Ann Surg Treat Res.
2023 Aug;105(2):63-68. 10.4174/astr.2023.105.2.63.
Surgical management for elderly patients with pancreatic cancer
- Affiliations
-
- 1Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- KMID: 2545156
- DOI: http://doi.org/10.4174/astr.2023.105.2.63
Abstract
- Pancreatic cancer, one of the diseases of the elderly, has dismal prognosis, demanding major surgery with high risk and life quality problems, especially in the elderly. Therefore, treatment selection, whether or not to undergo surgery, preoperative risk assessment, and perioperative management of the elderly are becoming critical issues. Although the elderly are expected to have higher morbidity and mortality and lower long-term survival outcomes, surgery is becoming safer over time. Appropriate surgical indication selection, patient-centered decision-making, adequate prehabilitation and postoperative geriatric care are expected to improve surgical outcomes in the elderly. Surgeons must have the concept of geriatric care, and efforts based on institutional systems and academic societies are required. If well selected and prepared, the same surgical principle as non-elderly patients can be applied to elderly patients. In this paper, the surgical treatment of elderly patients with pancreatic cancer is reviewed.
Figure
Reference
-
1. Population Division, Department of Economic and Social Affairs, United Nations. World population prospects: the 2008 revision. Volume II. Sex and age distribution of the world population. United Nations Publication;2009. Available from: https://www.un.org/development/desa/pd/sites/www.un.org.development.desa.pd/files/files/documents/2020/Jan/un_2008_world_population_prospects-2008_revision_volume-ii.pdf .2. Kang MJ, Lim J, Han SS, Park HM, Park SJ, Won YJ, et al. First course of treatment and prognosis of exocrine pancreatic cancer in Korea from 2006 to 2017. Cancer Res Treat. 2022; 54:208–217. PMID: 34030432.
Article3. Riall TS, Reddy DM, Nealon WH, Goodwin JS. The effect of age on short-term outcomes after pancreatic resection: a population-based study. Ann Surg. 2008; 248:459–467. PMID: 18791366.4. Finlayson E, Fan Z, Birkmeyer JD. Outcomes in octogenarians undergoing high-risk cancer operation: a national study. J Am Coll Surg. 2007; 205:729–734. PMID: 18035254.
Article5. van der Geest LG, Besselink MG, van Gestel YR, Busch OR, de Hingh IH, de Jong KP, et al. Pancreatic cancer surgery in elderly patients: balancing between short-term harm and long-term benefit: a population-based study in the Netherlands. Acta Oncol. 2016; 55:278–285. PMID: 26552841.
Article6. Wang H, Liu J, Xia G, Lei S, Huang X, Huang X. Survival of pancreatic cancer patients is negatively correlated with age at diagnosis: a population-based retrospective study. Sci Rep. 2020; 10:7048. PMID: 32341400.
Article7. Park HM, Park SJ, Han SS, Kim SH. Surgery for elderly patients with resectable pancreatic cancer, a comparison with non-surgical treatments: a retrospective study outcomes of resectable pancreatic cancer. BMC Cancer. 2019; 19:1090. PMID: 31718565.
Article8. Satoi S, Yamamoto T, Uchida K, Fujii T, Kin T, Hirano S, et al. Optimal treatment for octogenarians with resectable and borderline resectable pancreatic ductal adenocarcinoma: a multicenter retrospective study. Pancreas. 2020; 49:837–844. PMID: 32590619.
Article9. Kang JS, Kim H, Kim JR, Han Y, Kim E, Byun Y, et al. Short- and long-term outcomes of pancreaticoduodenectomy in elderly patients with periampullary cancer. Ann Surg Treat Res. 2020; 98:7–14. PMID: 31909045.
Article10. Tan E, Song J, Lam S, D’Souza M, Crawford M, Sandroussi C. Postoperative outcomes in elderly patients undergoing pancreatic resection for pancreatic adenocarcinoma: a systematic review and meta-analysis. Int J Surg. 2019; 72:59–68. PMID: 31580919.
Article11. Meltzer RS, Kooby DA, Switchenko JM, Datta J, Carpizo DR, Maithel SK, et al. Does major pancreatic surgery have utility in nonagenarians with pancreas cancer? Ann Surg Oncol. 2021; 28:2265–2272. PMID: 33141373.
Article12. Wildiers H, Heeren P, Puts M, Topinkova E, Janssen-Heijnen ML, Extermann M, et al. International Society of Geriatric Oncology consensus on geriatric assessment in older patients with cancer. J Clin Oncol. 2014; 32:2595–2603. PMID: 25071125.
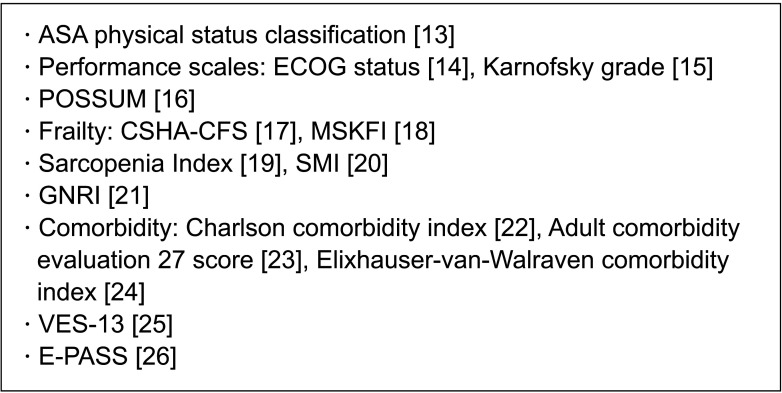
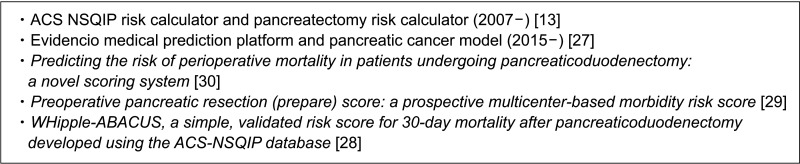
Article13. American College of Surgeons (ACS). ACS NSQIP Surgical risk calculator [Internet]. ACS National Surgical Quality Improvement Program;c2007-2023. cited 2022 Dec 1. Available from: https://riskcalculator.facs.org/RiskCalculator/PatientInfo.jsp .14. Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982; 5:649–655. PMID: 7165009.
Article15. Karnofsky DA, Abelmann WH, Craver LF, Burchenal JH. The use of the nitrogen mustards in the palliative treatment of carcinoma: with particular reference to bronchogenic carcinoma. Cancer. 1948; 1:634–656.
Article16. Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991; 78:355–360. PMID: 2021856.
Article17. Rockwood K, Song X, MacKnight C, Bergman H, Hogan DB, McDowell I, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005; 173:489–495. PMID: 16129869.
Article18. Shahrokni A, Tin A, Alexander K, Sarraf S, Afonso A, Filippova O, et al. Development and evaluation of a new frailty index for older surgical patients with cancer. JAMA Netw Open. 2019; 2:e193545. PMID: 31074814.
Article19. Kashani KB, Frazee EN, Kukrálová L, Sarvottam K, Herasevich V, Young PM, et al. Evaluating muscle mass by using markers of kidney function: development of the sarcopenia index. Crit Care Med. 2017; 45:e23–e29. PMID: 27611976.
Article20. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–896. PMID: 12028177.
Article21. Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, et al. Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr. 2005; 82:777–783. PMID: 16210706.
Article22. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383. PMID: 3558716.
Article23. Piccirillo JF, Creech CM, Zequeira R, Anderson S, Johnston AS. Inclusion of comorbidity into oncology data registries. J Regist Manag. 1999; 26:66–70.24. van Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009; 47:626–633. PMID: 19433995.
Article25. Saliba D, Orlando M, Wenger NS, Hays RD, Rubenstein LZ. Identifying a short functional disability screen for older persons. J Gerontol A Biol Sci Med Sci. 2000; 55:M750–M756. PMID: 11129398.
Article26. Haga Y, Ikei S, Ogawa M. Estimation of Physiologic Ability and Surgical Stress (E-PASS) as a new prediction scoring system for postoperative morbidity and mortality following elective gastrointestinal surgery. Surg Today. 1999; 29:219–225. PMID: 10192731.
Article27. Evidencio Medical Decision Support. Risk of complications in patients following pancreaticoduodenectomy [Internet]. Evidencio Community;2018. cited 2022 Dec 1. Available from: https://www.evidencio.com/models/show/1198 .28. Gleeson EM, Shaikh MF, Shewokis PA, Clarke JR, Meyers WC, Pitt HA, et al. WHipple-ABACUS, a simple, validated risk score for 30-day mortality after pancreaticoduodenectomy developed using the ACS-NSQIP database. Surgery. 2016; 160:1279–1287. PMID: 27544541.
Article29. Uzunoglu FG, Reeh M, Vettorazzi E, Ruschke T, Hannah P, Nentwich MF, et al. Preoperative Pancreatic Resection (PREPARE) score: a prospective multicenter-based morbidity risk score. Ann Surg. 2014; 260:857–864. PMID: 25243549.30. Venkat R, Puhan MA, Schulick RD, Cameron JL, Eckhauser FE, Choti MA, et al. Predicting the risk of perioperative mor tal it y in pat ients undergoing pancreaticoduodenectomy: a novel scoring system. Arch Surg. 2011; 146:1277–1284. PMID: 22106320.
Article31. Winer A, Dotan E. Treatment paradigms for older adults with pancreatic cancer: a nuanced approach. Curr Treat Options Oncol. 2021; 22:104. PMID: 34596801.
Article32. Kondo N, Uemura K, Nakagawa N, Okada K, Seo S, Takahashi S, et al. Reappraisal of the validity of surgery for patients with pancreatic cancer aged 80 years or older stratified by resectability status. J Hepatobiliary Pancreat Sci. 2020; 27:64–74. PMID: 31602815.
Article33. Sho M, Murakami Y, Kawai M, Motoi F, Satoi S, Matsumoto I, et al. Prognosis after surgical treatment for pancreatic cancer in patients aged 80 years or older: a multicenter study. J Hepatobiliary Pancreat Sci. 2016; 23:188–197. PMID: 26763744.
Article34. Weniger M, Moir J, Damm M, Maggino L, Kordes M, Rosendahl J, et al. Neoadjuvant therapy in elderly patients receiving FOLFIRINOX or gemcitabine/nab-paclitaxel for borderline resectable or locally advanced pancreatic cancer is feasible and lead to a similar oncological outcome compared to non-aged patients: results of the RESPECT-Study. Surg Oncol. 2020; 35:285–297. PMID: 32949968.
Article35. Rieser CJ, Zenati M, Narayanan S, Bahary N, Lee KK, Paniccia A, et al. Optimal management of resectable pancreatic head cancer in the elderly patient: does neoadjuvant therapy offer a survival benefit? Ann Surg Oncol. 2021; 28:6264–6272. PMID: 33748894.
Article36. Rieser CJ, Narayanan S, Bahary N, Bartlett DL, Lee KK, Paniccia A, et al. Optimal management of patients with operable pancreatic head cancer: a Markov decision analysis. J Surg Oncol. 2021; 124:801–809. PMID: 34231222.
Article37. Cooper AB, Holmes HM, des Bordes JK, Fogelman D, Parker NH, Lee JE, et al. Role of neoadjuvant therapy in the multimodality treatment of older patients with pancreatic cancer. J Am Coll Surg. 2014; 219:111–120. PMID: 24856952.
Article38. Chesney TR, Schwarze ML. Patient-centered surgical decision making. Rosenthal RA, Zenilman ME, Katlic MR, editors. Principles and practice of geriatric surgery. Springer International Publishing;2020. p. 81–93.39. Zhang W, Huang Z, Zhang J, Che X. Effect of laparoscopic pancreaticoduodenectomy in elderly people: a meta-analysis. Pancreas. 2021; 50:1154–1162. PMID: 34714278.
Article40. Zhu J, Wang G, Du P, He J, Li Y. Minimally invasive pancreaticoduodenectomy in elderly patients: systematic review and meta-analysis. World J Surg. 2021; 45:1186–1201. PMID: 33458781.
Article41. Kanda M, Fujii T, Suenaga M, Takami H, Inokawa Y, Yamada S, et al. Pancreatoduodenectomy with portal vein resection is feasible and potentially beneficial for elderly patients with pancreatic cancer. Pancreas. 2014; 43:951–958. PMID: 24717827.
Article42. Fang JZ, Lu CD, Wu SD, Huang J, Zhou J. Portal vein/superior mesenteric vein resection in pancreatic cancer treatment in the elderly. Medicine (Baltimore). 2017; 96:e7335. PMID: 28682880.
Article43. Jegatheeswaran S, Baltatzis M, Jamdar S, Siriwardena AK. Superior mesenteric artery (SMA) resection during pancreatectomy for malignant disease of the pancreas: a systematic review. HPB (Oxford). 2017; 19:483–490. PMID: 28410913.
Article44. Wang X, Dong Y, Jin J, Liu Q, Zhan Q, Chen H, et al. Efficacy of modified Appleby surgery: a benefit for elderly patients? J Surg Res. 2015; 194:83–90. PMID: 25311939.
Article45. Melloul E, Lassen K, Roulin D, Grass F, Perinel J, Adham M, et al. Guidelines for perioperative care for pancreatoduodenectomy: enhanced recovery after surgery (ERAS) recommendations 2019. World J Surg. 2020; 44:2056–2084. PMID: 32161987.
Article46. Ji HB, Zhu WT, Wei Q, Wang XX, Wang HB, Chen QP. Impact of enhanced recovery after surgery programs on pancreatic surgery: a meta-analysis. World J Gastroenterol. 2018; 24:1666–1678. PMID: 29686474.47. Raza SS, Nutu OA, Powell-Brett S, Carvalheiro Boteon A, Hodson J, Abradelo M, et al. Impact of an enhanced recovery after surgery protocol on short-term outcomes in elderly patients undergoing pancreaticoduodenectomy. HPB (Oxford). 2022; 24:1720–1728. PMID: 35643908.48. Bongers BC, Dejong CH, den Dulk M. Enhanced recovery after surgery programmes in older patients undergoing hepatopancreatobiliary surgery: what benefits might prehabilitation have? Eur J Surg Oncol. 2021; 47(3 Pt A):551–559. PMID: 32253075.49. McDonald SR, Heflin MT, Whitson HE, Dalton TO, Lidsky ME, Liu P, et al. Association of integrated care coordination with postsurgical outcomes in high-risk older adults: the Perioperative Optimization of Senior Health (POSH) Initiative. JAMA Surg. 2018; 153:454–462. PMID: 29299599.
Article50. Talarico L, Chen G, Pazdur R. Enrollment of elderly patients in clinical trials for cancer drug registration: a 7-year experience by the US Food and Drug Administration. J Clin Oncol. 2004; 22:4626–4631. PMID: 15542812.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relief of Cancer Pain in Patients with Pancreatic Cancer
- Impact of Surgery on Oligometastatic Pancreatic Cancer: Current Status and Future Perspectives
- Pancreaticoduodenectomy of Pancreatic Ductal Adenocarcinoma in the Elderly
- Management of Borderline Resectable Pancreatic Cancer and Local Treatment of Locally Advanced Pancreatic Cancer
- Prevalence, Diagnosis and Management of Pancreatic Cystic Neoplasms: Current Status and Future Directions