J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):380-385. 10.7461/jcen.2022.E2021.10.004.
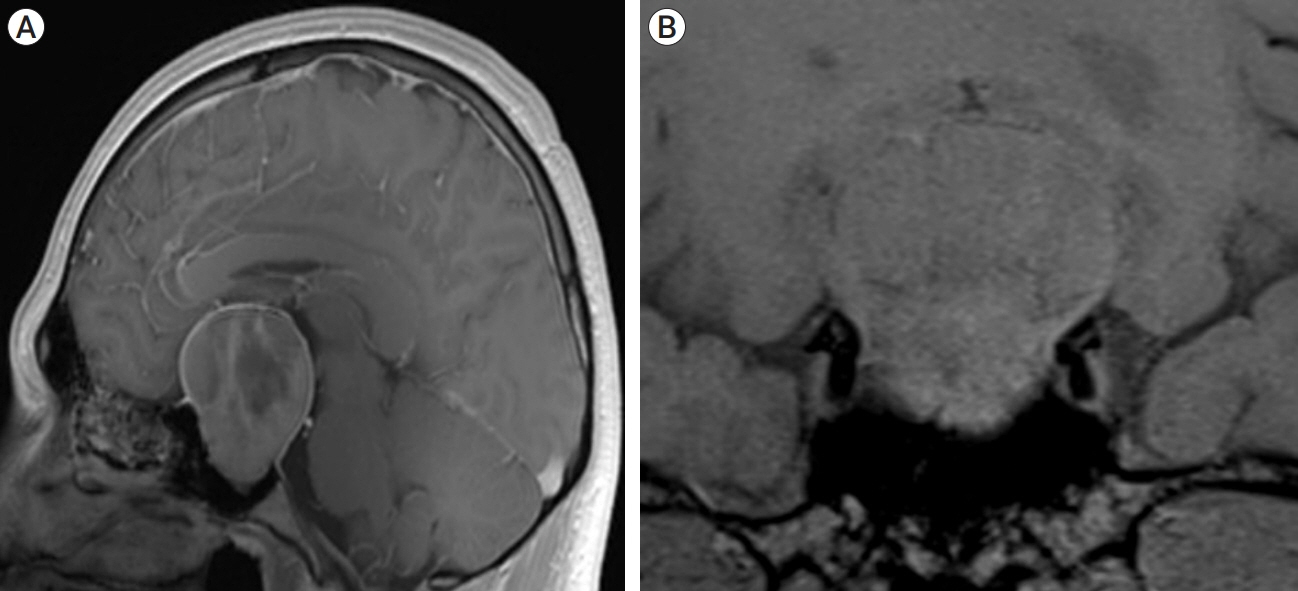
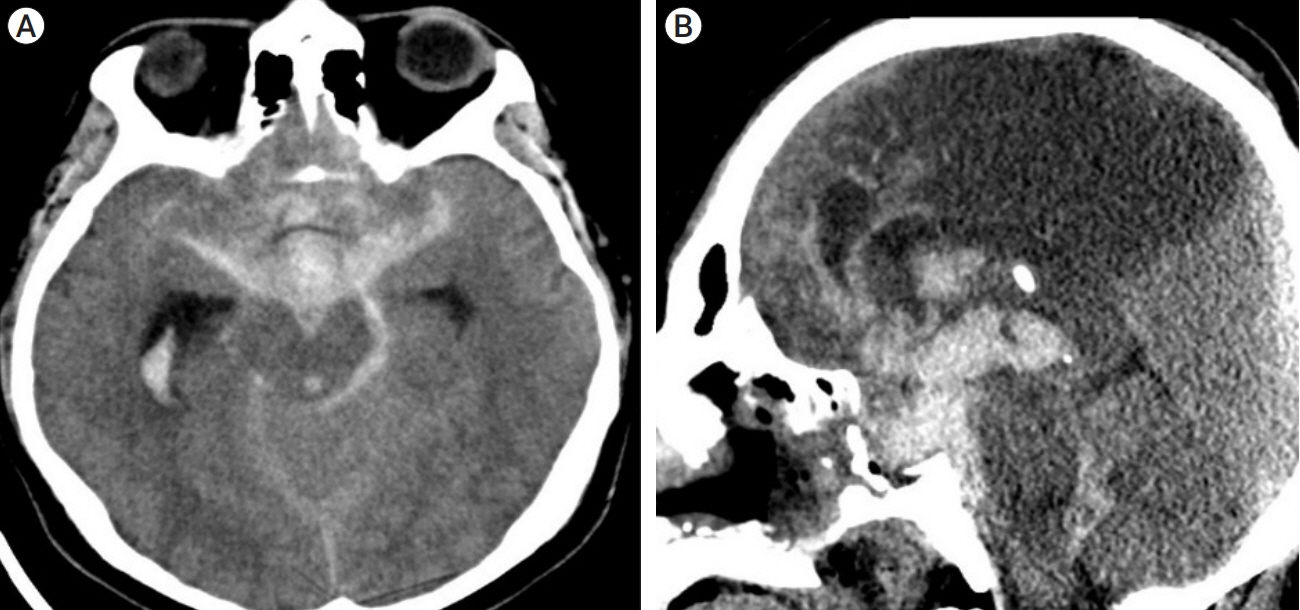
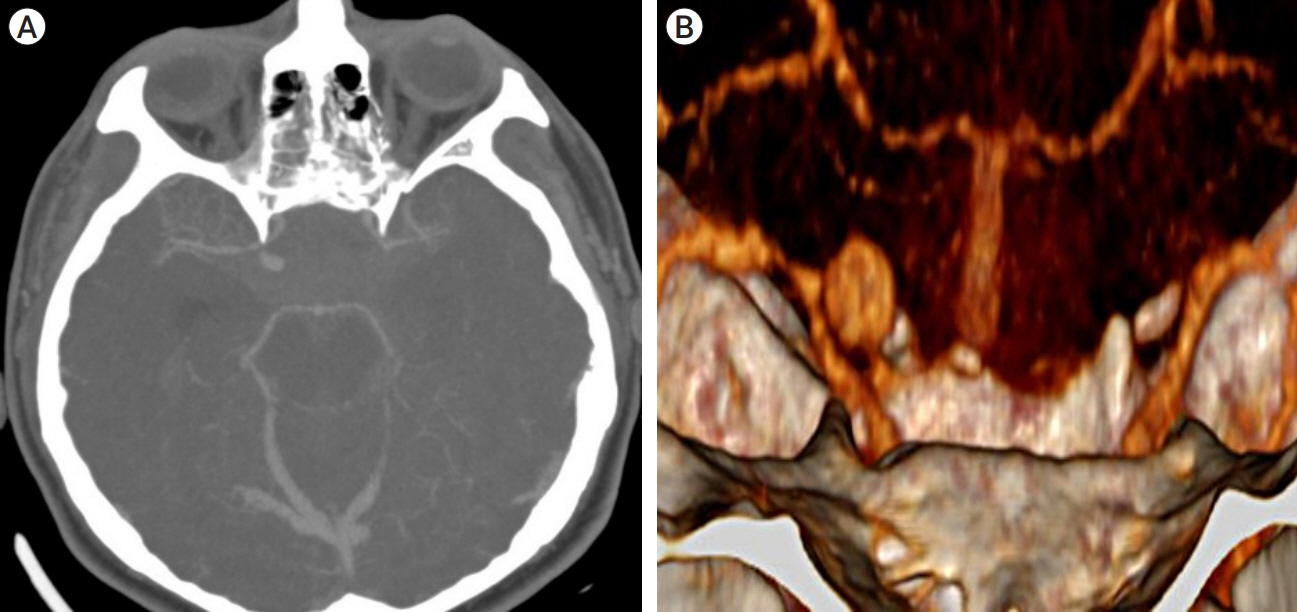
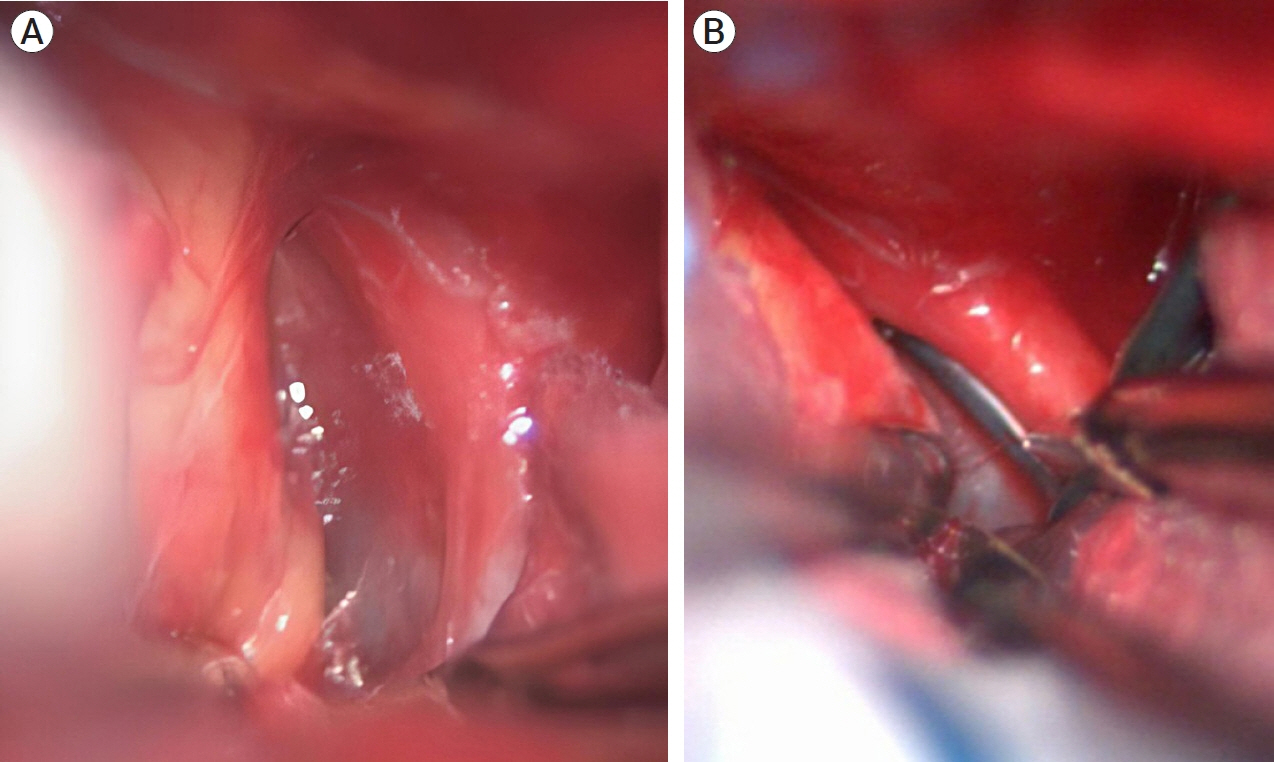
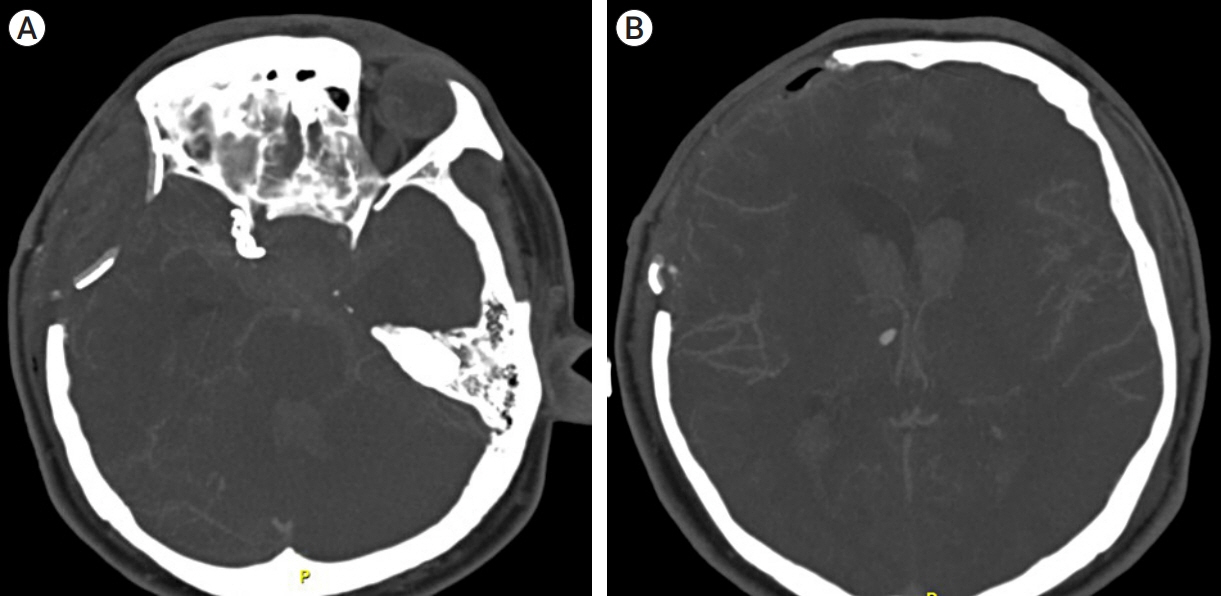
Surgical treatment of a ruptured internal carotid artery pseudoaneurysm following transsphenoidal surgery
- Affiliations
-
- 1Specialties Hospital, 21st Century National Medical Center, Mexico City, Mexico
- KMID: 2537323
- DOI: http://doi.org/10.7461/jcen.2022.E2021.10.004
Abstract
- Development of Internal Carotid Artery pseudoaneurysms (ICAp) after transsphenoidal surgery is extremely rare, occurring only in 0.4% of cases. Surgical treatment of ICAp poses a real challenge to the neurosurgeon as treatment may require parent vessel sacrifice or artery reconstruction with bypass grafting. Furthermore, surgical resolution of these lesions is rarely reported in the literature. The internal carotid artery is prone to iatrogenic injury in transsphenoidal surgery due to its frequent involvement in pituitary adenomas. Intracranial pseudoaneurysms may be at high risk for rupture and increased morbidity and mortality. Here we present a case of a patient with an ICAp rupture two months after transsphenoidal surgery for a pituitary adenoma.
Figure
Reference
-
1. Alzhrani G, Sivakumar W, Park MS, Taussky P, Couldwell WT. Delayed complications after transsphenoidal surgery for pituitary adenomas. World Neurosurg. 2018; Jan. 109:233–41.
Article2. Amenta PS, Starke RM, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH. Successful treatment of a traumatic carotid pseudoaneurysm with the Pipeline stent: case report and review of the literature. Surg Neurol Int. 2012; 3:160.
Article3. Andrade-Barazarte H, Luostarinen T, Goehre F, Kivelev J, Jahromi BR, Ludtka C, et al. Transient cardiac arrest induced by adenosine: a tool for contralateral clipping of internal carotid artery-ophtalmic segment aneurysms. World Neurosurg. 2015; Dec. 84(6):1933–40.4. Bulsara KR, Karavadia SS, Powers CJ, Paullus WC. Association between pituitary adenomas and intracranial aneurysms: an illustrative case and review of the literature. Neurol India. 2007; Oct-Dec. 55(4):410–2.
Article5. Burton C, Velasco F, Dorman J. Traumatic aneurysm of a peripheral cerebral artery. Review and case report. J Neurosurg. 1968; May. 28(5):468–74.6. Ciceri EFM, Regna-Gladin C, Erbetta A, Chiapparini L, Nappini S, Savoiardo M, et al. Iatrogenic intracranial pseudoaneurysms: neuroradiological and therapeutical considerations, including endovascular options. Neurol Sci. 2006; Nov. 27(5):317–22.
Article7. Goyal N, Basheer N, Suri A, Mahapatra AK. Subarachnoid hemorrhage after transsphenoidal surgery for pituitary adenoma: a case report and review of literature. Neurol India. May-Jun. 2012; 60(3):337–8.8. Karadag A, Kinali B, Ugur O, Oran I, Middlebrooks EH, Senoglu M. A case of pseudoaneurysm of the internal carotid artery following endoscopic endonasal pituitary surgery: endovascular treatment with flow-diverting stent implantation. Acta Medica (Hradec Kralove). 2017; 60(2):89–92.
Article9. Laws ER Jr. Vascular complications of transsphenoidal surgery. Pituitary. 1999; Aug. 2(2):163–70.10. Medel R, Crowley RW, Hamilton DK, Dumont AS. Endovascular obliteration of an intracranial pseudoaneurysm: the utility of Onyx. J Neurosurg Pediatr. 2009; Nov. 4(5):445–8.11. Nariai Y, Kawamura Y, Takigawa T, Hyodo A, Suzuki K. Pipeline embolization for an iatrogenic intracranial internal carotid artery pseudoaneurysm after transsphenoidal pituitary tumor surgery: case report and review of the literature. Interv Neuroradiol. 2020; Feb. 26(1):74–82.
Article12. Nerva JD, Morton RP, Levitt MR, Osbun JW, Ferreira MJ, Ghodke BV, et al. Pipeline embolization device as primary treatment for blister aneurysms and iatrogenic pseudoaneurysms of the internal carotid artery. J Neurointerv Surg. 2015; Mar. 7(3):210–6.
Article13. Raymond J, Hardy J, Czepko R, Roy D. Arterial injuries in transsphenoidal surgery for pituitary adenoma; the role of angiography and endovascular treatment. AJNR Am J Neuroradiol. 1997; Apr. 18(4):655–65.14. Wilson CB, Dempsey LC. Transsphenoidal microsurgical removal of 250 pituitary adenomas. J Neurosurg. 1978; Jan. 48(1):13–22.
Article15. Zhang Y, Tian Z, Li C, Liu J, Zhang Y, Yang X, et al. A modified endovascular treatment protocol for iatrogenic internal carotid artery injuries following endoscopic endonasal surgery. J Neurosurg. 2019; Jan. 25. 132(2):343–50.
Article16. Zheng Y, Lu Z, Shen J, Xu F. Intracranial pseudoaneurysms: evaluation and management. Front Neurol. 2020; Jul. 11:582.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Internal Carotid Artery Pseudoaneurysm 10 Years after Cervical Spine Surgery
- Technical Pitfalls in the Endovascular Treatment of Traumatic Pseudoaneurysm of the Internal Carotid Artery: Case Report
- Traumatic Pseudoaneurysm of the External and Internal Carotid Artery Presenting as Epistaxis: Case Report
- Surgical Experience of Carotid Pseudoaneurysm
- Pseudoaneurysm of the Petrosal Internal Carotid Artery in the Middle Ear as a Complication of Middle Ear Cholesteatoma