J Liver Cancer.
2022 Sep;22(2):202-206. 10.17998/jlc.2022.09.17.
Multidisciplinary approach for hepatocellular carcinoma arising from cirrhotic liver with Budd-Chiari syndrome: a case report
- Affiliations
-
- 1Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2534248
- DOI: http://doi.org/10.17998/jlc.2022.09.17
Abstract
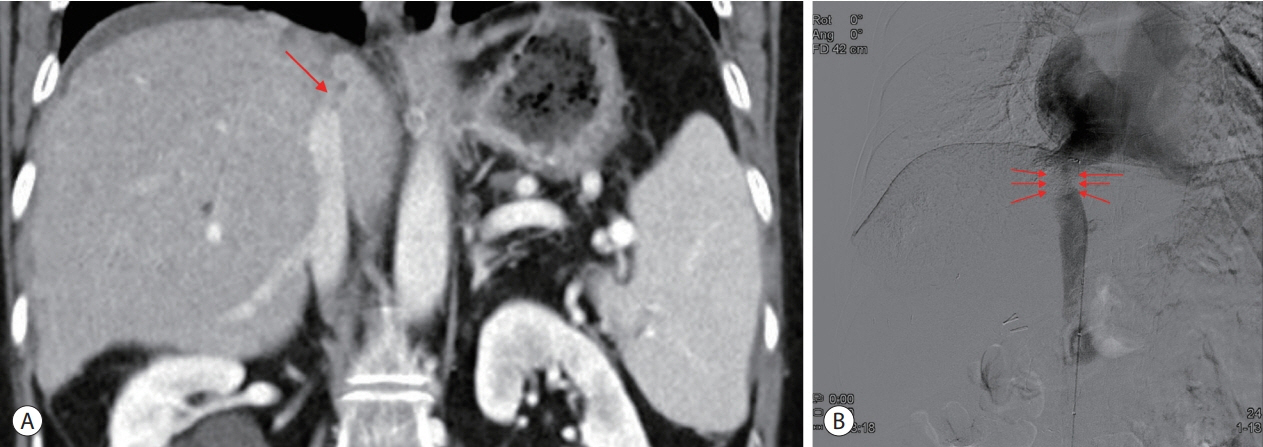
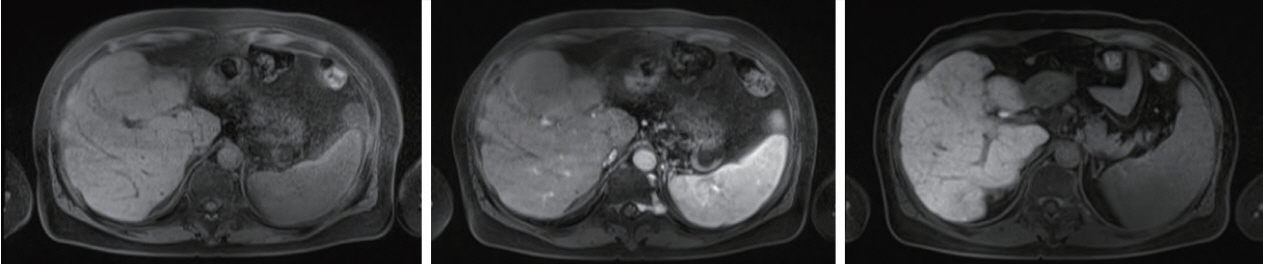
- Budd-Chiari syndrome (BCS) is defined by the obstruction of the hepatic venous outflow between the small hepatic veins and the junction of the inferior vena cava (IVC) with the right atrium. BCS with IVC obstruction occasionally progresses to hepatocellular carcinoma (HCC). Here, we report the case of a patient with HCC arising from a cirrhotic liver with BCS, in whom the hepatic portion of the IVC was obstructed, and who had a favorable outcome with a multidisciplinary approach and IVC balloon angioplasty.
Keyword
Figure
Reference
-
1. Goel RM, Johnston EL, Patel KV, Wong T. Budd-Chiari syndrome: investigation, treatment and outcomes. Postgrad Med J. 2015; 91:692–697.2. Matsui S, Ichida T, Watanabe M, Sugitani S, Suda T, Takahashi T, et al. Clinical features and etiology of hepatocellular carcinoma arising in patients with membranous obstruction of the inferior vena cava: in reference to hepatitis viral infection. J Gastroenterol Hepatol. 2000; 15:1205–1211.3. Darwish Murad S, Plessier A, Hernandez-Guerra M, Fabris F, Eapen CE, Bahr MJ, et al. Etiology, management, and outcome of the Budd-Chiari syndrome. Ann Intern Med. 2009; 151:167–175.4. Valla DC. Budd-Chiari syndrome and veno-occlusive disease/sinusoidal obstruction syndrome. Gut. 2008; 57:1469–1478.5. DeLeve LD, Valla DC, Garcia-Tsao G; American Association for the Study Liver Diseases. Vascular disorders of the liver. Hepatology. 2009; 49:1729–1764.6. Shin SH, Chung YH, Suh DD, Shin JW, Jang MK, Ryu SH, et al. Characteristic clinical features of hepatocellular carcinoma associated with Budd-Chiari syndrome: evidence of different carcinogenic process from hepatitis B virus-associated hepatocellular carcinoma. Eur J Gastroenterol Hepatol. 2004; 16:319–324.7. Shrestha SM, Okuda K, Uchida T, Maharjan KG, Shrestha S, Joshi BL, et al. Endemicity and clinical picture of liver disease due to obstruction of the hepatic portion of the inferior vena cava in Nepal. J Gastroenterol Hepatol. 1996; 11:170–179.8. Qi X, Zhang C, Han G, Zhang W, He C, Yin Z, et al. Prevalence of the JAK2V617F mutation in Chinese patients with Budd-Chiari syndrome and portal vein thrombosis: a prospective study. J Gastroenterol Hepatol. 2012; 27:1036–1043.9. Oliveri RS, Wetterslev J, Gluud C. Hepatocellular carcinoma. Lancet. 2012; 380:470. author reply 470-1.10. Sung PS. Crosstalk between tumor-associated macrophages and neighboring cells in hepatocellular carcinoma. Clin Mol Hepatol. 2022; 28:333–350.11. Lambert MP, Paliwal A, Vaissière T, Chemin I, Zoulim F, Tommasino M, et al. Aberrant DNA methylation distinguishes hepatocellular carcinoma associated with HBV and HCV infection and alcohol intake. J Hepatol. 2011; 54:705–715.12. Stickel F, Hampe J. Genetic determinants of alcoholic liver disease. Gut. 2012; 61:150–159.13. Krawczyk M, Bonfrate L, Portincasa P. Nonalcoholic fatty liver disease. Best Pract Res Clin Gastroenterol. 2010; 24:695–708.14. Liang Y, Yang Z, Zhong R. Primary biliary cirrhosis and cancer risk: a systematic review and meta-analysis. Hepatology. 2012; 56:1409–1417.15. El-Serag HB. Hepatocellular carcinoma. N Engl J Med. 2011; 365:1118–1127.16. Gwon D 2nd, Ko GY, Yoon HK, Sung KB, Kim JH, Lee SS, et al. Hepatocellular carcinoma associated with membranous obstruction of the inferior vena cava: incidence, characteristics, and risk factors and clinical efficacy of TACE. Radiology. 2010; 254:617–626.17. Shrestha SM. Liver cirrhosis and hepatocellular carcinoma in hepatic vena cava disease, a liver disease caused by obstruction of inferior vena cava. Hepatol Int. 2009; 3:392–402.18. Sung PS, Oh JS, Choi JI. Acute Budd-Chiari syndrome with thrombotic thrombocytopenia after BNT162b2 mRNA vaccination. Liver Int. 2022; 42:1447–1448.19. Kew MC, McKnight A, Hodkinson J, Bukofzer S, Esser JD. The role of membranous obstruction of the inferior vena cava in the etiology of hepatocellular carcinoma in Southern African blacks. Hepatology. 1989; 9:121–125.20. Martens P, Nevens F. Budd-Chiari syndrome. United European Gastroenterol J. 2015; 3:489–500.21. Valla D, Hadengue A, el Younsi M, Azar N, Zeitoun G, Boudet MJ, et al. Hepatic venous outflow block caused by short-length hepatic vein stenoses. Hepatology. 1997; 25:814–819.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Budd-Chiari syndrome with hepatocellular carcinoma
- A Case of Budd Chiari Syndrome Caused by Membraneous Obstruction of Suprahepatic Inferior Vena Cava
- Budd-Chiari syndrome with multiple large regenerative nodules
- Budd-Chiari Syndrome: Right hepatic vein obstruction and incomplete IVC obstruction with azygos continuation of IVC
- A Case of Budd-Chiari Syndrome with IVC Web Treated by Balloon Dilatation