J Korean Neurosurg Soc.
2022 Jul;65(4):591-597. 10.3340/jkns.2021.0164.
Arachnoid Remodeling by Clipping Technique Facilitates Surgical Maneuverability during Transsphenoidal Surgery for Pituitary Macroadenoma
- Affiliations
-
- 1Department of Neurosurgery, Yonsei University College of Medicine, Seoul, Korea
- 2Pituitary Tumor Center, Severance Hospital, Seoul, Korea
- 3Yonsei Endocrine Research Institute, Yonsei University College of Medicine, Seoul, Korea
- 4Department of Neurosurgery, Ewha Woman’s University College of Medicine, Seoul, Korea
- 5Department of Neurosurgery, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2531628
- DOI: http://doi.org/10.3340/jkns.2021.0164
Abstract
Objective
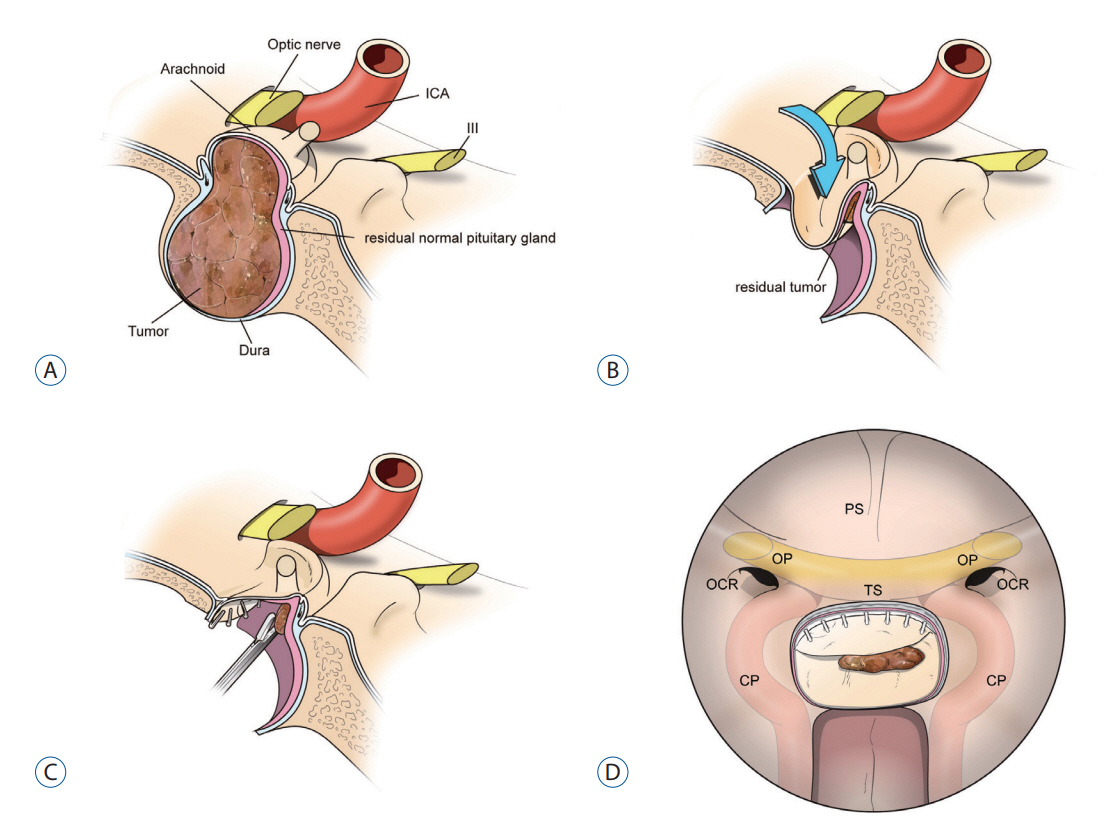
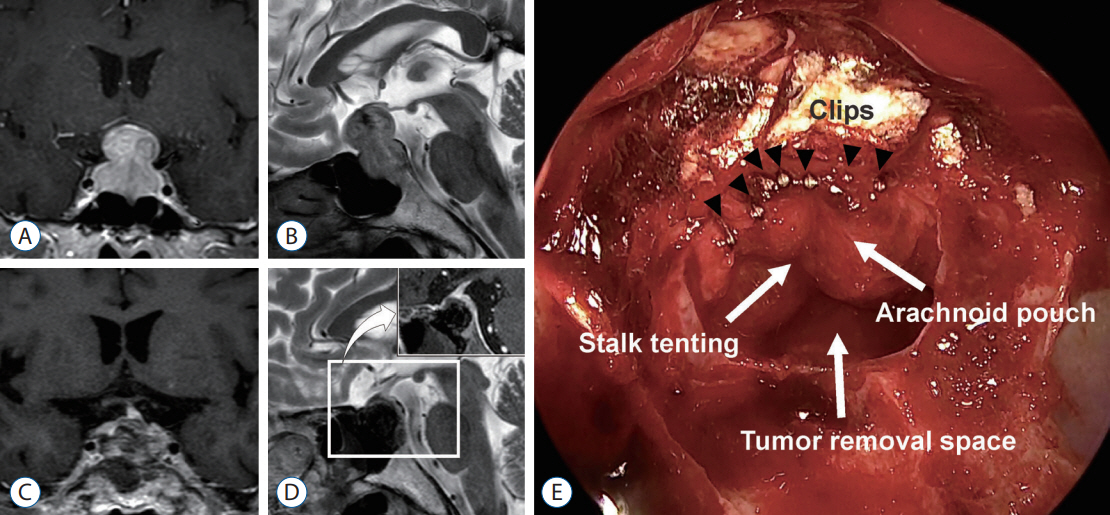
: Pituitary adenomas frequently extend into the suprasellar space. After a suprasellar tumor is removed, the superiorly extended arachnoid becomes redundant and sinks down into the intrasellar space which often hiders visualization and accessibility to the hidden space behind the evaginated arachnoid. We introduced arachnoid remodeling by clipping technique, and evaluated its usefulness and safety during TSS.
Methods
: Total 223 patients who underwent arachnoid remodeling with our new clipping technique were included. Redundant arachnoid was clipped along the dural edge with multiple 2.6-mm titanium clips until the redundant arachnoid membrane no longer blocked the surgical route. To check for possible deterioration of hormonal function by this technique, we assessed anterior pituitary function of 166 patients who underwent arachnoid remodeling by clipping and compared this with those of other 429 control patients.
Results
: Our technique greatly enhanced the accessibility and visualization of intrasellar and parasellar spaces, both of which are generally hindered by redundant arachnoid during transsphenoidal surgery (TSS). We found no difference in anterior pituitary function between a clip-assisted arachnoid remodeling group and the control group, implying that this technique does not result in hypopituitarism.
Conclusion
: During TSS for pituitary adenomas with suprasellar extension, arachnoid remodeling by clipping technique is very useful and convenient for the management of the redundant arachnoid membrane to enhance visualization and surgical accessibility.
Keyword
Figure
Reference
-
References
1. Barzaghi LR, Losa M, Giovanelli M, Mortini P. Complications of transsphenoidal surgery in patients with pituitary adenoma: experience at a single centre. Acta Neurochir (Wien). 149:877–885. 2007.
Article2. Ciric I, Ragin A, Baumgartner C, Pierce D. Complications of transsphenoidal surgery: results of a national survey, review of the literature, and personal experience. Neurosurgery. 40:225–237. 1997.
Article3. Decker RE, Chalif DJ. Progressive coma after the transsphenoidal decompression of a pituitary adenoma with marked suprasellar extension: report of two cases. Neurosurgery. 28:154–157. 1991.
Article4. Kim EH, Ku CR, Lee EJ, Kim SH. Extracapsular en bloc resection in pituitary adenoma surgery. Pituitary. 18:397–404. 2015.
Article5. Kim EH, Moon JH, Kim SH. Clipping technique for the repair of the intraoperative cerebrospinal fluid leakage during transsphenoidal pituitary tumor surgery. Oper Neurosurg (Hagerstown). 17:382–388. 2019.
Article6. Kim EH, Oh MC, Kim SH. Angiographically documented cerebral vasospasm following transsphenoidal surgery for pituitary tumors. Pituitary. 16:260–269. 2013.
Article7. Kim EH, Oh MC, Kim SH. Application of low-field intraoperative magnetic resonance imaging in transsphenoidal surgery for pituitary adenomas: technical points to improve the visibility of the tumor resection margin. Acta Neurochir (Wien). 155:485–493. 2013.
Article8. Kitano M, Taneda M. Capsule plication as a protective measure against post-operative intracapsular haematoma formation following transsphenoidal removal of pituitary macroadenoma. Acta Neurochir (Wien). 150:797–802. 2008.
Article9. Ku CR, Kim EH, Oh MC, Lee EJ, Kim SH. Surgical and endocrinological outcomes in the treatment of growth hormone-secreting pituitary adenomas according to the shift of surgical paradigm. Neurosurgery. 71(2 Suppl Operative):ons192–ons203. 2012.
Article10. Kurwale NS, Ahmad F, Suri A, Kale SS, Sharma BS, Mahapatra AK, et al. Post operative pituitary apoplexy: preoperative considerations toward preventing nightmare. Br J Neurosurg. 26:59–63. 2012.
Article11. Lee EJ, Ahn JY, Noh T, Kim SH, Kim TS, Kim SH. Tumor tissue identification in the pseudocapsule of pituitary adenoma: should the pseudocapsule be removed for total resection of pituitary adenoma? Neurosurgery. 64(3 Suppl):ONS62–ONS69. 2009.12. Moon JH, Kim EH, Kim SH. Snare technique for the remodeling of the redundant arachnoid pouch to prevent cerebrospinal fluid rhinorrhea and hematoma collection during transsphenoidal surgery for suprasellar-extended pituitary tumors. J Neurosurg. 125:1443–1450. 2016.
Article13. Nakane T, Kuwayama A, Watanabe M, Kageyama N. Transsphenoidal approach to pituitary adenomas with suprasellar extension. Surg Neurol. 16:225–229. 1981.
Article14. Zhang X, Fei Z, Zhang J, Fu L, Zhang Z, Liu W, et al. Management of nonfunctioning pituitary adenomas with suprasellar extensions by transsphenoidal microsurgery. Surg Neurol. 52:380–385. 1999.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Large Intracranial Aneurysm after Transsphenoidal Surgery for Pituitary Macroadenoma
- Clinical Analysis of Endoscopic Transnasal Transsphenoidal Hypophysectomy of Pituitary Tumor
- Pituitary Apoplexy due to Pituitary Adenoma Infarction
- Surgical treatment of a ruptured internal carotid artery pseudoaneurysm following transsphenoidal surgery
- Transsphenoidal Supradiaphragmatic Intradural Approach - Technical Note -