspiration of cervical cystic metastatic lymph nodes from papillary thyroid cancer with negative cytology. Thyroid. 2003; Dec. 13(12):1163–7.
Article55. Suh CH, Baek JH, Choi YJ, Lee JH. Performance of CT in the preoperative diagnosis of cervical lymph node metastasis in patients with papillary thyroid cancer: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2017; Jan. 38(1):154–61.
Article56. Lee Y, Kim JH, Baek JH, Jung SL, Park SW, Kim J, et al. Value of CT added to ultrasonography for the diagnosis of lymph node metastasis in patients with thyroid cancer. Head Neck. 2018; Oct. 40(10):2137–48.
Article57. Choi YJ, Yun JS, Kook SH, Jung EC, Park YL. Clinical and imaging assessment of cervical lymph node metastasis in papillary thyroid carcinomas. World J Surg. 2010; Jul. 34(7):1494–9.58. Kim BS, Ryu HS, Kang KH. The value of preoperative PET-CT in papillary thyroid cancer. J Int Med Res. 2013; Apr. 41(2):445–56.
Article59. Kim K, Shim SR, Lee SW, Kim SJ. Diagnostic values of F-18 FDG PET or PET/CT, CT, and US for preoperative lymph node staging in thyroid cancer: a network meta-analysis. Br J Radiol. 2021; Apr. 94(1120):20201076.
Article60. Rajjoub SR, Yan H, Calcatera NA, Kuchta K, Wang CE, Lutfi W, et al. Thyroid lobectomy is not sufficient for T2 papillary thyroid cancers. Surgery. 2018; May. 163(5):1134–43.
Article61. Barney BM, Hitchcock YJ, Sharma P, Shrieve DC, Tward JD. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck. 2011; May. 33(5):645–9.
Article62. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS, et al. Extent of surgery affects survival for papillary thyroid cancer. Ann Surg. 2007; Sep. 246(3):375–84.
Article63. Xiang J, Wang Z, Sun W, Zhang H. The new T3b category has clinical significance? SEER-based study. Clin Endocrinol (Oxf). 2021; Mar. 94(3):449–59.
Article64. Song E, Lee YM, Oh HS, Jeon MJ, Song DE, Kim TY, et al. A relook at the T stage of differentiated thyroid carcinoma with a focus on gross extrathyroidal extension. Thyroid. 2019; Feb. 29(2):202–8.
Article65. Park SY, Kim HI, Kim JH, Kim JS, Oh YL, Kim SW, et al. Prognostic significance of gross extrathyroidal extension invading only strap muscles in differentiated thyroid carcinoma. Br J Surg. 2018; Aug. 105(9):1155–62.
Article66. Bortz MD, Kuchta K, Winchester DJ, Prinz RA, Moo-Young TA. Extrathyroidal extension predicts negative clinical outcomes in papillary thyroid cancer. Surgery. 2021; Jan. 169(1):2–6.
Article67. Li G, Li R, Song L, Chen W, Jiang K, Tang H, et al. Implications of extrathyroidal extension invading only the strap muscles in papillary thyroid carcinomas. Thyroid. 2020; Jan. 30(1):57–64.
Article68. Amit M, Boonsripitayanon M, Goepfert RP, Tam S, Busaidy NL, Cabanillas ME, et al. Extrathyroidal extension: does strap muscle invasion alone influence recurrence and survival in patients with differentiated thyroid cancer. Ann Surg Oncol. 2018; Oct. 25(11):3380–8.
Article69. Kim JW, Roh JL, Gong G, Cho KJ, Choi SH, Nam SY, et al. Extent of extrathyroidal extension as a significant predictor of nodal metastasis and extranodal extension in patients with papillary thyroid carcinoma. Ann Surg Oncol. 2017; Feb. 24(2):460–8.
Article70. Hassan A, Khalid M, Riaz S, Nawaz MK, Bashir H. Follicular thyroid carcinoma: disease response evaluation using American Thyroid Association risk assessment guidelines. Eur Thyroid J. 2015; Dec. 4(4):260–5.
Article71. Choi JS, Kim J, Kwak JY, Kim MJ, Chang HS, Kim EK. Preoperative staging of papillary thyroid carcinoma: comparison of ultrasound imaging and CT. AJR Am J Roentgenol. 2009; Sep. 193(3):871–8.
Article72. Kim H, Kim JA, Son EJ, Youk JH, Chung TS, Park CS, et al. Preoperative prediction of the extrathyroidal extension of papillary thyroid carcinoma with ultrasonography versus MRI: a retrospective cohort study. Int J Surg. 2014; 12(5):544–8.
Article73. Park YM, Wang SG, Goh JY, Shin DH, Kim IJ, Lee BJ. Intraoperative frozen section for the evaluation of extrathyroidal extension in papillary thyroid cancer. World J Surg. 2015; Jan. 39(1):187–93.
Article74. Henry LR, Solomon NP, Howard R, Gurevich-Uvena J, Horst LB, Coppit G, et al. The functional impact on voice of sternothyroid muscle division during thyroidectomy. Ann Surg Oncol. 2008; Jul. 15(7):2027–33.
Article75. Hirota K, Nishimoto K, Kumai Y, Miyamaru S, Miyamoto T, Saito H, et al. Swallowing dysfunction following surgery for well-differentiated thyroid cancer with extrathyroid invasion. Int J Clin Oncol. 2020; Nov. 25(11):1921–7.
Article76. Kihara M, Miyauchi A, Yabuta T, Higashiyama T, Fukushima M, Ito Y, et al. Outcome of vocal cord function after partial layer resection of the recurrent laryngeal nerve in patients with invasive papillary thyroid cancer. Surgery. 2014; Jan. 155(1):184–9.
Article77. Moritani S, Takenobu M, Yoshioka K, Kawamoto K, Fujii T, Yasunaga M, et al. Novel surgical methods for reconstruction of the recurrent laryngeal nerve: microscope-guided partial layer resection and intralaryngeal reconstruction of the recurrent laryngeal nerve. Surgery. 2021; May. 169(5):1124–30.
Article78. Nishida T, Nakao K, Hamaji M, Kamiike W, Kurozumi K, Matsuda H. Preservation of recurrent laryngeal nerve invaded by differentiated thyroid cancer. Ann Surg. 1997; Jul. 226(1):85–91.
Article79. Chen W, Lei J, You J, Lei Y, Li Z, Gong R, et al. Predictive factors and prognosis for recurrent laryngeal nerve invasion in papillary thyroid carcinoma. Onco Targets Ther. 2017; Sep. 10:4485–91.
Article80. Na HS, Kwon HK, Shin SC, Cheon YI, Seo M, Lee JC, et al. Clinical outcomes of T4a papillary thyroid cancer with recurrent laryngeal nerve involvement: a retrospective analysis. Sci Rep. 2021; Mar. 11(1):6707.
Article81. Ito Y, Kihara M, Takamura Y, Kobayashi K, Miya A, Miyauchi A. Prognosis and prognostic factors of patients with papillary thyroid carcinoma requiring resection of recurrent laryngeal nerve due to carcinoma extension. Endocr J. 2012; 59(3):247–52.
Article82. Kamani D, Darr EA, Randolph GW. Electrophysiologic monitoring characteristics of the recurrent laryngeal nerve preoperatively paralyzed or invaded with malignancy. Otolaryngol Head Neck Surg. 2013; Nov. 149(5):682–8.
Article83. Kim KH, Sung MW, Chang KH, Kang BS. Therapeutic dilemmas in the management of thyroid cancer with laryngotracheal involvement. Otolaryngol Head Neck Surg. 2000; May. 122(5):763–7.
Article84. Iwaki S, Maeda T, Saito M, Otsuki N, Takahashi M, Wakui E, et al. Role of immediate recurrent laryngeal nerve reconstruction in surgery for thyroid cancers with fixed vocal cords. Head Neck. 2017; Mar. 39(3):427–31.
Article85. Yumoto E, Sanuki T, Kumai Y. Immediate recurrent laryngeal nerve reconstruction and vocal outcome. Laryngoscope. 2006; Sep. 116(9):1657–61.
Article86. Yuan Q, Hou J, Liao Y, Zheng L, Wang K, Wu G. Selective vagus-recurrent laryngeal nerve anastomosis in thyroidectomy with cancer invasion or iatrogenic transection. Langenbecks Arch Surg. 2020; Jun. 405(4):461–8.
Article87. Shelton VK, Skolnik EM, Berlinger FG, Arab M. Laryngotracheal invasion by thyroid-carcinoma. Ann Otol Rhinol Laryngol. 1982; Jul-Aug. 91(4 Pt 1):363–9.88. McCarty TM, Kuhn JA, Williams WL, Ellenhorn JD, O’Brien JC, Preskitt JT, et al. Surgical management of thyroid cancer invading the airway. Ann Surg Oncol. 1997; Jul-Aug. 4(5):403–8.
Article89. Grillo HC, Zannini P. Resectional management of airway invasion by thyroid carcinoma. Ann Thorac Surg. 1986; Sep. 42(3):287–98.
Article90. Mattavelli F, Bombardieri E, Collini P, Costa L, Pizzi N, Fallahadar D, et al. Role of surgery in treatment of advanced differentiated thyroid carcinomas. Acta Otorhinolaryngol Ital. 2007; Apr. 27(2):62–7.91. Chala AI, Velez S, Sanabria A. The role of laryngectomy in locally advanced thyroid carcinoma: review of 16 cases. Acta Otorhinolaryngol Ital. 2018; Apr. 38(2):109–14.
Article92. Moritani S. Surgical management of laryngeal invasion by papillary thyroid carcinoma: a retrospective analysis. Thyroid. 2015; May. 25(5):528–33.
Article93. McCaffrey JC. Aerodigestive tract invasion by well-differentiated thyroid carcinoma: diagnosis, management, prognosis, and biology. Laryngoscope. 2006; Jan. 116(1):1–11.
Article94. Bayles SW, Kingdom TT, Carlson GW. Management of thyroid carcinoma invading the aerodigestive tract. Laryngoscope. 1998; Sep. 108(9):1402–7.
Article95. Wada N, Nakayama H, Masudo Y, Suganuma N, Rino Y. Clinical outcome of different modes of resection in papillary thyroid carcinomas with laryngotracheal invasion. Langenbecks Arch Surg. 2006; Nov. 391(6):545–9.
Article96. Gaissert HA, Honings J, Grillo HC, Donahue DM, Wain JC, Wright CD, et al. Segmental laryngotracheal and tracheal resection for invasive thyroid carcinoma. Ann Thorac Surg. 2007; Jun. 83(6):1952–9.
Article97. Abboud B, Abou Zeid H, Rohbane R, Jabbour H, Haddad A, Tabchy B. Surgical management and prognosis of thyroid carcinomas invading adjacent structures. Lebanese Med J. 2018; 66(1):28–34.
Article98. Shin DH, Mark EJ, Suen HC, Grillo HC. Pathologic staging of papillary carcinoma of the thyroid with airway invasion based on the anatomic manner of extension to the trachea: a clinicopathologic study based on 22 patients who underwent thyroidectomy and airway resection. Hum Pathol. 1993; Aug. 24(8):866–70.
Article99. Ji YB, Tae K, Lee YS, Jeong JH, Lee SH, Kim KR, et al. Surgical management of tracheal invasion by differentiated thyroid cancer: how we do it. Clin Otolaryngol. 2009; Dec. 34(6):565–7.
Article100. Park CS, Suh KW, Min JS. Cartilage-shaving procedure for the control of tracheal cartilage invasion by thyroid carcinoma. Head Neck. 1993; Jul-Aug. 15(4):289–91.
Article101. Friedman M, Danielzadeh JA, Caldarelli DD. Treatment of patients with carcinoma of the thyroid invading the airway. Arch Otolaryngol Head Neck Surg. 1994; Dec. 120(12):1377–81.
Article102. Ito Y, Fukushima M, Yabuta T, Tomoda C, Inoue H, Kihara M, et al. Local prognosis of patients with papillary thyroid carcinoma who were intra-operatively diagnosed as having minimal invasion of the trachea: a 17-year experience in a single institute. Asian J Surg. 2009; Apr. 32(2):102–8.
Article103. Su SY, Milas ZL, Bhatt N, Roberts D, Clayman GL. Well-differentiated thyroid cancer with aerodigestive tract invasion: long-term control and functional outcomes. Head Neck. 2016; Jan. 38(1):72–8.
Article104. Wang LY, Nixon IJ, Patel SG, Palmer FL, Tuttle RM, Shaha A, et al. Operative management of locally advanced, differentiated thyroid cancer. Surgery. 2016; Sep. 160(3):738–46.
Article105. Brauckhoff M, Machens A, Thanh PN, Lorenz K, Schmeil A, Stratmann M, et al. Impact of extent of resection for thyroid cancer invading the aerodigestive tract on surgical morbidity, local recurrence, and cancer-specific survival. Surgery. 2010; Dec. 148(6):1257–66.
Article106. Hay ID, McConahey WM, Goellner JR. Managing patients with papillary thyroid carcinoma: insights gained from the Mayo Clinic’s experience of treating 2,512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc. 2002; 113:241–60.107. Matsumoto F, Ikeda K. Surgical management of tracheal invasion by well-differentiated thyroid cancer. Cancers (Basel). 2021; Feb. 13(4):797.
Article108. Allen M, Spillinger A, Arianpour K, Johnson J, Johnson AP, Folbe AJ, et al. Tracheal resection in the management of thyroid cancer: an evidence-based approach. Laryngoscope. 2021; Apr. 131(4):932–46.109. Musholt TJ, Musholt PB, Behrend M, Raab R, Scheumann GF, Klempnauer J. Invasive differentiated thyroid carcinoma: tracheal resection and reconstruction procedures in the hands of the endocrine surgeon. Surgery. 1999; Dec. 126(6):1078–88.
Article110. Tsukahara K, Sugitani I, Kawabata K. Surgical management of tracheal shaving for papillary thyroid carcinoma with tracheal invasion. Acta Otolaryngol. 2009; Dec. 129(12):1498–502.
Article111. Shadmehr MB, Farzanegan R, Zangi M, Mohammadzadeh A, Sheikhy K, Pejhan S, et al. Thyroid cancers with laryngotracheal invasion. Eur J Cardiothorac Surg. 2012; Mar. 41(3):635–40.
Article112. Nishida T, Nakao K, Hamaji M. Differentiated thyroid carcinoma with airway invasion: indication for tracheal resection based on the extent of cancer invasion. J Thorac Cardiovasc Surg. 1997; Jul. 114(1):84–92.
Article113. Ozaki O, Sugino K, Mimura T, Ito K. Surgery for patients with thyroid carcinoma invading the trachea: circumferential sleeve resection followed by end-to-end anastomosis. Surgery. 1995; Mar. 117(3):268–71.
Article114. Chen W, Zou S, Wang L, Wu C, Wang Z, Li K, et al. Anastomosis in the absence of a suprahyoid release following circumferential sleeve resection is feasible in differentiated thyroid carcinoma patients with tracheal invasion. Oncol Lett. 2017; Sep. 14(3):2822–30.
Article115. Tsai YF, Tseng YL, Wu MH, Hung CJ, Lai WW, Lin MY. Aggressive resection of the airway invaded by thyroid carcinoma. Br J Surg. 2005; Nov. 92(11):1382–7.
Article116. Kim H, Jung HJ, Lee SY, Kwon TK, Kim KH, Sung MW, et al. Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur Arch Otorhinolaryngol. 2016; Jul. 273(7):1919–26.
Article117. Warshavsky A, Rosen R, Nard-Carmel N, Muhanna N, Ungar O, Abergel A, et al. Outcomes of tracheal resections in well-differentiated thyroid cancer-a case series and meta-analysis. World J Surg. 2021; Sep. 45(9):2752–8.
Article118. Moritani S. Window resection for intraluminal cricotracheal invasion by papillary thyroid carcinoma. World J Surg. 2017; Jul. 41(7):1812–9.
Article119. Ebihara M, Kishimoto S, Hayashi R, Miyazaki M, Shinozaki T, Daiko H, et al. Window resection of the trachea and secondary reconstruction for invasion by differentiated thyroid carcinoma. Auris Nasus Larynx. 2011; Apr. 38(2):271–5.
Article120. Ballantyne AJ. Resections of the upper aerodigestive tract for locally invasive thyroid cancer. Am J Surg. 1994; Dec. 168(6):636–9.
Article121. Liu J, Ren J, Lv D, Wang J, Deng D, Li L, et al. Simultaneous tracheal and esophageal reconstruction for thyroid cancer involving trachea and esophagus using a free bipaddled posterior tibial artery perforator flap. Head Neck. 2019; Sep. 41(9):3472–7.
Article122. Fujimoto Y, Obara T, Ito Y, Kodama T, Yashiro T, Yamashita T, et al. Aggressive surgical approach for locally invasive papillary carcinoma of the thyroid in patients over forty-five years of age. Surgery. 1986; Dec. 100(6):1098–107.123. Melliere DJ, Ben Yahia NE, Becquemin JP, Lange F, Boulahdour H. Thyroid carcinoma with tracheal or esophageal involvement: limited or maximal surgery. Surgery. 1993; Feb. 113(2):166–72.124. Tanaka K, Sonoo H, Yamamoto Y, Udagawa K, Arime I, Kunisue H, et al. Analyses of the outcome of locally invasive papillary thyroid carcinomas. Thyroid. 1999; Oct. 9(10):1017–22.
Article125. Martins AS, Melo GM, Valerio JB, Langner E, Lage HT, Tincani AJ. Treatment of locally aggressive well-differentiated thyroid cancer. Int Surg. 2001; Oct-Dec. 86(4):213–9.126. Hartl DM, Zago S, Leboulleux S, Mirghani H, Deandreis D, Baudin E, et al. Resection margins and prognosis in locally invasive thyroid cancer. Head Neck. 2014; Jul. 36(7):1034–8.
Article127. Ito Y, Miyauchi A, Masuoka H, Fukushima M, Kihara M, Miya A. Excellent prognosis of central lymph node recurrence-free survival for cN0M0 papillary thyroid carcinoma patients who underwent routine prophylactic central node dissection. World J Surg. 2018; Aug. 42(8):2462–8.
Article128. Xue S, Wang P, Liu J, Li R, Zhang L, Chen G. Prophylactic central lymph node dissection in cN0 patients with papillary thyroid carcinoma: a retrospective study in China. Asian J Surg. 2016; Jul. 39(3):131–6.
Article129. Giles Senyurek Y, Tunca F, Boztepe H, Alagol F, Terzioglu T, Tezelman S. The long term outcome of papillary thyroid carcinoma patients without primary central lymph node dissection: expected improvement of routine dissection. Surgery. 2009; Dec. 146(6):1188–95.
Article130. Barczynski M, Konturek A, Stopa M, Nowak W. Prophylactic central neck dissection for papillary thyroid cancer. Br J Surg. 2013; Feb. 100(3):410–8.
Article131. Filetti S, Durante C, Hartl D, Leboulleux S, Locati LD, Newbold K, et al. Thyroid cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2019; Dec. 30(12):1856–83.
Article132. Medas F, Canu GL, Cappellacci F, Anedda G, Conzo G, Erdas E, et al. Prophylactic central lymph node dissection improves diseasefree survival in patients with intermediate and high risk differentiated thyroid carcinoma: a retrospective analysis on 399 patients. Cancers (Basel). 2020; Jun. 12(6):1658.
Article133. Hartl DM, Leboulleux S, Al Ghuzlan A, Baudin E, Chami L, Schlumberger M, et al. Optimization of staging of the neck with prophylactic central and lateral neck dissection for papillary thyroid carcinoma. Ann Surg. 2012; Apr. 255(4):777–83.
Article134. Yoo HS, Shin MC, Ji YB, Song CM, Lee SH, Tae K. Optimal extent of prophylactic central neck dissection for papillary thyroid carcinoma: comparison of unilateral versus bilateral central neck dissection. Asian J Surg. 2018; Jul. 41(4):363–9.
Article135. Ywata de Carvalho A, Chulam TC, Kowalski LP. Long-term results of observation vs prophylactic selective level VI neck dissection for papillary thyroid carcinoma at a cancer center. JAMA Otolaryngol Head Neck Surg. 2015; Jul. 141(7):599–606.
Article136. Kim SK, Woo JW, Lee JH, Park I, Choe JH, Kim JH, et al. Prophylactic central neck dissection might not be necessary in papillary thyroid carcinoma: analysis of 11,569 cases from a single institution. J Am Coll Surg. 2016; May. 222(5):853–64.
Article137. Zetoune T, Keutgen X, Buitrago D, Aldailami H, Shao H, Mazumdar M, et al. Prophylactic central neck dissection and local recurrence in papillary thyroid cancer: a meta-analysis. Ann Surg Oncol. 2010; Dec. 17(12):3287–93.
Article138. Sippel RS, Robbins SE, Poehls JL, Pitt SC, Chen H, Leverson G, et al. A randomized controlled clinical trial: no clear benefit to prophylactic central neck dissection in patients with clinically node negative papillary thyroid cancer. Ann Surg. 2020; Sep. 272(3):496–503.139. Liu Q, Pang WT, Dong YB, Wang ZX, Yu MH, Huang XF, et al. Analysis of risk factors for lateral lymph node metastasis in papillary thyroid carcinoma: a retrospective cohort study. World J Otorhinolaryngol Head Neck Surg. 2022; Apr. 8(3):274–8.
Article140. Podnos YD, Smith D, Wagman LD, Ellenhorn JD. The implication of lymph node metastasis on survival in patients with well-differentiated thyroid cancer. Am Surg. 2005; Sep. 71(9):731–4.
Article141. Zaydfudim V, Feurer ID, Griffin MR, Phay JE. The impact of lymph node involvement on survival in patients with papillary and follicular thyroid carcinoma. Surgery. 2008; Dec. 144(6):1070–8.
Article142. Leenhardt L, Erdogan MF, Hegedus L, Mandel SJ, Paschk R, Rago T, et al. 2013 European thyroid association guidelines for cervical ultrasound scan and ultrasound-guided techniques in the postoperative management of patients with thyroid cancer. Eur Thyroid J. 2013; Sep. 2(3):147–59.
Article143. Adam MA, Pura J, Goffredo P, Dinan MA, Reed SD, Scheri RP, et al. Presence and number of lymph node metastases are associated with compromised survival for patients younger than age 45 years with papillary thyroid cancer. J Clin Oncol. 2015; Jul. 33(21):2370–5.
Article144. Kouvaraki MA, Shapiro SE, Fornage BD, Edeiken-Monro BS, Sherman SI, Vassilopoulou-Sellin R, et al. Role of preoperative ultrasonography in the surgical management of patients with thyroid cancer. Surgery. 2003; Dec. 134(6):946–55.
Article145. Alzahrani AS, Alsuhaibani H, Salam SA, Al Sifri SN, Mohamed G, Al Sobhi S, et al. Diagnostic accuracy of high-resolution neck ultrasonography in the follow-up of differentiated thyroid cancer: a prospective study. Endocr Pract. 2005; May-Jun. 11(3):165–71.
Article146. do Rosario PW, Fagundes TA, Maia FF, Franco AC, Figueiredo MB, Purisch S. Sonography in the diagnosis of cervical recurrence in patients with differentiated thyroid carcinoma. J Ultrasound Med. 2004; Jul. 23(7):915–20.
Article147. Leboulleux S, Girard E, Rose M, Travagli JP, Sabbah N, Caillou B, et al. Ultrasound criteria of malignancy for cervical lymph nodes in patients followed up for differentiated thyroid cancer. J Clin Endocrinol Metab. 2007; Sep. 92(9):3590–4.
Article148. Park JS, Son KR, Na DG, Kim E, Kim S. Performance of preoperative sonographic staging of papillary thyroid carcinoma based on the sixth edition of the AJCC/UICC TNM classification system. AJR Am J Roentgenol. 2009; Jan. 192(1):66–72.
Article149. Sohn YM, Kwak JY, Kim EK, Moon HJ, Kim SJ, Kim MJ. Diagnostic approach for evaluation of lymph node metastasis from thyroid cancer using ultrasound and fine-needle aspiration biopsy. AJR Am J Roentgenol. 2010; Jan. 194(1):38–43.
Article150. Lang BH, Wong KP, Wan KY, Lo CY. Impact of routine unilateral central neck dissection on preablative and postablative stimulated thyroglobulin levels after total thyroidectomy in papillary thyroid carcinoma. Ann Surg Oncol. 2012; Jan. 19(1):60–7.151. Wang TS, Evans DB, Fareau GG, Carroll T, Yen TW. Effect of prophylactic central compartment neck dissection on serum thyroglobulin and recommendations for adjuvant radioactive iodine in patients with differentiated thyroid cancer. Ann Surg Oncol. 2012; Dec. 19(13):4217–22.152. Musacchio MJ, Kim AW, Vijungco JD, Prinz RA. Greater local recurrence occurs with “berry picking” than neck dissection in thyroid cancer. Am Surg. 2003; Mar. 69(3):191–7.153. Noguchi M, Kumaki T, Taniya T, Segawa M, Nakano T, Ohta N, et al. Impact of neck dissection on survival in well-differentiated thyroid cancer: a multivariate analysis of 218 cases. Int Surg. 1990; Oct-Dec. 75(4):220–4.154. Keum HS, Ji YB, Kim JM, Jeong JH, Choi WH, Ahn YH, et al. Optimal surgical extent of lateral and central neck dissection for papillary thyroid carcinoma located in one lobe with clinical lateral lymph node metastasis. World J Surg Oncol. 2012; Oct. 10:221.
Article155. Kim SK, Woo JW, Lee JH, Park I, Choe JH, Kim JH, et al. Role of BRAF V600E mutation as an indicator of the extent of thyroidectomy and lymph node dissection in conventional papillary thyroid carcinoma. Surgery. 2015; Dec. 158(6):1500–11.
Article156. Bae SY, Yang JH, Choi MY, Choe JH, Kim JH, Kim JS. Right paraesophageal lymph node dissection in papillary thyroid carcinoma. Ann Surg Oncol. 2012; Mar. 19(3):996–1000.
Article157. Kouvaraki MA, Lee JE, Shapiro SE, Sherman SI, Evans DB. Preventable reoperations for persistent and recurrent papillary thyroid carcinoma. Surgery. 2004; Dec. 136(6):1183–91.
Article158. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Preoperative ultrasonographic examination for lymph node metastasis: usefulness when designing lymph node dissection for papillary microcarcinoma of the thyroid. World J Surg. 2004; May. 28(5):498–501.
Article159. Pingpank JF, Sasson AR, Hanlon AL, Friedman CD, Ridge JA. Tumor above the spinal accessory nerve in papillary thyroid cancer that involves lateral neck nodes: a common occurrence. Arch Otolaryngol Head Neck Surg. 2002; Nov. 128(11):1275–8.
Article160. Ahmadi N, Grewal A, Davidson BJ. Patterns of cervical lymph node metastases in primary and recurrent papillary thyroid cancer. J Oncol. 2011; 2011:735678.
Article161. Lombardi D, Paderno A, Giordano D, Barbieri D, Taboni S, Piazza C, et al. Therapeutic lateral neck dissection in well-differentiated thyroid cancer: analysis on factors predicting distribution of positive nodes and prognosis. Head Neck. 2018; Feb. 40(2):242–50.
Article162. Lee J, Sung TY, Nam KH, Chung WY, Soh EY, Park CS. Is level IIb lymph node dissection always necessary in N1b papillary thyroid carcinoma patients. World J Surg. 2008; May. 32(5):716–21.
Article163. Lee BJ, Wang SG, Lee JC, Son SM, Kim IJ, Kim YK. Level IIb lymph node metastasis in neck dissection for papillary thyroid carcinoma. Arch Otolaryngol Head Neck Surg. 2007; Oct. 133(10):1028–30.
Article164. Neiderman NN, Baris H, Duek I, Warshavsky A, Ringel B, Izkhakov E, et al. Lateral neck dissection for well-differentiated thyroid carcinoma: is prophylactic level V neck dissection necessary? A retrospective cohort study. Ear Nose Throat J. 2021; Apr. 29. [Epub]. https://doi.org/10.1177/01455613211003805.
Article165. Roh JL, Kim JM, Park CI. Lateral cervical lymph node metastases from papillary thyroid carcinoma: pattern of nodal metastases and optimal strategy for neck dissection. Ann Surg Oncol. 2008; Apr. 15(4):1177–82.
Article166. Yanir Y, Doweck I. Regional metastases in well-differentiated thyroid carcinoma: pattern of spread. Laryngoscope. 2008; Mar. 118(3):433–6.
Article167. Caron NR, Tan YY, Ogilvie JB, Triponez F, Reiff ES, Kebebew E, et al. Selective modified radical neck dissection for papillary thyroid cancer-is level I, II and V dissection always necessary. World J Surg. 2006; May. 30(5):833–40.
Article168. Harries V, McGill M, Wang LY, Tuttle RM, Wong RJ, Shaha AR, et al. Is a prophylactic central compartment neck dissection required in papillary thyroid carcinoma patients with clinically involved lateral compartment lymph nodes. Ann Surg Oncol. 2021; Jan. 28(1):512–8.
Article169. Khafif A, Ben-Yosef R, Abergel A, Kesler A, Landsberg R, Fliss DM. Elective paratracheal neck dissection for lateral metastases from papillary carcinoma of the thyroid: is it indicated. Head Neck. 2008; Mar. 30(3):306–10.
Article170. Scharpf J, Tuttle M, Wong R, Ridge D, Smith R, Hartl D, et al. Comprehensive management of recurrent thyroid cancer: an American Head and Neck Society consensus statement. Head Neck. 2016; Dec. 38(12):1862–9.
Article171. Urken ML, Milas M, Randolph GW, Tufano R, Bergman D, Bernet V, et al. Management of recurrent and persistent metastatic lymph nodes in well-differentiated thyroid cancer: a multifactorial decision-making guide for the thyroid cancer care collaborative. Head Neck. 2015; Apr. 37(4):605–14.
Article172. Chami L, Hartl D, Leboulleux S, Baudin E, Lumbroso J, Schlumberger M, et al. Preoperative localization of neck recurrences from thyroid cancer: charcoal tattooing under ultrasound guidance. Thyroid. 2015; Mar. 25(3):341–6.
Article173. Lang BH, Shek TW, Chan AO, Lo CY, Wan KY. Significance of size of persistent/recurrent central nodal disease on surgical morbidity and response to therapy in reoperative neck dissection for papillary thyroid carcinoma. Thyroid. 2017; Jan. 27(1):67–73.
Article174. Clayman GL, Agarwal G, Edeiken BS, Waguespack SG, Roberts DB, Sherman SI. Long-term outcome of comprehensive central compartment dissection in patients with recurrent/persistent papillary thyroid carcinoma. Thyroid. 2011; Dec. 21(12):1309–16.
Article175. Lamartina L, Borget I, Mirghani H, Al Ghuzlan A, Berdelou A, Bidault F, et al. Surgery for neck recurrence of differentiated thyroid cancer: outcomes and risk factors. J Clin Endocrinol Metab. 2017; Mar. 102(3):1020–31.176. Chinn SB, Zafereo ME, Waguespack SG, Edeiken BS, Roberts DB, Clayman GL. Long-term outcomes of lateral neck dissection in patients with recurrent or persistent well-differentiated thyroid cancer. Thyroid. 2017; Oct. 27(10):1291–9.
Article177. Wu G, Fraser S, Pai SI, Farrag TY, Ladenson PW, Tufano RP. Determining the extent of lateral neck dissection necessary to establish regional disease control and avoid reoperation after previous total thyroidectomy and radioactive iodine for papillary thyroid cancer. Head Neck. 2012; Oct. 34(10):1418–21.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Treatment in Locally Advanced Thyroid Cancer – Trachea, Larynx, Esophagus Invasion Management
- ATA Guideline in a View Point of Nuclear Medicine
- Surgery for Advanced Nodal Metastasis in Thyroid Cancer
- Diagnostic and Therapeutic Approaches to Radioactive Iodine Refractory Differentiated Thyroid Cancer
- A Case of Window Resection and Secondary Reconstruction of the Trachea Invaded by Papillary Thyroid Carcinoma