J Korean Med Sci.
2022 Dec;37(49):e343. 10.3346/jkms.2022.37.e343.
Lifestyle Behaviors According to the Duration of Hypertension: Korea National Health and Nutrition Examination Survey 2016–2018
- Affiliations
-
- 1Department of Medical Bigdata Convergence, Kangwon National University, Chuncheon, Korea
- 2Department of Preventive Medicine, Kangwon National University College of Medicine, Chuncheon, Korea
- KMID: 2537044
- DOI: http://doi.org/10.3346/jkms.2022.37.e343
Abstract
- Background
The aim of this study was to examine the lifestyle characteristics of hypertensive patients and to investigate the association between the duration of hypertension and lifestyle characteristics.
Methods
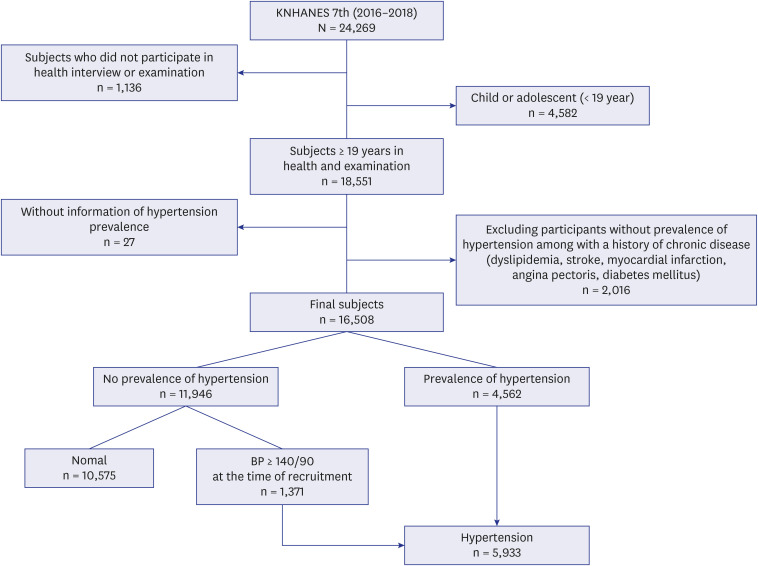
A total 16,508 adults (including 5,933 hypertensive patients) aged 20 years and older who participated in the 7th Korea National Health and Nutrition Examination Survey 2016–2018 were analyzed. Multiple logistic regression analysis was performed to examine the association between the duration of hypertension and lifestyle factors.
Results
The longer duration of hypertension was associated with lower risk of drinking in men (odds ratio [OR], 0.78; 95% confidence interval [CI], 0.66–0.93), and this observation remained when participants with hypertension for ≥ 13 years were compared to those with hypertension for < 1 year (OR, 0.57; 95% CI, 0.37–0.88). On the other hand, increased duration of hypertension increased the odds of engaging in high physical activity (PA) in women (OR, 1.72; 95% CI, 1.15–2.56), particularly in men with hypertension for 6–12 years (OR, 1.66; 95% CI, 1.03–2.69) and women with hypertension for ≥ 13 years (OR, 3.64; 95% CI, 1.38–9.62).
Conclusion
In conclusion, adoption and maintenance of healthy lifestyle habits, particularly drinking cessation in men, and PA in both men and women was observed, and differences were observed depending on the duration of hypertension.
Keyword
Figure
Reference
-
1. World Health Organization. Global status report on noncommunicable diseases 2014. Updated 2014. Accessed February 9, 2022. https://www.who.int/publications/i/item/9789241564854 .2. GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392(10159):1923–1994. PMID: 30496105.3. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021; 398(10304):957–980. PMID: 34450083.4. Korean Society Hypertension (KSH). Hypertension Epidemiology Research Working Group. Kim HC, Cho MC. Korea hypertension fact sheet 2018. Clin Hypertens. 2018; 24(1):13. PMID: 30288297.5. Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017; (289):1–8.6. Samadian F, Dalili N, Jamalian A. Lifestyle modifications to prevent and control hypertension. Iran J Kidney Dis. 2016; 10(5):237–263. PMID: 27721223.7. Dickey RA, Janick JJ. Lifestyle modifications in the prevention and treatment of hypertension. Endocr Pract. 2001; 7(5):392–399. PMID: 11585378.8. Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006; 29(8):1009–1014. PMID: 16944668.9. Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens. 2012; 25(3):335–341. PMID: 22052075.10. Diaz KM, Booth JN 3rd, Calhoun DA, Irvin MR, Howard G, Safford MM, et al. Healthy lifestyle factors and risk of cardiovascular events and mortality in treatment-resistant hypertension: the Reasons for Geographic and Racial Differences in Stroke study. Hypertension. 2014; 64(3):465–471. PMID: 24914189.11. Ayala C, Neff LJ, Croft JB, Keenan NL, Malarcher AM, Hyduk A, et al. Prevalence of self-reported high blood pressure awareness, advice received from health professionals, and actions taken to reduce high blood pressure among US adults--Healthstyles 2002. J Clin Hypertens (Greenwich). 2005; 7(9):513–519. PMID: 16227770.12. Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol. 2005; 23(34):8884–8893. PMID: 16314649.13. World Health Organization. Global physical activity questionnaire (GPAQ): analysis guide v2. Updated 2005. Accessed March 27, 2022. https://cdn.who.int/media/docs/default-source/ncds/ncd-surveillance/gpaq-analysis-guide.pdf .14. Korea Centers for Disease Control and Prevention. In-depth analyses of the Third National Health and Nutrition Examination Survey: the health interview and health behavior survey part. Updated 2007. Accessed December 13, 2021. https://scienceon.kisti.re.kr/commons/util/originalView.do?cn=TRKO201300000730&dbt=TRKO&rn= .15. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol. 2014; 43(1):69–77. PMID: 24585853.16. Kim H, Andrade FC. Diagnostic status and age at diagnosis of hypertension on adherence to lifestyle recommendations. Prev Med Rep. 2018; 13:52–56. PMID: 30510893.17. Neutel CI, Campbell N. Canadian Hypertension Society. Changes in lifestyle after hypertension diagnosis in Canada. Can J Cardiol. 2008; 24(3):199–204. PMID: 18340389.18. Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, Dennison Himmelfarb C, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71(6):1269–1324. PMID: 29133354.19. Korea Disease Control and Prevention Agency. Korea community health at a glance 2020: Korea Community Health Survey (KCHS). Updated 2021. Accessed June 2, 2022. https://chs.kdca.go.kr/chs/stats/statsMain.do .20. Ike SO, Aniebue PN, Aniebue UU. Knowledge, perceptions and practices of lifestyle-modification measures among adult hypertensives in Nigeria. Trans R Soc Trop Med Hyg. 2010; 104(1):55–60. PMID: 19733378.21. Silagy C, Muir J, Coulter A, Thorogood M, Yudkin P, Roe L. Lifestyle advice in general practice: rates recalled by patients. BMJ. 1992; 305(6858):871–874. PMID: 1422405.22. Ham OK, Yang SJ. Lifestyle factors associated with blood pressure control among those taking antihypertensive medication. Asia Pac J Public Health. 2011; 23(4):485–495. PMID: 19825840.23. Pescatello LS, Buchner DM, Jakicic JM, Powell KE, Kraus WE, Bloodgood B, et al. Physical activity to prevent and treat hypertension: a systematic review. Med Sci Sports Exerc. 2019; 51(6):1314–1323. PMID: 31095088.24. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003; 42(6):1206–1252. PMID: 14656957.25. Lee HY, Shin J, Kim GH, Park S, Ihm SH, Kim HC, et al. 2018 Korean Society of Hypertension guidelines for the management of hypertension: part II-diagnosis and treatment of hypertension. Clin Hypertens. 2019; 25(1):20. PMID: 31388453.26. Valderrama AL, Tong X, Ayala C, Keenan NL. Prevalence of self-reported hypertension, advice received from health care professionals, and actions taken to reduce blood pressure among US adults--HealthStyles, 2008. J Clin Hypertens (Greenwich). 2010; 12(10):784–792. PMID: 21029341.27. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 8th ed. Philadelphia, PA, USA: Lippincott Williams & Wilkins;2010.28. Barnes PM, Schoenborn CA. Trends in adults receiving a recommendation for exercise or other physical activity from a physician or other health professional. NCHS Data Brief. 2012; (86):1–8.29. Gangwisch JE, Heymsfield SB, Boden-Albala B, Buijs RM, Kreier F, Pickering TG, et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and Nutrition Examination Survey. Hypertension. 2006; 47(5):833–839. PMID: 16585410.30. Wang Q, Xi B, Liu M, Zhang Y, Fu M. Short sleep duration is associated with hypertension risk among adults: a systematic review and meta-analysis. Hypertens Res. 2012; 35(10):1012–1018. PMID: 22763475.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association between periodontal disease and hypertension using propensity score matching: results from the seventh (2016-2018) Korea National Health and Nutrition Examination Surve
- Trends in health behaviors over 20 years: findings from the 1998-2018 Korea National Health and Nutrition Examination Survey
- Decreased Health-Seeking Behaviors in People With Depressive Symptoms: The Korea National Health and Nutrition Examination Survey 2014, 2016, and 2018
- Relationship between Oral Health Care Behaviors and Perceived Periodontal Disease on Hypertension Patients
- The Influence of Family History of Hypertension on Hypertension Prevalence, Management and Healthy Behaviors among Korean Adults: Results from the Korea National Health and Nutrition Examination Survey 2014–2016