Cardiovasc Prev Pharmacother.
2021 Apr;3(2):38-46. 10.36011/cpp.2021.3.e6.
Geriatric Considerations in the Management of Elderly Patients with Cardiovascular Diseases
- Affiliations
-
- 1Department of Cardiovascular Medicine, Incheon St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Incheon, Korea
- 2Department of Cardiology, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2536945
- DOI: http://doi.org/10.36011/cpp.2021.3.e6
Abstract
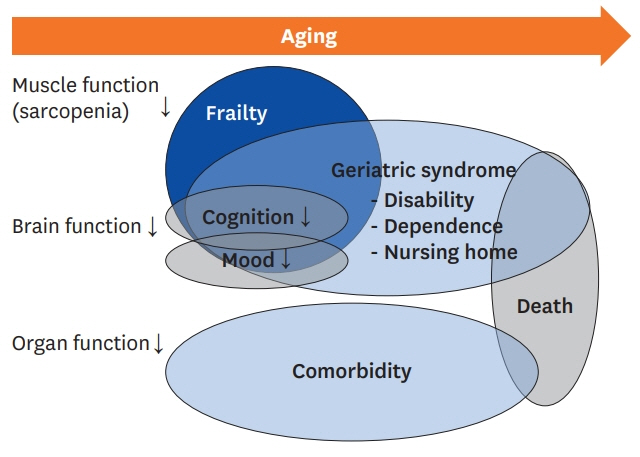
- Cardiovascular disease (CVD) is the most frequently diagnosed disease as well as the leading cause of death in the elderly. It usually results from long-term effects of cardiovascular risk factors as well as the aging process itself. Elderly people commonly have geriatric syndrome, which is an age-specific problem that is complicated by the presence of cardiovascular, cognitive, and physical dysfunction and is accompanied by many other chronic diseases. While caring for the elderly, in addition to CVD, various inherent problems must be considered. The patient-centered approach, instead of evidence-based guidelines that are designed for young adult patients, is the most important concept when it comes to elderly patients with CVD and multiple comorbidities. This approach should be used to maintain the functionality, independence, quality of life, and dignity of these patients.
Figure
Reference
-
1. Forman DE, Rich MW, Alexander KP, Zieman S, Maurer MS, Najjar SS, Cleveland JC Jr, Krumholz HM, Wenger NK. Cardiac care for older adults. Time for a new paradigm. J Am Coll Cardiol. 2011; 57:1801–10.2. Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises: Part II: the aging heart in health: links to heart disease. Circulation. 2003; 107:346–54.
Article3. Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: JACC health promotion series. J Am Coll Cardiol. 2018; 72:1141–56.4. Fleg JL, Strait J. Age-associated changes in cardiovascular structure and function: a fertile milieu for future disease. Heart Fail Rev. 2012; 17:545–54.
Article5. Fritze O, Romero B, Schleicher M, Jacob MP, Oh DY, Starcher B, Schenke-Layland K, Bujan J, Stock UA. Age-related changes in the elastic tissue of the human aorta. J Vasc Res. 2012; 49:77–86.
Article6. Meyer ML, Tanaka H, Palta P, Cheng S, Gouskova N, Aguilar D, Heiss G. Correlates of segmental pulse wave velocity in older adults: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens. 2016; 29:114–22.
Article7. Lloyd-Jones DM, Larson MG, Leip EP, Beiser A; D'Agostino RB, Kannel WB, Murabito JM, Vasan RS, Benjamin EJ; Levy D; Framingham Heart Study. Lifetime risk for developing congestive heart failure: the Framingham Heart Study. Circulation. 2002; 106:3068–72.
Article8. Redfield MM. Heart failure with preserved ejection fraction. N Engl J Med. 2016; 375:1868–77.
Article9. Iung B, Vahanian A. Degenerative calcific aortic stenosis: a natural history. Heart. 2012; 98 Suppl 4:iv7–13.
Article10. Klotz U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab Rev. 2009; 41:67–76.
Article11. Sera LC, McPherson ML. Pharmacokinetics and pharmacodynamic changes associated with aging and implications for drug therapy. Clin Geriatr Med. 2012; 28:273–86.
Article12. Montamat SC, Abernethy DR. Calcium antagonists in geriatric patients: diltiazem in elderly persons with hypertension. Clin Pharmacol Ther. 1989; 45:682–91.
Article13. White M, Roden R, Minobe W, Khan MF, Larrabee P, Wollmering M, Port JD, Anderson F, Campbell D, Feldman AM. Age-related changes in beta-adrenergic neuroeffector systems in the human heart. Circulation. 1994; 90:1225–38.
Article14. Stewart R. Cardiovascular disease and frailty: what are the mechanistic links? Clin Chem. 2019; 65:80–6.
Article15. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, Mitnitski A. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005; 173:489–95.
Article16. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G; McBurnie MA; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001; 56:M146–56.
Article17. Afilalo J, Lauck S, Kim DH, Lefèvre T, Piazza N, Lachapelle K, Martucci G, Lamy A, Labinaz M, Peterson MD, Arora RC, Noiseux N, Rassi A, Palacios IF; Généreux P, Lindman BR, Asgar AW, Kim CA, Trnkus A, Morais JA, Langlois Y, Rudski LG, Morin JF, Popma JJ, Webb JG, Perrault LP. Frailty in older adults undergoing aortic valve replacement: the FRAILTY-AVR study. J Am Coll Cardiol. 2017; 70:689–700.18. Boparai MK, Korc-Grodzicki B. Prescribing for older adults. Mt Sinai J Med. 2011; 78:613–26.
Article19. Odden MC, Peralta CA, Haan MN, Covinsky KE. Rethinking the association of high blood pressure with mortality in elderly adults: the impact of frailty. Arch Intern Med. 2012; 172:1162–8.20. Félix-Redondo FJ, Grau M; Fernández-Bergés D. Cholesterol and cardiovascular disease in the elderly. Facts and gaps. Aging Dis. 2013; 4:154–69.21. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010; 138:1093–100.
Article22. Scott IA, Hilmer SN, Reeve E, Potter K, Le Couteur D, Rigby D, Gnjidic D, Del Mar CB, Roughead EE, Page A, Jansen J, Martin JH. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015; 175:827–34.23. Feldman RD, Harris SB, Hegele RA, Pickering JG, Rockwood K. Applying atherosclerotic risk prevention guidelines to elderly patients: a bridge too far? Can J Cardiol. 2016; 32:598–602.
Article