Endocrinol Metab.
2022 Dec;37(6):819-829. 10.3803/EnM.2022.1598.
Prenatal Exposure to Per- and Polyfluoroalkyl Substances, Maternal Thyroid Dysfunction, and Child Autism Spectrum Disorder
- Affiliations
-
- 1Department of Environmental Science, Baylor University, Waco, TX, USA
- 2Department of Public Health Sciences, University of California, Davis, CA, USA
- 3UC Davis MIND (Medical Investigations of Neurodevelopmental Disorders) Institute, Sacramento, CA, USA
- 4Section of Endocrinology, Diabetes, and Nutrition, Department of Medicine, Boston University School of Medicine, Boston, MA, USA
- KMID: 2537282
- DOI: http://doi.org/10.3803/EnM.2022.1598
Abstract
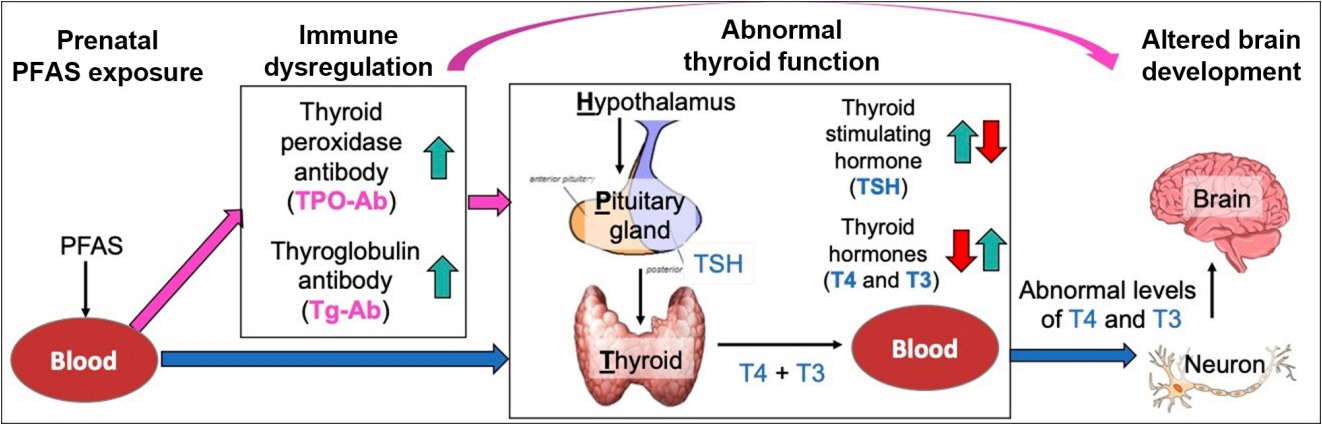
- Autism spectrum disorder (ASD), with its high economic and societal costs, is a growing public health concern whose prevalence has risen steadily over the last two decades. Although actual increased incidence versus improved diagnosis remains controversial, the increased prevalence of ASD suggests non-inherited factors as likely contributors. There is increasing epidemiologic evidence that abnormal maternal thyroid function during pregnancy is associated with increased risk of child ASD and other neurodevelopmental disorders. Prenatal exposure to endocrine-disrupting chemicals such as per- and polyfluoroalkyl substances (PFAS) is known to disrupt thyroid function and can affect early brain development; thus, thyroid dysfunction is hypothesized to mediate this relationship. The concept of a potential pathway from prenatal PFAS exposure through thyroid dysfunction to ASD etiology is not new; however, the extant literature on this topic is scant. The aim of this review is to evaluate and summarize reports with regard to potential mechanisms in this pathway.
Keyword
Figure
Reference
-
1. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Arlington: American Psychiatric Association;2013.2. Rogge N, Janssen J. The economic costs of autism spectrum disorder: a literature review. J Autism Dev Disord. 2019; 49:2873–900.3. Leigh JP, Du J. Brief report: forecasting the economic burden of autism in 2015 and 2025 in the United States. J Autism Dev Disord. 2015; 45:4135–9.4. Myers SM, Voigt RG, Colligan RC, Weaver AL, Storlie CB, Stoeckel RE, et al. Autism spectrum disorder: incidence and time trends over two decades in a populationbased birth cohort. J Autism Dev Disord. 2019; 49:1455–74.5. Maenner MJ, Shaw KA, Bakian AV, Bilder DA, Durkin MS, Esler A, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years: autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR Surveill Summ. 2021; 70:1–16.6. Grinker RR, Leventhal BL. Estimating the incidence of autism. Epidemiology. 2009; 20:622–3.7. Hertz-Picciotto I, Delwiche L. The rise in autism and the role of age at diagnosis. Epidemiology. 2009; 20:84–90.8. King M, Bearman P. Diagnostic change and the increased prevalence of autism. Int J Epidemiol. 2009; 38:1224–34.9. Hallmayer J, Cleveland S, Torres A, Phillips J, Cohen B, Torigoe T, et al. Genetic heritability and shared environmental factors among twin pairs with autism. Arch Gen Psychiatry. 2011; 68:1095–102.10. Sandin S, Lichtenstein P, Kuja-Halkola R, Larsson H, Hultman CM, Reichenberg A. The familial risk of autism. JAMA. 2014; 311:1770–7.11. Roberts EM, English PB, Grether JK, Windham GC, Somberg L, Wolff C. Maternal residence near agricultural pesticide applications and autism spectrum disorders among children in the California central valley. Environ Health Perspect. 2007; 115:1482–9.
Article12. Shelton JF, Geraghty EM, Tancredi DJ, Delwiche LD, Schmidt RJ, Ritz B, et al. Neurodevelopmental disorders and prenatal residential proximity to agricultural pesticides: the CHARGE study. Environ Health Perspect. 2014; 122:1103–9.
Article13. Volk HE, Hertz-Picciotto I, Delwiche L, Lurmann F, McConnell R. Residential proximity to freeways and autism in the CHARGE study. Environ Health Perspect. 2011; 119:873–7.
Article14. Volk HE, Lurmann F, Penfold B, Hertz-Picciotto I, McConnell R. Traffic-related air pollution, particulate matter, and autism. JAMA Psychiatry. 2013; 70:71–7.15. Brucato M, Ladd-Acosta C, Li M, Caruso D, Hong X, Kaczaniuk J, et al. Prenatal exposure to fever is associated with autism spectrum disorder in the Boston Birth Cohort. Autism Res. 2017; 10:1878–90.16. Croen LA, Qian Y, Ashwood P, Zerbo O, Schendel D, Pinto-Martin J, et al. Infection and fever in pregnancy and autism spectrum disorders: findings from the study to explore early development. Autism Res. 2019; 12:1551–61.17. Schmidt RJ. Maternal folic acid supplements associated with reduced autism risk in the child. Evid Based Med. 2013; 18:e53.
Article18. Schmidt RJ, Hansen RL, Hartiala J, Allayee H, Schmidt LC, Tancredi DJ, et al. Prenatal vitamins, one-carbon metabolism gene variants, and risk for autism. Epidemiology. 2011; 22:476–85.19. Schmidt RJ, Tancredi DJ, Ozonoff S, Hansen RL, Hartiala J, Allayee H, et al. Maternal periconceptional folic acid intake and risk of autism spectrum disorders and developmental delay in the CHARGE (CHildhood Autism Risks from Genetics and Environment) case-control study. Am J Clin Nutr. 2012; 96:80–9.20. Krakowiak P, Walker CK, Bremer AA, Baker AS, Ozonoff S, Hansen RL, et al. Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics. 2012; 129:e1121–8.21. Li M, Fallin MD, Riley A, Landa R, Walker SO, Silverstein M, et al. The association of maternal obesity and diabetes with autism and other developmental disabilities. Pediatrics. 2016; 137:e20152206.
Article22. Mann JR, McDermott S, Bao H, Hardin J, Gregg A. Pre-eclampsia, birth weight, and autism spectrum disorders. J Autism Dev Disord. 2010; 40:548–54.
Article23. Cheslack-Postava K, Liu K, Bearman PS. Closely spaced pregnancies are associated with increased odds of autism in California sibling births. Pediatrics. 2011; 127:246–53.
Article24. Gunnes N, Suren P, Bresnahan M, Hornig M, Lie KK, Lipkin WI, et al. Interpregnancy interval and risk of autistic disorder. Epidemiology. 2013; 24:906–12.25. Zerbo O, Yoshida C, Gunderson EP, Dorward K, Croen LA. Interpregnancy interval and risk of autism spectrum disorders. Pediatrics. 2015; 136:651–7.26. Feingold KR, Anawalt B, Boyce A, Chrousos G, de Herder WW, Dhatariya K, et al. Endotext. South Dartmouth: MDText.com Inc;2000. Chapter, Thyroid hormones in brain development and function [cited 2022 Oct 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK285549.27. Rovet JF. The role of thyroid hormones for brain development and cognitive function. Endocr Dev. 2014; 26:26–43.28. Bernal J. Thyroid hormones and brain development. Vitam Horm. 2005; 71:95–122.
Article29. Lavado-Autric R, Auso E, Garcia-Velasco JV, Arufe Mdel C, Escobar del Rey F, Berbel P, et al. Early maternal hypothyroxinemia alters histogenesis and cerebral cortex cytoarchitecture of the progeny. J Clin Invest. 2003; 111:1073–82.
Article30. Stepien BK, Huttner WB. Transport, metabolism, and function of thyroid hormones in the developing mammalian brain. Front Endocrinol (Lausanne). 2019; 10:209.31. Ge GM, Leung MT, Man KK, Leung WC, Ip P, Li GH, et al. Maternal thyroid dysfunction during pregnancy and the risk of adverse outcomes in the offspring: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2020; 105:dgaa555.32. Brown AS, Surcel HM, Hinkka-Yli-Salomaki S, CheslackPostava K, Bao Y, Sourander A. Maternal thyroid autoantibody and elevated risk of autism in a national birth cohort. Prog Neuropsychopharmacol Biol Psychiatry. 2015; 57:86–92.
Article33. UN Environment Programme. Global chemicals outlook: towards sound management of chemicals. Nairobi: UNEP;2012. p. 44.34. Shin HM, Moschet C, Young TM, Bennett DH. Measured concentrations of consumer product chemicals in California house dust: implications for sources, exposure, and toxicity potential. Indoor Air. 2020; 30:60–75.35. Diamanti-Kandarakis E, Bourguignon JP, Giudice LC, Hauser R, Prins GS, Soto AM. Endocrine-disrupting chemicals: an endocrine society scientific statement. Endocr Rev. 2009; 30:293–342.36. Mughal BB, Fini JB, Demeneix BA. Thyroid-disrupting chemicals and brain development: an update. Endocr Connect. 2018; 7:R160–86.
Article37. La Merrill MA, Vandenberg LN, Smith MT, Goodson W, Browne P, Patisaul HB, et al. Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification. Nat Rev Endocrinol. 2020; 16:45–57.38. Brucker-Davis F. Effects of environmental synthetic chemicals on thyroid function. Thyroid. 1998; 8:827–56.39. Howdeshell KL. A model of the development of the brain as a construct of the thyroid system. Environ Health Perspect. 2002; 110 Suppl 3:337–48.40. Talsness CE. Overview of toxicological aspects of polybrominated diphenyl ethers: a flame-retardant additive in several consumer products. Environ Res. 2008; 108:158–67.
Article41. Moriyama K, Tagami T, Akamizu T, Usui T, Saijo M, Kanamoto N, et al. Thyroid hormone action is disrupted by bisphenol A as an antagonist. J Clin Endocrinol Metab. 2002; 87:5185–90.
Article42. Fritsche E, Cline JE, Nguyen NH, Scanlan TS, Abel J. Polychlorinated biphenyls disturb differentiation of normal human neural progenitor cells: clue for involvement of thyroid hormone receptors. Environ Health Perspect. 2005; 113:871–6.
Article43. Boas M, Feldt-Rasmussen U, Skakkebaek NE, Main KM. Environmental chemicals and thyroid function. Eur J Endocrinol. 2006; 154:599–611.
Article44. Prevedouros K, Cousins IT, Buck RC, Korzeniowski SH. Sources, fate and transport of perfluorocarboxylates. Environ Sci Technol. 2006; 40:32–44.45. Centers for Disease Control and Prevention. Fourth national report on human exposure to environmental chemicals. Atlanta: CDC;2015. [cited 2022 Oct 28]. Available from: https://www.cdc.gov/biomonitoring/pdf/fourthreport_updatedtables_feb2015.pdf.46. Fromme H, Mosch C, Morovitz M, Alba-Alejandre I, Boehmer S, Kiranoglu M, et al. Pre- and postnatal exposure to perfluorinated compounds (PFCs). Environ Sci Technol. 2010; 44:7123–9.
Article47. Monroy R, Morrison K, Teo K, Atkinson S, Kubwabo C, Stewart B, et al. Serum levels of perfluoroalkyl compounds in human maternal and umbilical cord blood samples. Environ Res. 2008; 108:56–62.
Article48. Jensen MS, Norgaard-Pedersen B, Toft G, Hougaard DM, Bonde JP, Cohen A, et al. Phthalates and perfluorooctanesulfonic acid in human amniotic fluid: temporal trends and timing of amniocentesis in pregnancy. Environ Health Perspect. 2012; 120:897–903.
Article49. Long M, Ghisari M, Kjeldsen L, Wielsoe M, NorgaardPedersen B, Mortensen EL, et al. Autism spectrum disorders, endocrine disrupting compounds, and heavy metals in amniotic fluid: a case-control study. Mol Autism. 2019; 10:1.
Article50. Boas M, Feldt-Rasmussen U, Main KM. Thyroid effects of endocrine disrupting chemicals. Mol Cell Endocrinol. 2012; 355:240–8.
Article51. Torres L, Redko A, Limper C, Imbiakha B, Chang S, August A. Effect of perfluorooctanesulfonic acid (PFOS) on immune cell development and function in mice. Immunol Lett. 2021; 233:31–41.
Article52. Guillette TC, McCord J, Guillette M, Polera ME, Rachels KT, Morgeson C, et al. Elevated levels of per- and polyfluoroalkyl substances in cape fear river striped bass (Morone saxatilis) are associated with biomarkers of altered immune and liver function. Environ Int. 2020; 136:105358.
Article53. Chang ET, Adami HO, Boffetta P, Wedner HJ, Mandel JS. A critical review of perfluorooctanoate and perfluorooctanesulfonate exposure and immunological health conditions in humans. Crit Rev Toxicol. 2016; 46:279–331.
Article54. Osuna CE, Grandjean P, Weihe P, El-Fawal HA. Autoantibodies associated with prenatal and childhood exposure to environmental chemicals in Faroese children. Toxicol Sci. 2014; 142:158–66.
Article55. Coperchini F, Awwad O, Rotondi M, Santini F, Imbriani M, Chiovato L. Thyroid disruption by perfluorooctane sulfonate (PFOS) and perfluorooctanoate (PFOA). J Endocrinol Invest. 2017; 40:105–21.
Article56. Hoffman K, Webster TF, Weisskopf MG, Weinberg J, Vieira VM. Exposure to polyfluoroalkyl chemicals and attention deficit/hyperactivity disorder in U.S. children 12-15 years of age. Environ Health Perspect. 2010; 118:1762–7.
Article57. Stein CR, Savitz DA. Serum perfluorinated compound concentration and attention deficit/hyperactivity disorder in children 5-18 years of age. Environ Health Perspect. 2011; 119:1466–71.
Article58. Ushijima J, Furukawa S, Sameshima H. The presence of thyroid peroxidase antibody is associated with lower placental weight in maternal thyroid dysfunction. Tohoku J Exp Med. 2019; 249:231–6.
Article59. Iddah MA, Macharia BN. Autoimmune thyroid disorders. ISRN Endocrinol. 2013; 2013:509764.
Article60. Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, et al. 2017 Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid. 2017; 27:315–89.
Article61. Andersen SL, Laurberg P, Wu CS, Olsen J. Attention deficit hyperactivity disorder and autism spectrum disorder in children born to mothers with thyroid dysfunction: a Danish nationwide cohort study. BJOG. 2014; 121:1365–74.
Article62. Rotem RS, Chodick G, Shalev V, Davidovitch M, Koren G, Hauser R, et al. Maternal thyroid disorders and risk of autism spectrum disorder in progeny. Epidemiology. 2020; 31:409–17.
Article63. Getahun D, Jacobsen SJ, Fassett MJ, Wing DA, Xiang AH, Chiu VY, et al. Association between maternal hypothyroidism and autism spectrum disorders in children. Pediatr Res. 2018; 83:580–8.
Article64. Roman GC, Ghassabian A, Bongers-Schokking JJ, Jaddoe VW, Hofman A, de Rijke YB, et al. Association of gestational maternal hypothyroxinemia and increased autism risk. Ann Neurol. 2013; 74:733–42.
Article65. Levie D, Korevaar TI, Bath SC, Dalmau-Bueno A, Murcia M, Espada M, et al. Thyroid function in early pregnancy, child IQ, and autistic traits: a meta-analysis of individual participant data. J Clin Endocrinol Metab. 2018; 103:2967–79.
Article66. Andersen SL, Andersen S, Vestergaard P, Olsen J. Maternal thyroid function in early pregnancy and child neurodevelopmental disorders: a Danish nationwide case-cohort study. Thyroid. 2018; 28:537–46.
Article67. Hoshiko S, Grether JK, Windham GC, Smith D, Fessel K. Are thyroid hormone concentrations at birth associated with subsequent autism diagnosis? Autism Res. 2011; 4:456–63.
Article68. Lyall K, Anderson M, Kharrazi M, Windham GC. Neonatal thyroid hormone levels in association with autism spectrum disorder. Autism Res. 2017; 10:585–92.
Article69. Korevaar TI, Tiemeier H, Peeters RP. Clinical associations of maternal thyroid function with foetal brain development: epidemiological interpretation and overview of available evidence. Clin Endocrinol (Oxf). 2018; 89:129–38.
Article70. Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB. Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr. 2016; 104 Suppl 3:918S–23S.
Article71. Tingi E, Syed AA, Kyriacou A, Mastorakos G, Kyriacou A. Benign thyroid disease in pregnancy: a state of the art review. J Clin Transl Endocrinol. 2016; 6:37–49.
Article72. Consortium on Thyroid and Pregnancy-Study Group on Preterm Birth, Korevaar TI, Derakhshan A, Taylor PN, Meima M, Chen L, et al. Association of thyroid function test abnormalities and thyroid autoimmunity with preterm birth: a systematic review and meta-analysis. JAMA. 2019; 322:632–41.
Article73. Derakhshan A, Peeters RP, Taylor PN, Bliddal S, Carty DM, Meems M, et al. Association of maternal thyroid function with birthweight: a systematic review and individual-participant data meta-analysis. Lancet Diabetes Endocrinol. 2020; 8:501–10.
Article74. Harel-Gadassi A, Friedlander E, Yaari M, Bar-Oz B, Eventov-Friedman S, Mankuta D, et al. Risk for ASD in preterm infants: a three-year follow-up study. Autism Res Treat. 2018; 2018:8316212.
Article75. Buchmayer S, Johansson S, Johansson A, Hultman CM, Sparen P, Cnattingius S. Can association between preterm birth and autism be explained by maternal or neonatal morbidity? Pediatrics. 2009; 124:e817–25.
Article76. Burstyn I, Sithole F, Zwaigenbaum L. Autism spectrum disorders, maternal characteristics and obstetric complications among singletons born in Alberta, Canada. Chronic Dis Can. 2010; 30:125–34.77. Lampi KM, Lehtonen L, Tran PL, Suominen A, Lehti V, Banerjee PN, et al. Risk of autism spectrum disorders in low birth weight and small for gestational age infants. J Pediatr. 2012; 161:830–6.
Article78. Hughes HK, Mills Ko E, Rose D, Ashwood P. Immune dysfunction and autoimmunity as pathological mechanisms in autism spectrum disorders. Front Cell Neurosci. 2018; 12:405.
Article79. Comi AM, Zimmerman AW, Frye VH, Law PA, Peeden JN. Familial clustering of autoimmune disorders and evaluation of medical risk factors in autism. J Child Neurol. 1999; 14:388–94.
Article80. Spann MN, Timonen-Soivio L, Suominen A, CheslackPostava K, McKeague IW, Sourander A, et al. Proband and familial autoimmune diseases are associated with proband diagnosis of autism spectrum disorders. J Am Acad Child Adolesc Psychiatry. 2019; 58:496–505.
Article81. Chen SW, Zhong XS, Jiang LN, Zheng XY, Xiong YQ, Ma SJ, et al. Maternal autoimmune diseases and the risk of autism spectrum disorders in offspring: a systematic review and meta-analysis. Behav Brain Res. 2016; 296:61–9.
Article82. Braunschweig D, Krakowiak P, Duncanson P, Boyce R, Hansen RL, Ashwood P, et al. Autism-specific maternal autoantibodies recognize critical proteins in developing brain. Transl Psychiatry. 2013; 3:e277.
Article83. Braunschweig D, Ashwood P, Krakowiak P, Hertz-Picciotto I, Hansen R, Croen LA, et al. Autism: maternally derived antibodies specific for fetal brain proteins. Neurotoxicology. 2008; 29:226–31.
Article84. Braunschweig D, Duncanson P, Boyce R, Hansen R, Ashwood P, Pessah IN, et al. Behavioral correlates of maternal antibody status among children with autism. J Autism Dev Disord. 2012; 42:1435–45.
Article85. Rossi CC, Fuentes J, Van de Water J, Amaral DG. Brief report: antibodies reacting to brain tissue in Basque Spanish children with autism spectrum disorder and their mothers. J Autism Dev Disord. 2014; 44:459–65.
Article86. Zimmerman AW, Connors SL, Matteson KJ, Lee LC, Singer HS, Castaneda JA, et al. Maternal antibrain antibodies in autism. Brain Behav Immun. 2007; 21:351–7.
Article87. Singer HS, Morris CM, Gause CD, Gillin PK, Crawford S, Zimmerman AW. Antibodies against fetal brain in sera of mothers with autistic children. J Neuroimmunol. 2008; 194:165–72.
Article88. Croen LA, Braunschweig D, Haapanen L, Yoshida CK, Fireman B, Grether JK, et al. Maternal mid-pregnancy autoantibodies to fetal brain protein: the early markers for autism study. Biol Psychiatry. 2008; 64:583–8.
Article89. Heuer L, Ashwood P, Schauer J, Goines P, Krakowiak P, Hertz-Picciotto I, et al. Reduced levels of immunoglobulin in children with autism correlates with behavioral symptoms. Autism Res. 2008; 1:275–83.
Article90. Grether JK, Ashwood P, Van de Water J, Yolken RH, Anderson MC, Torres AR, et al. Prenatal and newborn immunoglobulin levels from mother-child pairs and risk of autism spectrum disorders. Front Neurosci. 2016; 10:218.
Article91. Korevaar TI, Steegers EA, Pop VJ, Broeren MA, Chaker L, de Rijke YB, et al. Thyroid autoimmunity impairs the thyroidal response to human chorionic gonadotropin: two population-based prospective cohort studies. J Clin Endocrinol Metab. 2017; 102:69–77.92. Osinga JA, Derakhshan A, Palomaki GE, Ashoor G, Mannisto T, Maraka S, et al. TSH and FT4 reference intervals in pregnancy: a systematic review and individual participant data meta-analysis. J Clin Endocrinol Metab. 2022; 107:2925–33.
Article93. Braun JM, Kalkbrenner AE, Just AC, Yolton K, Calafat AM, Sjodin A, et al. Gestational exposure to endocrine-disrupting chemicals and reciprocal social, repetitive, and stereotypic behaviors in 4- and 5-year-old children: the HOME study. Environ Health Perspect. 2014; 122:513–20.
Article94. Liew Z, Ritz B, von Ehrenstein OS, Bech BH, Nohr EA, Fei C, et al. Attention deficit/hyperactivity disorder and childhood autism in association with prenatal exposure to perfluoroalkyl substances: a nested case-control study in the Danish national birth cohort. Environ Health Perspect. 2015; 123:367–73.
Article95. Lyall K, Yau VM, Hansen R, Kharrazi M, Yoshida CK, Calafat AM, et al. Prenatal maternal serum concentrations of per- and polyfluoroalkyl substances in association with autism spectrum disorder and intellectual disability. Environ Health Perspect. 2018; 126:017001.
Article96. Shin HM, Bennett DH, Calafat AM, Tancredi D, HertzPicciotto I. Modeled prenatal exposure to per- and polyfluoroalkyl substances in association with child autism spectrum disorder: a case-control study. Environ Res. 2020; 186:109514.
Article97. Oh J, Bennett DH, Calafat AM, Tancredi D, Roa DL, Schmidt RJ, et al. Prenatal exposure to per- and polyfluoroalkyl substances in association with autism spectrum disorder in the MARBLES study. Environ Int. 2021; 147:106328.
Article98. Skogheim TS, Weyde KV, Aase H, Engel SM, Suren P, Oie MG, et al. Prenatal exposure to per- and polyfluoroalkyl substances (PFAS) and associations with attention-deficit/hyperactivity disorder and autism spectrum disorder in children. Environ Res. 2021; 202:111692.
Article99. Kim S, Choi K, Ji K, Seo J, Kho Y, Park J, et al. Trans-placental transfer of thirteen perfluorinated compounds and relations with fetal thyroid hormones. Environ Sci Technol. 2011; 45:7465–72.
Article100. de Cock M, de Boer MR, Lamoree M, Legler J, van de Bor M. Prenatal exposure to endocrine disrupting chemicals in relation to thyroid hormone levels in infants: a Dutch prospective cohort study. Environ Health. 2014; 13:106.101. Wang Y, Rogan WJ, Chen PC, Lien GW, Chen HY, Tseng YC, et al. Association between maternal serum perfluoroalkyl substances during pregnancy and maternal and cord thyroid hormones: Taiwan maternal and infant cohort study. Environ Health Perspect. 2014; 122:529–34.
Article102. Berg V, Nost TH, Hansen S, Elverland A, Veyhe AS, Jorde R, et al. Assessing the relationship between perfluoroalkyl substances, thyroid hormones and binding proteins in pregnant women; a longitudinal mixed effects approach. Environ Int. 2015; 77:63–9.
Article103. Shah-Kulkarni S, Kim BM, Hong YC, Kim HS, Kwon EJ, Park H, et al. Prenatal exposure to perfluorinated compounds affects thyroid hormone levels in newborn girls. Environ Int. 2016; 94:607–13.
Article104. Berg V, Nost TH, Pettersen RD, Hansen S, Veyhe AS, Jorde R, et al. Persistent organic pollutants and the association with maternal and infant thyroid homeostasis: a multipollutant assessment. Environ Health Perspect. 2017; 125:127–33.
Article105. Preston EV, Webster TF, Oken E, Claus Henn B, McClean MD, Rifas-Shiman SL, et al. Maternal plasma per- and polyfluoroalkyl substance concentrations in early pregnancy and maternal and neonatal thyroid function in a prospective birth cohort: Project Viva (USA). Environ Health Perspect. 2018; 126:027013.
Article106. Itoh S, Araki A, Miyashita C, Yamazaki K, Goudarzi H, Minatoya M, et al. Association between perfluoroalkyl substance exposure and thyroid hormone/thyroid antibody levels in maternal and cord blood: the Hokkaido study. Environ Int. 2019; 133(Pt A):105139.
Article107. Preston EV, Webster TF, Claus Henn B, McClean MD, Gennings C, Oken E, et al. Prenatal exposure to per- and polyfluoroalkyl substances and maternal and neonatal thyroid function in the project viva cohort: a mixtures approach. Environ Int. 2020; 139:105728.
Article108. Lebeaux RM, Doherty BT, Gallagher LG, Zoeller RT, Hoofnagle AN, Calafat AM, et al. Maternal serum perfluoroalkyl substance mixtures and thyroid hormone concentrations in maternal and cord sera: the HOME study. Environ Res. 2020; 185:109395.
Article109. Liang H, Wang Z, Miao M, Tian Y, Zhou Y, Wen S, et al. Prenatal exposure to perfluoroalkyl substances and thyroid hormone concentrations in cord plasma in a Chinese birth cohort. Environ Health. 2020; 19:127.
Article110. Guo J, Zhang J, Wang Z, Zhang L, Qi X, Zhang Y, et al. Umbilical cord serum perfluoroalkyl substance mixtures in relation to thyroid function of newborns: findings from sheyang mini birth cohort study. Chemosphere. 2021; 273:129664.
Article111. Kim DH, Kim UJ, Kim HY, Choi SD, Oh JE. Perfluoroalkyl substances in serum from South Korean infants with congenital hypothyroidism and healthy infants: its relationship with thyroid hormones. Environ Res. 2016; 147:399–404.
Article112. Webster GM, Venners SA, Mattman A, Martin JW. Associations between perfluoroalkyl acids (PFASs) and maternal thyroid hormones in early pregnancy: a population-based cohort study. Environ Res. 2014; 133:338–47.
Article113. Webster GM, Rauch SA, Marie NS, Mattman A, Lanphear BP, Venners SA. Cross-sectional associations of serum perfluoroalkyl acids and thyroid hormones in U.S. adults: variation according to TPOAB and iodine status (NHANES 2007-2008). Environ Health Perspect. 2016; 124:935–42.
Article114. de Escobar GM, Obregon MJ, del Rey FE. Iodine deficiency and brain development in the first half of pregnancy. Public Health Nutr. 2007; 10:1554–70.
Article115. Bath SC, Steer CD, Golding J, Emmett P, Rayman MP. Effect of inadequate iodine status in UK pregnant women on cognitive outcomes in their children: results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Lancet. 2013; 382:331–7.
Article116. Valeri L, Vanderweele TJ. Mediation analysis allowing for exposure-mediator interactions and causal interpretation: theoretical assumptions and implementation with SAS and SPSS macros. Psychol Methods. 2013; 18:137–50.
Article117. Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol Methods. 2002; 7:422–45.
Article118. Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York: The Guilford Press;2013.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Translation of the Term 'Autism Spectrum Disorder' in Korean
- Environmental Factors in Autism and Autistic Spectrum Disorder
- Comparison of the Autism Diagnostic Observation Schedule and Childhood Autism Rating Scale in the Diagnosis of Autism Spectrum Disorder: A Preliminary Study
- Review of Early Intervention for Children with Autism Spectrum Disorder: Focused on Randomized Controlled Trials
- Association between Exposure to Endocrine Disrupting Chemicals in Breast Milk and Maternal Lifestyle Factor