J Korean Neurosurg Soc.
2022 Jul;65(4):507-513. 10.3340/jkns.2021.0195.
The Relationship between Parkinson’s Disease and Acute Myocardial Infarction in Korea : A Nationwide Longitudinal Cohort Study
- Affiliations
-
- 1Department of Neurosurgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 2Department of Neurosurgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Genome & Health Big Data Branch, Department of Public Health, Graduate School of Public Health, Seoul National University, Seoul, Korea
- 4Cornell University, Ithaca, NY, USA
- KMID: 2531619
- DOI: http://doi.org/10.3340/jkns.2021.0195
Abstract
Objective
: The goal of the following statewide age and gender-coordinated cohort study in Korea is to find out if there is a link between acute myocardial infarction (AMI) and Parkinson’s disease (PD).
Methods
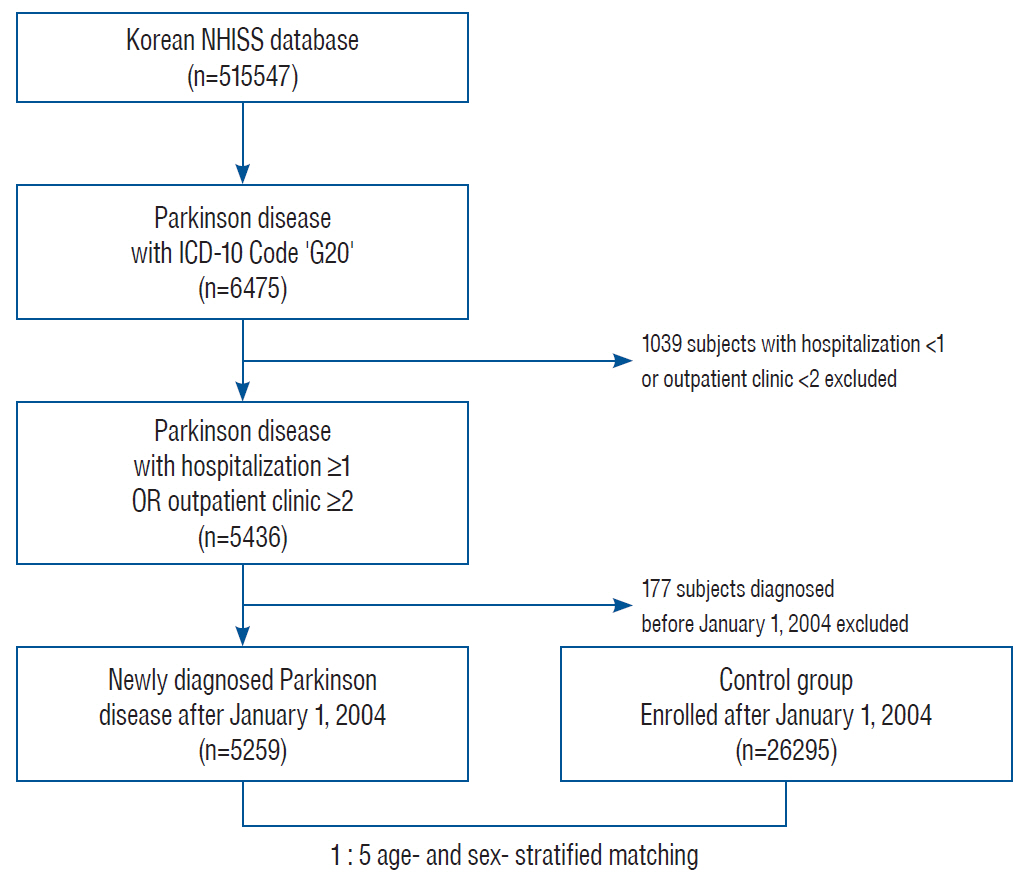
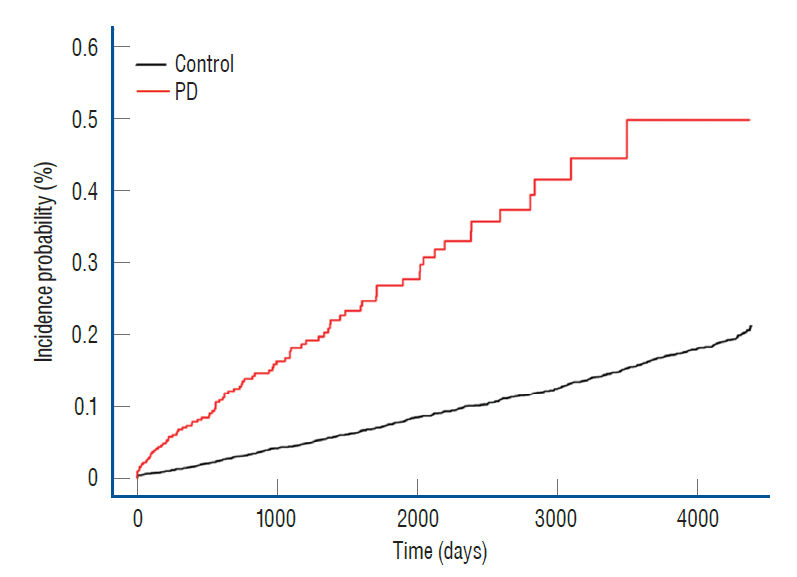
: Utilizing the National Health Insurance Sharing Service cohort, patient data were collected. Six thousand four hundred seventy-five individuals with PD were distinguished by utilizing the International Classification of Diseases 10 code G20 and have enrolled in the PD group. The number of participants decreased to 5259 after excluding 1039 patients who were hospitalized less than one time or who visited an outpatient clinic less than twice. Then, 26295 individuals were selected as part of the control group after case control matching was conducted through 1 : 5 age- and gender-coordinated matching. The Cox proportional hazard regression analysis and Kaplan-Meier method were utilized to analyze the likelihood of AMI in PD.
Results
: After controlling for age and gender, the hazard ratio of AMI in the PD group was 3.603 (95% confidence interval [CI], 2.837–4.577). After that, the following hazard ratio of AMI in the PD group was modified against for co-morbid medical disorders, resulting in 3.551 (95% CI, 2.795–4.511). According to a subgroup analysis, in males and females aged <65 and aged ≥65 and in the non-diabetes and diabetes, hypertension and non-hypertension, dyslipidemia and non-dyslipidemia subgroups, the AMI incidence rates were dramatically higher in the PD group compared to that of the control.
Conclusion
: Individuals with PD have a greater chance of AMI, according to this cross-national study.
Figure
Cited by 1 articles
-
Editor’s Pick in July 2023
Bum-Tae Kim
J Korean Neurosurg Soc. 2023;66(4):341-343. doi: 10.3340/jkns.2023.0117.
Reference
-
References
1. Bae KH, Hong JB, Choi YJ, Jung JH, Han IB, Choi JM, et al. Association of congestive heart failure and death with ankylosing spondylitis : a nationwide longitudinal cohort study in Korea. J Korean Neurosurg Soc. 62:217–224. 2019.
Article2. Beyer MK, Herlofson K, Arsland D, Larsen JP. Causes of death in a community-based study of Parkinson’s disease. Acta Neurol Scand. 103:7–11. 2001.
Article3. Cereda E, Barichella M, Pedrolli C, Klersy C, Cassani E, Caccialanza R, et al. Diabetes and risk of Parkinson’s disease: a systematic review and meta-analysis. Diabetes Care. 34:2614–2623. 2011.4. de Lau LM, Breteler MM. Epidemiology of Parkinson’s disease. Lancet Neurol. 5:525–535. 2006.
Article5. Fahdi IE, Gaddam V, Garza L, Romeo F, Mehta JL. Inflammation, infection, and atherosclerosis. Brain Behav Immun. 17:238–244. 2003.
Article6. Fedorowski A, Stavenow L, Hedblad B, Berglund G, Nilsson PM, Melander O. Orthostatic hypotension predicts all-cause mortality and coronary events in middle-aged individuals (the Malmo preventive project). Eur Heart J. 31:85–91. 2010.
Article7. Gołab-Janowska M, Budzianowska A, Honczarenko K. Autonomic disorders in Parkinson’s disease. Ann Acad Med Stetin. 57:11–15. discussion 16. 2011.8. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 352:1685–1695. 2005.
Article9. Harrison D, Griendling KK, Landmesser U, Hornig B, Drexler H. Role of oxidative stress in atherosclerosis. Am J Cardiol. 91(3A):7A–11A. 2003.
Article10. Heitzer T, Schlinzig T, Krohn K, Meinertz T, Münzel T. Endothelial dysfunction, oxidative stress, and risk of cardiovascular events in patients with coronary artery disease. Circulation. 104:2673–2678. 2001.
Article11. Jain S, Goldstein DS. Cardiovascular dysautonomia in Parkinson disease: from pathophysiology to pathogenesis. Neurobiol Dis. 46:572–580. 2012.
Article12. Jenner P. Oxidative stress in Parkinson’s disease. Ann Neurol. 53 Suppl 3:S26–S36. discussion S36-S38. 2003.13. Kang SH, Choi EK, Han KD, Lee SR, Lim WH, Cha MJ, et al. Underweight is a risk factor for atrial fibrillation: a nationwide populationbased study. Int J Cardiol. 215:449–456. 2016.
Article14. Kim YS, Kim JG, Yi J, Choi JM, Chung CK, Choi UY, et al. Changes in the medical burden of pyogenic and tuberculous spondylitis between 2007 and 2016: a nationwide cohort study. J Clin Neurosci. 73:89–93. 2020.
Article15. Lee DH, Choi YJ, Han IB, Hong JB, Do Han K, Choi JM, et al. Association of ischemic stroke with ankylosing spondylitis: a nationwide longitudinal cohort study. Acta Neurochir (Wien). 160:949–955. 2018.
Article16. Lee JK, Kim H, Hong JB, Sheen SH, Han IB, Sohn S. Association of acute myocardial infarction with seropositive rheumatoid arthritis in Korea: a nationwide longitudinal cohort study. J Clin Neurosci. 78:97–101. 2020.
Article17. Liang HW, Huang YP, Pan SL. Parkinson disease and risk of acute myocardial infarction: a population-based, propensity score-matched, longitudinal follow-up study. Am Heart J. 169:508–514. 2015.
Article18. Libby P, Ridker PM, Maseri A. Inflammation and atherosclerosis. Circulation. 105:1135–1143. 2002.
Article19. Lim SY, Lang AE. The nonmotor symptoms of Parkinson’s disease--an overview. Mov Disord. 25 Suppl 1:S123–S130. 2010.
Article20. Luukinen H, Koski K, Laippala P, Airaksinen KE. Orthostatic hypotension and the risk of myocardial infarction in the home-dwelling elderly. J Intern Med. 255:486–493. 2004.
Article21. Madamanchi NR, Vendrov A, Runge MS. Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol. 25:29–38. 2005.
Article22. Mehta JL, Saldeen TG, Rand K. Interactive role of infection, inflammation and traditional risk factors in atherosclerosis and coronary artery disease. J Am Coll Cardiol. 31:1217–1225. 1998.
Article23. Park CJ, Choi YJ, Kim JG, Han IB, Do Han K, Choi JM, et al. Association of acute myocardial infarction with ankylosing spondylitis: a nationwide longitudinal cohort study. J Clin Neurosci. 56:34–37. 2018.
Article24. Park CS, Choi EK, Han KD, Lee HJ, Rhee TM, Lee SR, et al. Association between adult height, myocardial infarction, heart failure, stroke and death: a Korean nationwide population-based study. Int J Epidemiol. 47:289–298. 2018.
Article25. Pennington S, Snell K, Lee M, Walker R. The cause of death in idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 16:434–437. 2010.
Article26. Qiu C, Hu G, Kivipelto M, Laatikainen T, Antikainen R, Fratiglioni L, et al. Association of blood pressure and hypertension with the risk of Parkinson disease: the national FINRISK study. Hypertension. 57:1094–1100. 2011.
Article27. Rektor I, Goldemund D, Sheardová K, Rektorová I, Michálková Z, Dufek M. Vascular pathology in patients with idiopathic Parkinson’s disease. Parkinsonism Relat Disord. 15:24–29. 2009.
Article28. Roos RA, Jongen JC, van der Velde EA. Clinical course of patients with idiopathic Parkinson’s disease. Mov Disord. 11:236–242. 1996.
Article29. Rose KM, Tyroler HA, Nardo CJ, Arnett DK, Light KC, Rosamond W, et al. Orthostatic hypotension and the incidence of coronary heart disease: the Atherosclerosis Risk in Communities study. Am J Hypertens. 13(6 Pt 1):571–578. 2000.
Article30. Ross R. Atherosclerosis--an inflammatory disease. N Engl J Med. 340:115–126. 1999.31. Senard JM, Raï S, Lapeyre-Mestre M, Brefel C, Rascol O, Rascol A, et al. Prevalence of orthostatic hypotension in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 63:584–589. 1997.
Article32. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 7:e016640. 2017.
Article33. Simanek AM, Dowd JB, Pawelec G, Melzer D, Dutta A, Aiello AE. Seropositivity to cytomegalovirus, inflammation, all-cause and cardiovascular disease-related mortality in the United States. PLoS One. 6:e16103. 2011.
Article34. Sun Y, Chang YH, Chen HF, Su YH, Su HF, Li CY. Risk of Parkinson disease onset in patients with diabetes: a 9-year population-based cohort study with age and sex stratifications. Diabetes Care. 35:1047–1049. 2012.35. Velseboer DC, de Haan RJ, Wieling W, Goldstein DS, de Bie RM. Prevalence of orthostatic hypotension in Parkinson’s disease: a systematic review and meta-analysis. Parkinsonism Relat Disord. 17:724–729. 2011.
Article36. Verwoert GC, Mattace-Raso FU, Hofman A, Heeringa J, Stricker BH, Breteler MM, et al. Orthostatic hypotension and risk of cardiovascular disease in elderly people: the Rotterdam study. J Am Geriatr Soc. 56:1816–1820. 2008.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Association of Acute Myocardial Infarction with Ossification of the Posterior Longitudinal Ligament in Korea: A Nationwide Longitudinal Cohort Study
- Invasive Treatment of Acute Myocardial Infarction: What is the Optimal Therapy for Acute Myocardial Infarction?
- The Association of Acute Myocardial Infarction with Pyogenic Spondylitis in Korea: A Nationwide Longitudinal Cohort Study
- Myocardial Longitudinal Strain in Prediction of Heart Failure after Acute Myocardial Infarction
- Differences in Clinical Outcomes Between Patients With ST-Elevation Versus Non-ST-Elevation Acute Myocardial Infarction in Korea