Endocrinol Metab.
2022 Aug;37(4):587-598. 10.3803/EnM.2022.1528.
Long-Term Outcomes of Congenital Adrenal Hyperplasia
- Affiliations
-
- 1Department of Women’s and Children’s Health, Karolinska Institute, Stockholm, Sweden
- 2Pediatric Endocrinology Unit, Karolinska University Hospital, Stockholm, Sweden
- 3Department of Molecular Medicine and Surgery, Karolinska Institute, Stockholm, Sweden
- 4Department of Endocrinology, Karolinska University Hospital, Stockholm, Sweden
- KMID: 2532858
- DOI: http://doi.org/10.3803/EnM.2022.1528
Abstract
- A plethora of negative long-term outcomes have been associated with congenital adrenal hyperplasia (CAH). The causes are multiple and involve supra-physiological gluco- and mineralocorticoid replacement, excess adrenal androgens both intrauterine and postnatal, elevated steroid precursor and adrenocorticotropic hormone levels, living with a congenital condition as well as the proximity of the cytochrome P450 family 21 subfamily A member 2 (CYP21A2) gene to other genes. This review aims to discuss the different long-term outcomes of CAH.
Figure
Reference
-
1. Gidlof S, Falhammar H, Thilen A, von Dobeln U, Ritzen M, Wedell A, et al. One hundred years of congenital adrenal hyperplasia in Sweden: a retrospective, population-based cohort study. Lancet Diabetes Endocrinol. 2013; 1:35–42.
Article2. Arlt W, Willis DS, Wild SH, Krone N, Doherty EJ, Hahner S, et al. Health status of adults with congenital adrenal hyperplasia: a cohort study of 203 patients. J Clin Endocrinol Metab. 2010; 95:5110–21.
Article3. Claahsen-van der Grinten HL, Speiser PW, Ahmed SF, Arlt W, Auchus RJ, Falhammar H, et al. Congenital adrenal hyperplasia: current insights in pathophysiology, diagnostics, and management. Endocr Rev. 2022; 43:91–159.4. Kocova M, Concolino P, Falhammar H. Characteristics of In2G variant in congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Front Endocrinol (Lausanne). 2022; 12:788812.
Article5. Merke DP, Auchus RJ. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency. N Engl J Med. 2020; 383:1248–61.
Article6. Kocova M, Anastasovska V, Falhammar H. Clinical outcomes and characteristics of P30L mutations in congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocrine. 2020; 69:262–77.
Article7. Espinosa Reyes TM, Collazo Mesa T, Lantigua Cruz PA, Agramonte Machado A, Dominguez Alonso E, Falhammar H. Molecular diagnosis of patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. BMC Endocr Disord. 2020; 20:165.
Article8. Speiser PW, Arlt W, Auchus RJ, Baskin LS, Conway GS, Merke DP, et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2018; 103:4043–88.
Article9. Nordenstrom A, Falhammar H. Management of endocrine disease: diagnosis and management of the patient with nonclassic CAH due to 21-hydroxylase deficiency. Eur J Endocrinol. 2019; 180:R127–45.10. Falhammar H, Wedell A, Nordenstrom A. Biochemical and genetic diagnosis of 21-hydroxylase deficiency. Endocrine. 2015; 50:306–14.
Article11. Zetterstrom RH, Karlsson L, Falhammar H, Lajic S, Nordenstrom A. Update on the Swedish newborn screening for congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Int J Neonatal Screen. 2020; 6:71.
Article12. Nordenstrom A, Ahmed S, Jones J, Coleman M, Price DA, Clayton PE, et al. Female preponderance in congenital adrenal hyperplasia due to CYP21 deficiency in England: implications for neonatal screening. Horm Res. 2005; 63:22–8.
Article13. Falhammar H, Nordenstrom A. Nonclassic congenital adrenal hyperplasia due to 21-hydroxylase deficiency: clinical presentation, diagnosis, treatment, and outcome. Endocrine. 2015; 50:32–50.
Article14. Nordenstrom A, Falhammar H, Lajic S. Current and novel treatment strategies in children with congenital adrenal hyperplasia. Horm Res Paediatr. 2022; Jan. 27. [Epub]. https://doi.org/10.1159/000522260.
Article15. Nordenstrom A, Lajic S, Falhammar H. Clinical outcomes in 21-hydroxylase deficiency. Curr Opin Endocrinol Diabetes Obes. 2021; 28:318–24.
Article16. Falhammar H, Thoren M. Clinical outcomes in the management of congenital adrenal hyperplasia. Endocrine. 2012; 41:355–73.
Article17. Whittle E, Falhammar H. Glucocorticoid regimens in the treatment of congenital adrenal hyperplasia: a systematic review and meta-analysis. J Endocr Soc. 2019; 3:1227–45.
Article18. Gomes LG, Mendonca BB, Bachega TA. Long-term cardio-metabolic outcomes in patients with classical congenital adrenal hyperplasia: is the risk real? Curr Opin Endocrinol Diabetes Obes. 2020; 27:155–61.
Article19. Eugster EA, Dimeglio LA, Wright JC, Freidenberg GR, Seshadri R, Pescovitz OH. Height outcome in congenital adrenal hyperplasia caused by 21-hydroxylase deficiency: a meta-analysis. J Pediatr. 2001; 138:26–32.
Article20. Muthusamy K, Elamin MB, Smushkin G, Murad MH, Lampropulos JF, Elamin KB, et al. Clinical review: Adult height in patients with congenital adrenal hyperplasia: a systematic review and metaanalysis. J Clin Endocrinol Metab. 2010; 95:4161–72.21. Van der Kamp HJ, Otten BJ, Buitenweg N, De Muinck Keizer-Schrama SM, Oostdijk W, Jansen M, et al. Longitudinal analysis of growth and puberty in 21-hydroxylase deficiency patients. Arch Dis Child. 2002; 87:139–44.
Article22. Balsamo A, Cicognani A, Baldazzi L, Barbaro M, Baronio F, Gennari M, et al. CYP21 genotype, adult height, and pubertal development in 55 patients treated for 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2003; 88:5680–8.
Article23. Falhammar H, Filipsson H, Holmdahl G, Janson PO, Nordenskjold A, Hagenfeldt K, et al. Metabolic profile and body composition in adult women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2007; 92:110–6.
Article24. Falhammar H, Filipsson H, Holmdahl G, Janson PO, Nordenskjold A, Hagenfeldt K, et al. Increased liver enzymes in adult women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Endocr J. 2009; 56:601–8.
Article25. Falhammar H, Filipsson Nystrom H, Wedell A, Thoren M. Cardiovascular risk, metabolic profile, and body composition in adult males with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Eur J Endocrinol. 2011; 164:285–93.
Article26. Finkielstain GP, Kim MS, Sinaii N, Nishitani M, Van Ryzin C, Hill SC, et al. Clinical characteristics of a cohort of 244 patients with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2012; 97:4429–38.
Article27. Falhammar H, Frisen L, Hirschberg AL, Norrby C, Almqvist C, Nordenskjold A, et al. Increased cardiovascular and metabolic morbidity in patients with 21-hydroxylase deficiency: a Swedish Population-Based National Cohort Study. J Clin Endocrinol Metab. 2015; 100:3520–8.
Article28. Torky A, Sinaii N, Jha S, Desai J, El-Maouche D, Mallappa A, et al. Cardiovascular disease risk factors and metabolic morbidity in a longitudinal study of congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2021; 106:e5247–57.
Article29. Tamhane S, Rodriguez-Gutierrez R, Iqbal AM, Prokop LJ, Bancos I, Speiser PW, et al. Cardiovascular and metabolic outcomes in congenital adrenal hyperplasia: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2018; 103:4097–103.
Article30. Falhammar H, Claahsen-van der Grinten H, Reisch N, Slowikowska-Hilczer J, Nordenstrom A, Roehle R, et al. Health status in 1040 adults with disorders of sex development (DSD): a European multicenter study. Endocr Connect. 2018; 7:466–78.
Article31. Bonfig W, Roehl FW, Riedl S, Dorr HG, Bettendorf M, Bramswig J, et al. Blood pressure in a large cohort of children and adolescents with classic adrenal hyperplasia (CAH) due to 21-hydroxylase deficiency. Am J Hypertens. 2016; 29:266–72.
Article32. Lim SG, Lee YA, Jang HN, Kong SH, Ahn CH, Kim SW, et al. Long-term health outcomes of Korean adults with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Front Endocrinol (Lausanne). 2021; 12:761258.
Article33. Kim JH, Choi S, Lee YA, Lee J, Kim SG. Epidemiology and long-term adverse outcomes in Korean patients with congenital adrenal hyperplasia: a nationwide study. Endocrinol Metab (Seoul). 2022; 37:138–47.
Article34. Bachelot A, Golmard JL, Dulon J, Dahmoune N, Leban M, Bouvattier C, et al. Determining clinical and biological indicators for health outcomes in adult patients with childhood onset of congenital adrenal hyperplasia. Eur J Endocrinol. 2015; 173:175–84.
Article35. Hagenfeldt K, Janson PO, Holmdahl G, Falhammar H, Filipsson H, Frisen L, et al. Fertility and pregnancy outcome in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Reprod. 2008; 23:1607–13.
Article36. Hirschberg AL, Gidlof S, Falhammar H, Frisen L, Almqvist C, Nordenskjold A, et al. Reproductive and perinatal outcomes in women with congenital adrenal hyperplasia: a population-based cohort study. J Clin Endocrinol Metab. 2021; 106:e957–65.
Article37. Badeghiesh A, Ismail S, Baghlaf H, Suarthana E, Dahan MH. Pregnancy, delivery and neonatal outcomes among women with congenital adrenal hyperplasia: a study of a large US database. Reprod Biomed Online. 2020; 41:1093–9.
Article38. Bouvattier C, Esterle L, Renoult-Pierre P, de la Perriere AB, Illouz F, Kerlan V, et al. Clinical outcome, hormonal status, gonadotrope axis, and testicular function in 219 adult men born with classic 21-hydroxylase deficiency: a French National Survey. J Clin Endocrinol Metab. 2015; 100:2303–13.
Article39. Mooij CF, Kroese JM, Sweep FC, Hermus AR, Tack CJ. Adult patients with congenital adrenal hyperplasia have elevated blood pressure but otherwise a normal cardiovascular risk profile. PLoS One. 2011; 6:e24204.
Article40. Kannel WB, Kannel C, Paffenbarger RS Jr, Cupples LA. Heart rate and cardiovascular mortality: the Framingham Study. Am Heart J. 1987; 113:1489–94.
Article41. Mensink GB, Hoffmeister H. The relationship between resting heart rate and all-cause, cardiovascular and cancer mortality. Eur Heart J. 1997; 18:1404–10.
Article42. Naqvi TZ, Lee MS. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. 2014; 7:1025–38.43. Sartorato P, Zulian E, Benedini S, Mariniello B, Schiavi F, Bilora F, et al. Cardiovascular risk factors and ultrasound evaluation of intima-media thickness at common carotids, carotid bulbs, and femoral and abdominal aorta arteries in patients with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2007; 92:1015–8.
Article44. Wasniewska M, Balsamo A, Valenzise M, Manganaro A, Faggioli G, Bombaci S, et al. Increased large artery intima media thickness in adolescents with either classical or nonclassical congenital adrenal hyperplasia. J Endocrinol Invest. 2013; 36:12–5.45. Zimmermann A, Sido PG, Schulze E, Al Khzouz C, Lazea C, Coldea C, et al. Bone mineral density and bone turnover in Romanian children and young adults with classical 21-hydroxylase deficiency are influenced by glucocorticoid replacement therapy. Clin Endocrinol (Oxf). 2009; 71:477–84.
Article46. Sciannamblo M, Russo G, Cuccato D, Chiumello G, Mora S. Reduced bone mineral density and increased bone metabolism rate in young adult patients with 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2006; 91:4453–8.
Article47. Falhammar H, Filipsson H, Holmdahl G, Janson PO, Nordenskjold A, Hagenfeldt K, et al. Fractures and bone mineral density in adult women with 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2007; 92:4643–9.
Article48. Falhammar H, Filipsson Nystrom H, Wedell A, Brismar K, Thoren M. Bone mineral density, bone markers, and fractures in adult males with congenital adrenal hyperplasia. Eur J Endocrinol. 2013; 168:331–41.
Article49. El-Maouche D, Collier S, Prasad M, Reynolds JC, Merke DP. Cortical bone mineral density in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Clin Endocrinol (Oxf). 2015; 82:330–7.
Article50. Espinosa Reyes TM, Leyva Gonzalez G, Dominguez Alonso E, Falhammar H. Bone mass in young patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Horm Res Paediatr. 2021; 94:1–8.
Article51. Riehl G, Reisch N, Roehle R, Claahsen van der Grinten H, Falhammar H, Quinkler M. Bone mineral density and fractures in congenital adrenal hyperplasia: findings from the dsd-LIFE study. Clin Endocrinol (Oxf). 2020; 92:284–94.
Article52. Hagenfeldt K, Martin Ritzen E, Ringertz H, Helleday J, Carlstrom K. Bone mass and body composition of adult women with congenital virilizing 21-hydroxylase deficiency after glucocorticoid treatment since infancy. Eur J Endocrinol. 2000; 143:667–71.
Article53. Lee DH, Kong SH, Jang HN, Ahn CH, Lim SG, Lee YA, et al. Association of androgen excess and bone mineral density in women with classical congenital adrenal hyperplasia with 21-hydroxylase deficiency. Arch Osteoporos. 2022; 17:45.
Article54. Rangaswamaiah S, Gangathimmaiah V, Nordenstrom A, Falhammar H. Bone mineral density in adults with congenital adrenal hyperplasia: a systematic review and metaanalysis. Front Endocrinol (Lausanne). 2020; 11:493.
Article55. Chakhtoura Z, Bachelot A, Samara-Boustani D, Ruiz JC, Donadille B, Dulon J, et al. Impact of total cumulative glucocorticoid dose on bone mineral density in patients with 21-hydroxylase deficiency. Eur J Endocrinol. 2008; 158:879–87.
Article56. Chotiyarnwong P, McCloskey EV. Pathogenesis of glucocorticoid-induced osteoporosis and options for treatment. Nat Rev Endocrinol. 2020; 16:437–47.
Article57. Li L, Bensing S, Falhammar H. Rate of fracture in patients with glucocorticoid replacement therapy: a systematic review and meta-analysis. Endocrine. 2021; 74:29–37.
Article58. Falhammar H, Frisen L, Hirschberg AL, Nordenskjold A, Almqvist C, Nordenstrom A. Increased prevalence of fractures in congenital adrenal hyperplasia: a Swedish population-based national cohort study. J Clin Endocrinol Metab. 2022; 107:e475–86.
Article59. Falhammar H, Butwicka A, Landen M, Lichtenstein P, Nordenskjold A, Nordenstrom A, et al. Increased psychiatric morbidity in men with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2014; 99:E554–60.
Article60. Engberg H, Butwicka A, Nordenstrom A, Hirschberg AL, Falhammar H, Lichtenstein P, et al. Congenital adrenal hyperplasia and risk for psychiatric disorders in girls and women born between 1915 and 2010: a total population study. Psychoneuroendocrinology. 2015; 60:195–205.
Article61. Jenkins-Jones S, Parviainen L, Porter J, Withe M, Whitaker MJ, Holden SE, et al. Poor compliance and increased mortality, depression and healthcare costs in patients with congenital adrenal hyperplasia. Eur J Endocrinol. 2018; 178:309–20.
Article62. Karlsson L, Barbaro M, Ewing E, Gomez-Cabrero D, Lajic S. Epigenetic alterations associated with early prenatal dexamethasone treatment. J Endocr Soc. 2018; 3:250–63.
Article63. Lao Q, Jardin MD, Jayakrishnan R, Ernst M, Merke DP. Complement component 4 variations may influence psychopathology risk in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Hum Genet. 2018; 137:955–60.
Article64. Falhammar H, Frisen L, Hirschberg AL, Nordenskjold A, Almqvist C, Nordenstrom A. Increased risk of autoimmune disorders in 21-hydroxylase deficiency: a Swedish population-based national cohort study. J Endocr Soc. 2019; 3:1039–52.
Article65. Patrova J, Jarocka I, Wahrenberg H, Falhammar H. Clinical outcomes in adrenal incidentaloma: experience from one center. Endocr Pract. 2015; 21:870–7.
Article66. Falhammar H. Non-functioning adrenal incidentalomas caused by 21-hydroxylase deficiency or carrier status? Endocrine. 2014; 47:308–14.
Article67. Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, et al. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016; 175:G1–34.
Article68. Calissendorff J, Juhlin CC, Sundin A, Bancos I, Falhammar H. Adrenal myelolipomas. Lancet Diabetes Endocrinol. 2021; 9:767–75.
Article69. Falhammar H, Torpy DJ. Congenital adrenal hyperplasia due to 21-hydroxylase deficiency presenting as adrenal incidentaloma: a systematic review and meta-analysis. Endocr Pract. 2016; 22:736–52.
Article70. Nermoen I, Falhammar H. Prevalence and characteristics of adrenal tumors and myelolipomas in congenital adrenal hyperplasia: a systematic review and meta-analysis. Endocr Pract. 2020; 26:1351–65.
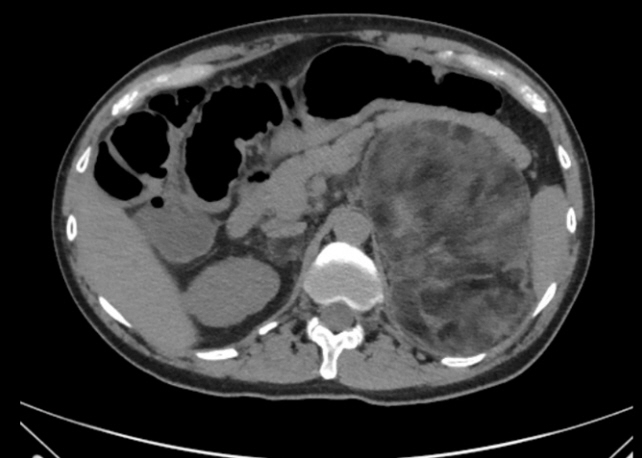
Article71. Kim TM, Kim JH, Jang HN, Choi MH, Cho JY, Kim SY. Adrenal morphology as an indicator of long-term disease control in adults with classic 21-hydroxylase deficiency. Endocrinol Metab (Seoul). 2022; 37:124–37.
Article72. Engels M, Span PN, van Herwaarden AE, Sweep FC, Stikkelbroeck NM, Claahsen-van der Grinten HL. Testicular adrenal rest tumors: current insights on prevalence, characteristics, origin, and treatment. Endocr Rev. 2019; 40:973–87.
Article73. Falhammar H, Nystrom HF, Ekstrom U, Granberg S, Wedell A, Thoren M. Fertility, sexuality and testicular adrenal rest tumors in adult males with congenital adrenal hyperplasia. Eur J Endocrinol. 2012; 166:441–9.
Article74. Engels M, Gehrmann K, Falhammar H, Webb EA, Nordenstrom A, Sweep FC, et al. Gonadal function in adult male patients with congenital adrenal hyperplasia. Eur J Endocrinol. 2018; 178:285–94.
Article75. Avila NA, Premkumar A, Merke DP. Testicular adrenal rest tissue in congenital adrenal hyperplasia: comparison of MR imaging and sonographic findings. AJR Am J Roentgenol. 1999; 172:1003–6.
Article76. Claahsen-van der Grinten HL, Stikkelbroeck N, Falhammar H, Reisch N. Management of endocrine disease: gonadal dysfunction in congenital adrenal hyperplasia. Eur J Endocrinol. 2021; 184:R85–97.77. Burman P, Falhammar H, Waldenstrom E, Sundin A, Bitzen U. 11C-Metomidate PET/CT detected multiple ectopic adrenal rest tumors in a woman with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2021; 106:e675. –9.
Article78. MacKay D, Nordenstrom A, Falhammar H. Bilateral adrenalectomy in congenital adrenal hyperplasia: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2018; 103:1767–78.
Article79. Falhammar H, Frisen L, Norrby C, Hirschberg AL, Almqvist C, Nordenskjold A, et al. Increased mortality in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2014; 99:E2715–21.
Article80. Dorr HG, Wollmann HA, Hauffa BP, Woelfle J; German Society of Pediatric Endocrinology and Diabetology. Mortality in children with classic congenital adrenal hyperplasia and 21-hydroxylase deficiency (CAH) in Germany. BMC Endocr Disord. 2018; 18:37.
Article81. Burger-Stritt S, Kardonski P, Pulzer A, Meyer G, Quinkler M, Hahner S. Management of adrenal emergencies in educated patients with adrenal insufficiency: a prospective study. Clin Endocrinol (Oxf). 2018; 89:22–9.82. Rushworth RL, Torpy DJ, Falhammar H. Adrenal crisis. N Engl J Med. 2019; 381:852–61.
Article83. Rushworth RL, Torpy DJ, Stratakis CA, Falhammar H. Adrenal crises in children: perspectives and research directions. Horm Res Paediatr. 2018; 89:341–51.
Article84. Rushworth RL, Torpy DJ, Falhammar H. Adrenal crises in older patients. Lancet Diabetes Endocrinol. 2020; 8:628–39.
Article85. Rushworth RL, Chrisp GL, Bownes S, Torpy DJ, Falhammar H. Adrenal crises in adolescents and young adults. Endocrine. 2022; 77:1–10.
Article86. Volkl TM, Ohl L, Rauh M, Schofl C, Dorr HG. Adrenarche and puberty in children with classic congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Horm Res Paediatr. 2011; 76:400–10.
Article87. Labarta E, Martinez-Conejero JA, Alama P, Horcajadas JA, Pellicer A, Simon C, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis. Hum Reprod. 2011; 26:1813–25.
Article88. Nordenskjold A, Holmdahl G, Frisen L, Falhammar H, Filipsson H, Thoren M, et al. Type of mutation and surgical procedure affect long-term quality of life for women with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2008; 93:380–6.
Article89. Reisch N. Pregnancy in congenital adrenal hyperplasia. Endocrinol Metab Clin North Am. 2019; 48:619–41.
Article90. Daae E, Feragen KB, Waehre A, Nermoen I, Falhammar H. Sexual orientation in individuals with congenital adrenal hyperplasia: a systematic review. Front Behav Neurosci. 2020; 14:38.
Article91. Frisen L, Nordenstrom A, Falhammar H, Filipsson H, Holmdahl G, Janson PO, et al. Gender role behavior, sexuality, and psychosocial adaptation in women with congenital adrenal hyperplasia due to CYP21A2 deficiency. J Clin Endocrinol Metab. 2009; 94:3432–9.92. Nordenstrom A, Frisen L, Falhammar H, Filipsson H, Holmdahl G, Janson PO, et al. Sexual function and surgical outcome in women with congenital adrenal hyperplasia due to CYP21A2 deficiency: clinical perspective and the patients’ perception. J Clin Endocrinol Metab. 2010; 95:3633–40.93. Casteràs A, De Silva P, Rumsby G, Conway GS. Reassessing fecundity in women with classical congenital adrenal hyperplasia (CAH): normal pregnancy rate but reduced fertility rate. Clin Endocrinol (Oxf). 2009; 70:833–7.
Article94. Jaaskelainen J, Hippelainen M, Kiekara O, Voutilainen R. Child rate, pregnancy outcome and ovarian function in females with classical 21-hydroxylase deficiency. Acta Obstet Gynecol Scand. 2000; 79:687–92.
Article95. Słowikowska-Hilczer J, Hirschberg AL, Claahsen-van der Grinten H, Reisch N, Bouvattier C, Thyen U, et al. Fertility outcome and information on fertility issues in individuals with different forms of disorders of sex development: findings from the dsd-LIFE study. Fertil Steril. 2017; 108:822–31.
Article96. Falhammar H, Nystrom HF, Thoren M. Quality of life, social situation, and sexual satisfaction, in adult males with congenital adrenal hyperplasia. Endocrine. 2014; 47:299–307.
Article97. Reisch N, Flade L, Scherr M, Rottenkolber M, Pedrosa Gil F, Bidlingmaier M, et al. High prevalence of reduced fecundity in men with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2009; 94:1665–70.
Article98. Falhammar H, Frisen L, Norrby C, Almqvist C, Hirschberg AL, Nordenskjold A, et al. Reduced frequency of biological and increased frequency of adopted children in males with 21-hydroxylase deficiency: a Swedish population-based national cohort study. J Clin Endocrinol Metab. 2017; 102:4191–9.
Article99. Cabrera MS, Vogiatzi MG, New MI. Long term outcome in adult males with classic congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2001; 86:3070–8.
Article100. Jaaskelainen J, Kiekara O, Hippelainen M, Voutilainen R. Pituitary gonadal axis and child rate in males with classical 21-hydroxylase deficiency. J Endocrinol Invest. 2000; 23:23–7.
Article101. Messina V, Karlsson L, Hirvikoski T, Nordenstrom A, Lajic S. Cognitive function of children and adolescents with congenital adrenal hyperplasia: importance of early diagnosis. J Clin Endocrinol Metab. 2020; 105:e683–91.
Article102. Herting MM, Azad A, Kim R, Tyszka JM, Geffner ME, Kim MS. Brain differences in the prefrontal cortex, amygdala, and hippocampus in youth with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2020; 105:1098–111.
Article103. Browne WV, Hindmarsh PC, Pasterski V, Hughes IA, Acerini CL, Spencer D, et al. Working memory performance is reduced in children with congenital adrenal hyperplasia. Horm Behav. 2015; 67:83–8.
Article104. Karlsson L, Gezelius A, Nordenstrom A, Hirvikoski T, Lajic S. Cognitive impairment in adolescents and adults with congenital adrenal hyperplasia. Clin Endocrinol (Oxf). 2017; 87:651–9.
Article105. Hamed SA, Metwalley KA, Farghaly HS. Cognitive function in children with classic congenital adrenal hyperplasia. Eur J Pediatr. 2018; 177:1633–40.
Article106. Berenbaum SA, Bryk KK, Duck SC. Normal intelligence in female and male patients with congenital adrenal hyperplasia. Int J Pediatr Endocrinol. 2010; 2010:853103.
Article107. Webb EA, Elliott L, Carlin D, Wilson M, Hall K, Netherton J, et al. Quantitative brain MRI in congenital adrenal hyperplasia: in vivo assessment of the cognitive and structural impact of steroid hormones. J Clin Endocrinol Metab. 2018; 103:1330–41.
Article108. Van’t Westeinde A, Karlsson L, Thomsen Sandberg M, Nordenstrom A, Padilla N, Lajic S. Altered gray matter structure and white matter microstructure in patients with congenital adrenal hyperplasia: relevance for working memory performance. Cereb Cortex. 2020; 30:2777–88.
Article109. Nordenstrom A, Butwicka A, Linden Hirschberg A, Almqvist C, Nordenskjold A, Falhammar H, et al. Are carriers of CYP21A2 mutations less vulnerable to psychological stress?: a population-based national cohort study. Clin Endocrinol (Oxf). 2017; 86:317–24.110. Strandqvist A, Falhammar H, Lichtenstein P, Hirschberg AL, Wedell A, Norrby C, et al. Suboptimal psychosocial outcomes in patients with congenital adrenal hyperplasia: epidemiological studies in a nonbiased national cohort in Sweden. J Clin Endocrinol Metab. 2014; 99:1425–32.
Article111. Daae E, Feragen KB, Nermoen I, Falhammar H. Psychological adjustment, quality of life, and self-perceptions of reproductive health in males with congenital adrenal hyperplasia: a systematic review. Endocrine. 2018; 62:3–13.
Article112. Verhees MJ, Engels M, Span PN, Sweep FC, van Herwaarden AE, Falhammar H, et al. Quality of life in men with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Front Endocrinol (Lausanne). 2021; 12:626646.
Article113. Nermoen I, Husebye ES, Svartberg J, Lovas K. Subjective health status in men and women with congenital adrenal hyperplasia: a population-based survey in Norway. Eur J Endocrinol. 2010; 163:453–9.
Article114. Reisch N, Hahner S, Bleicken B, Flade L, Pedrosa Gil F, Loeffler M, et al. Quality of life is less impaired in adults with congenital adrenal hyperplasia because of 21-hydroxylase deficiency than in patients with primary adrenal insufficiency. Clin Endocrinol (Oxf). 2011; 74:166–73.
Article115. Almasri J, Zaiem F, Rodriguez-Gutierrez R, Tamhane SU, Iqbal AM, Prokop LJ, et al. Genital reconstructive surgery in females with congenital adrenal hyperplasia: a systematic review and meta-analysis. J Clin Endocrinol Metab. 2018; 103:4089–96.
Article116. Gehrmann K, Engels M, Bennecke E, Bouvattier C, Falhammar H, Kreukels BP, et al. Sexuality in males with congenital adrenal hyperplasia resulting from 21-hydroxylase deficiency. J Endocr Soc. 2019; 3:1445–56.
Article117. Nygren U, Sodersten M, Falhammar H, Thoren M, Hagenfeldt K, Nordenskjold A. Voice characteristics in women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Clin Endocrinol (Oxf). 2009; 70:18–25.
Article118. Nygren U, Nystrom HF, Falhammar H, Hagenfeldt K, Nordenskjold A, Sodersten M. Voice problems due to virilization in adult women with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. Clin Endocrinol (Oxf). 2013; 79:859–66.
Article119. Nygren U, Sodersten M, Thyen U, Kohler B, Nordenskjold A; dsd-LIFE Group. Voice dissatisfaction in individuals with a disorder of sex development. Clin Endocrinol (Oxf). 2019; 91:219–27.
Article120. Lao Q, Brookner B, Merke DP. High-throughput screening for CYP21A1P-TNXA/TNXB chimeric genes responsible for ehlers-danlos syndrome in patients with congenital adrenal hyperplasia. J Mol Diagn. 2019; 21:924–31.
Article121. Gao Y, Lu L, Yu B, Mao J, Wang X, Nie M, et al. The prevalence of the chimeric TNXA/TNXB gene and clinical symptoms of ehlers-danlos syndrome with 21-hydroxylase deficiency. J Clin Endocrinol Metab. 2020; 105:dgaa199.122. Marino R, Garrido NP, Ramirez P, Notaristefano G, Moresco A, Touzon MS, et al. Ehlers-Danlos syndrome: molecular and clinical characterization of TNXA/TNXB chimeras in congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2021; 106:e2789–802.123. Concolino P, Falhammar H. CAH-X syndrome: genetic and clinical profile. Mol Diagn Ther. 2022; 26:293–300.
Article124. Miller WL, Merke DP. Tenascin-X, congenital adrenal hyperplasia, and the CAH-X syndrome. Horm Res Paediatr. 2018; 89:352–61.
Article125. Lajic S, Karlsson L, Zetterstrom RH, Falhammar H, Nordenstrom A. The success of a screening program is largely dependent on close collaboration between the laboratory and the clinical follow-up of the patients. Int J Neonatal Screen. 2020; 6:68.
Article126. Prete A, Auchus RJ, Ross RJ. Clinical advances in the pharmacotherapy of congenital adrenal hyperplasia. Eur J Endocrinol. 2021; 186:R1–14.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of adrenocortical adenoma following long-term treatment in a patient with congenital adrenal hyperplasia
- A Case of Congenital Lipoid Adrenal Hyperplasia: Early Diagnosis by Using Computed Tomography
- Management of Congenital Adrenal Hyperplasia
- Congenital adrenal Hyperplasia
- Genotype-phenotype Correlations in Congenital Adrenal hyperplasia