Korean J Pain.
2022 Jul;35(3):250-260. 10.3344/kjp.2022.35.3.250.
Identification of cranial nerve ganglia using sectioned images and three-dimensional models of a cadaver
- Affiliations
-
- 1Department of Anatomy, Dongguk University School of Medicine, Gyeongju, Korea
- 2Department of Anatomy, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2530980
- DOI: http://doi.org/10.3344/kjp.2022.35.3.250
Abstract
- Background
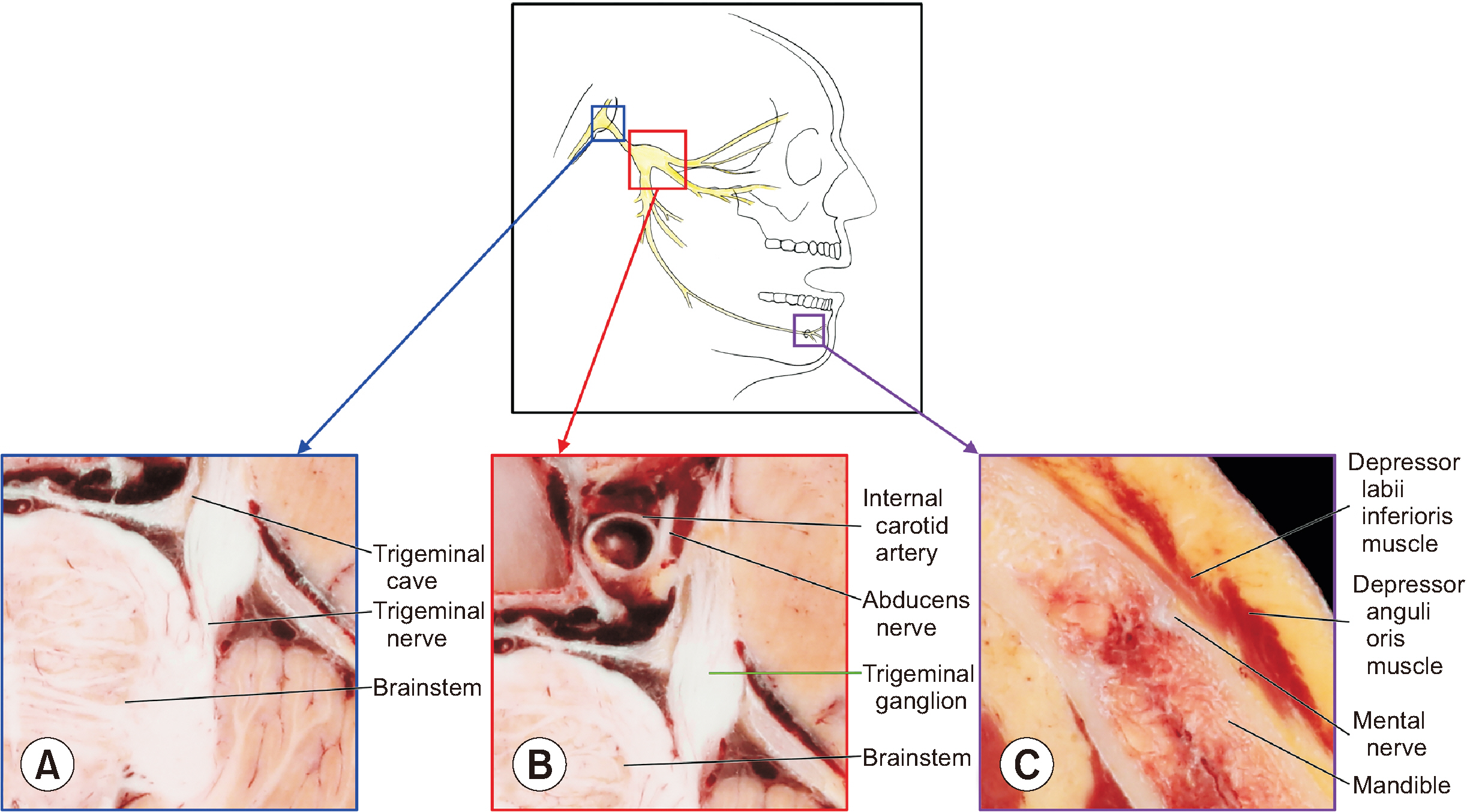
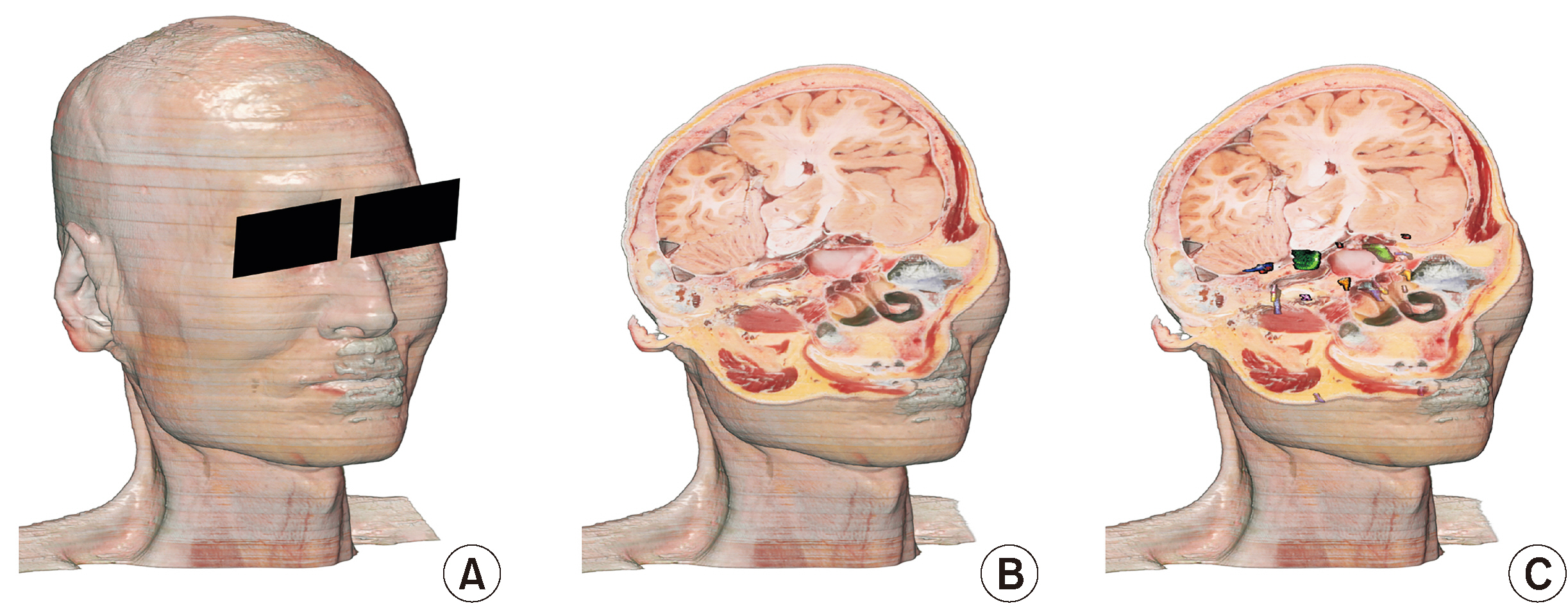
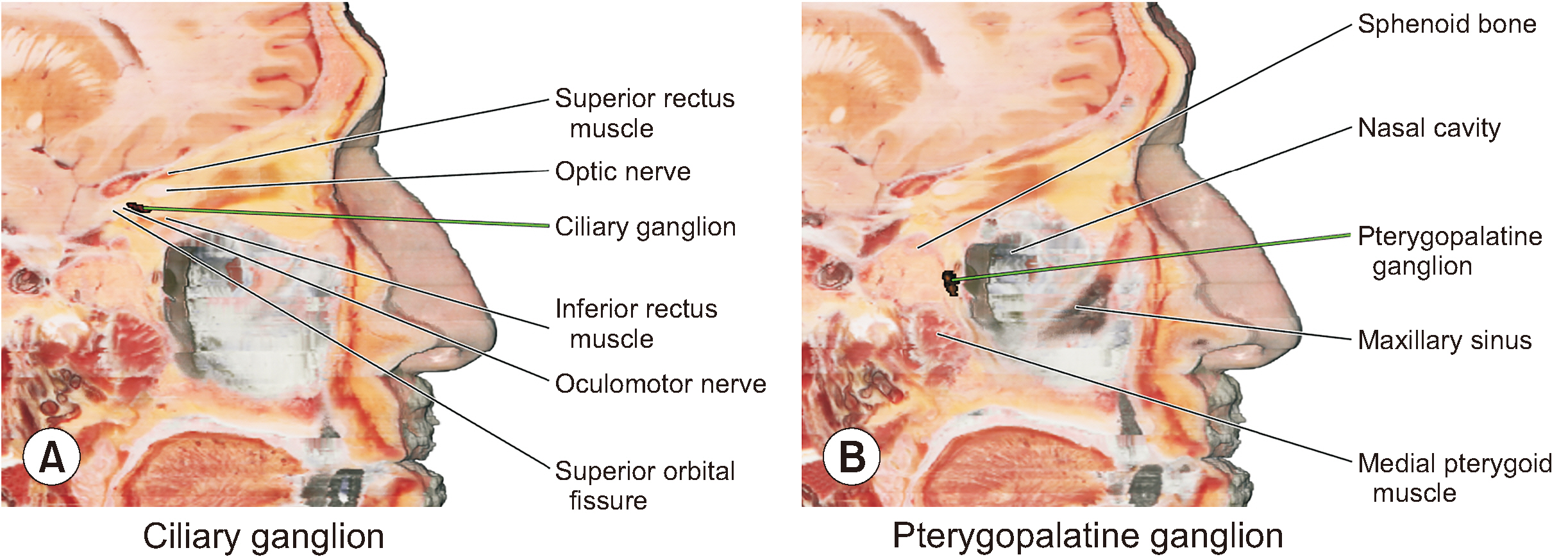
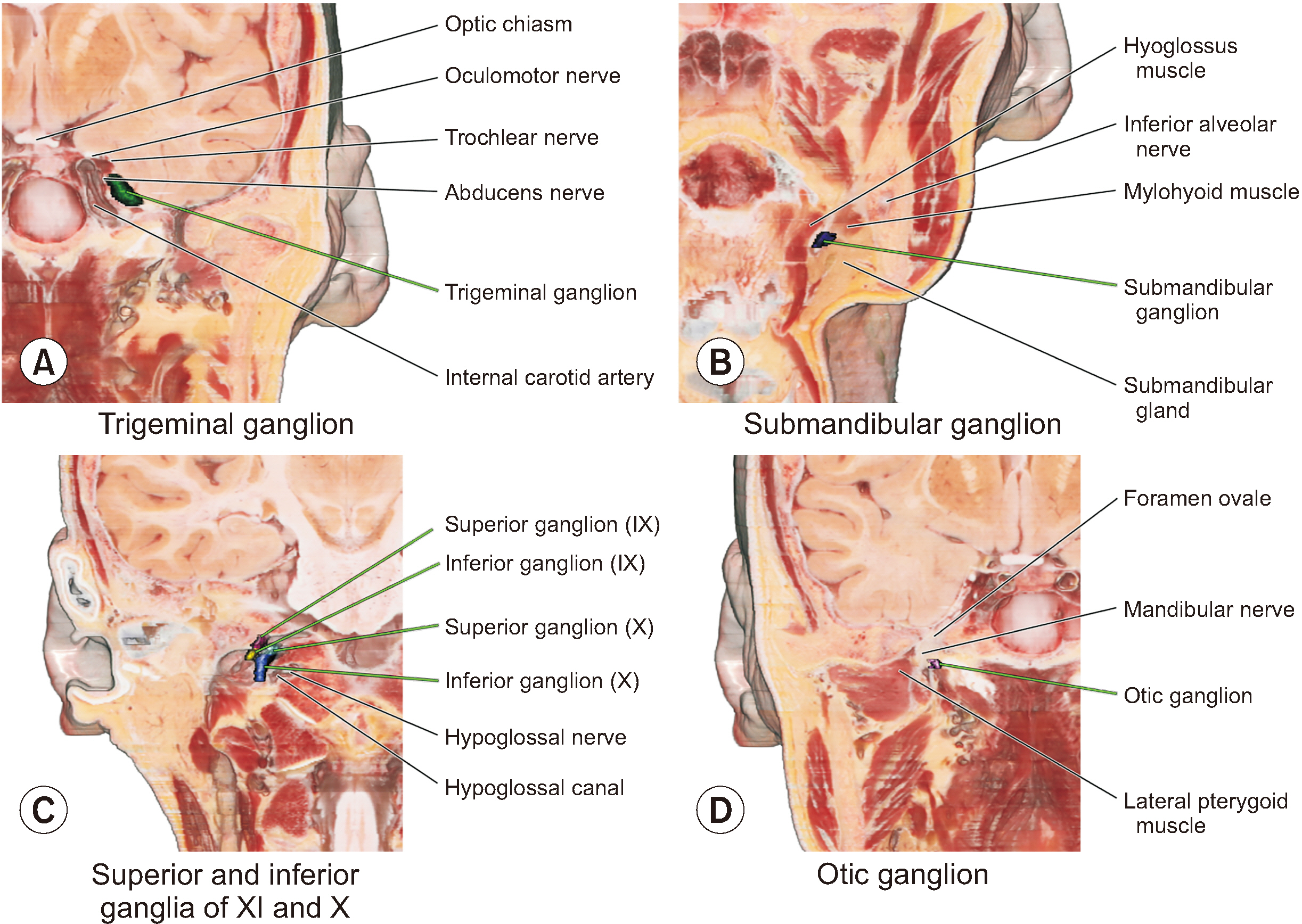
Cranial nerve ganglia, which are prone to viral infections and tumors, are located deep in the head, so their detailed anatomy is difficult to understand using conventional cadaver dissection. For locating the small ganglia in medical images, their sectional anatomy should be learned by medical students and doctors. The purpose of this study is to elucidate cranial ganglia anatomy using sectioned images and three-dimensional (3D) models of a cadaver.
Methods
One thousand two hundred and forty-six sectioned images of a male cadaver were examined to identify the cranial nerve ganglia. Using the real color sectioned images, real color volume model having a voxel size of 0.4 × 0.4 × 0.4 mm was produced.
Results
The sectioned images and 3D models can be downloaded for free from a webpage, anatomy.dongguk.ac.kr/ganglia. On the images and model, all the cranial nerve ganglia and their whole course were identified. In case of the facial nerve, the geniculate, pterygopalatine, and submandibular ganglia were clearly identified. In case of the glossopharyngeal nerve, the superior, inferior, and otic ganglia were found. Thanks to the high resolution and real color of the sectioned images and volume models, detailed observation of the ganglia was possible. Since the volume models can be cut both in orthogonal planes and oblique planes, advanced sectional anatomy of the ganglia can be explained concretely.
Conclusions
The sectioned images and 3D models will be helpful resources for understanding cranial nerve ganglia anatomy, for performing related surgical procedures.
Keyword
Figure
Reference
-
1. Saremi F, Helmy M, Farzin S, Zee CS, Go JL. 2005; MRI of cranial nerve enhancement. AJR Am J Roentgenol. 185:1487–97. DOI: 10.2214/AJR.04.1518. PMID: 16304002.
Article2. VandeVyver V, Lemmerling M, Van Hecke W, Verstraete K. 2007; MRI findings of the normal and diseased trigeminal nerve ganglion and branches: a pictorial review. JBR-BTR. 90:272–7. DOI: 10.1016/j.clinimag.2008.01.005. PMID: 17966244.
Article3. Khonsary SA, Ma Q, Villablanca P, Emerson J, Malkasian D. 2013; Clinical functional anatomy of the pterygopalatine ganglion, cephalgia and related dysautonomias: a review. Surg Neurol Int. 4(Suppl 6):S422–8. DOI: 10.4103/2152-7806.121628. PMID: 24349865. PMCID: PMC3858801.
Article4. An JX, Liu H, Chen RW, Wang Y, Zhao WX, Eastwood D, et al. 2018; Computed tomography-guided percutaneous ozone injection of the Gasserian ganglion for the treatment of trigeminal neuralgia. J Pain Res. 11:255–63. DOI: 10.2147/JPR.S140369. PMID: 29430195. PMCID: PMC5797463.
Article5. Rusu MC, Pop F, Curcă GC, Podoleanu L, Voinea LM. 2009; The pterygopalatine ganglion in humans: a morphological study. Ann Anat. 191:196–202. DOI: 10.1016/j.aanat.2008.09.008. PMID: 19124232.
Article6. Senger M, Stoffels HJ, Angelov DN. 2014; Topography, syntopy and morphology of the human otic ganglion: a cadaver study. Ann Anat. 196:327–35. DOI: 10.1016/j.aanat.2014.05.039. PMID: 24973995.
Article7. Bratbak DF, Folvik M, Nordgård S, Stovner LJ, Dodick DW, Matharu M, et al. 2018; Depicting the pterygopalatine ganglion on 3 Tesla magnetic resonance images. Surg Radiol Anat. 40:689–95. DOI: 10.1007/s00276-017-1960-6. PMID: 29274037.
Article8. Kim CY, Jung YW, Park JS. 2021; The Visible Korean: movable surface models of the hip joint. Surg Radiol Anat. 43:559–66. DOI: 10.1007/s00276-021-02697-7. PMID: 33550473.
Article9. Chung BS, Park JS. 2019; Real-color volume models made from real-color sectioned images of Visible Korean. J Korean Med Sci. 34:e86. DOI: 10.3346/jkms.2019.34.e86. PMID: 30886552. PMCID: PMC6417999.
Article10. You Y, Kim CY, Kim SK, Chung BS, Har D, Choi J, et al. 2022; Advanced-sectioned images obtained by microsectioning of the entire male body. Clin Anat. 35:79–86. DOI: 10.1002/ca.23795. PMID: 34591338.
Article11. Park JS, Chung MS, Hwang SB, Lee YS, Har DH, Park HS. 2005; Visible Korean human: improved serially sectioned images of the entire body. IEEE Trans Med Imaging. 24:352–60. DOI: 10.1109/TMI.2004.842454. PMID: 15754985.
Article12. Tesapirat L, Jariyakosol S, Chentanez V. 2020; Morphometric study of the ciliary ganglion and its pertinent intraorbital procedure. Folia Morphol (Warsz). 79:438–44. DOI: 10.5603/FM.a2019.0112. PMID: 31621056.
Article13. Moore KL, Dalley AF 2nd, Agur AM. 2018. Clinically oriented anatomy. 8th ed. Lippincott Williams & Wilkins;Philadelphia: p. 1956–7. https://www.worldcat.org/title/clinically-oriented-anatomy/oclc/1113102860?referer=br&ht=edition. DOI: 10.5603/fm.a2019.0112.14. Hamzaoğlu V, Beger O, Erdoğan O, Kara E, Vayisoğlu Y, Taghipour P, et al. 2020; Radioanatomic assessment of the geniculate ganglion dehiscence and dimension: a cadaveric study. World Neurosurg. 134:e913–9. DOI: 10.1016/j.wneu.2019.11.036. PMID: 31733393.
Article15. Piagkou M, Demesticha T, Troupis T, Vlasis K, Skandalakis P, Makri A, et al. 2012; The pterygopalatine ganglion and its role in various pain syndromes: from anatomy to clinical practice. Pain Pract. 12:399–412. Erratum in: Pain Pract 2012; 12: 673. DOI: 10.1111/j.1533-2500.2011.00507.x. PMID: 21956040.
Article16. Spock T, Hoffman HT, Joshi AS. 2015; Transoral submandibular ganglion neurectomy: an anatomical feasibility study. Ann Otol Rhinol Laryngol. 124:341–4. DOI: 10.1177/0003489414557019. PMID: 25429100.17. Zhang L, Chen S, Sun Y. 2022; Mechanism and prevention of spiral ganglion neuron degeneration in the cochlea. Front Cell Neurosci. 15:814891. DOI: 10.3389/fncel.2021.814891. PMID: 35069120. PMCID: PMC8766678. PMID: 950ed78c05fd41058c9f040e54bee32f.
Article18. Guillotte A, Zand A, Ortiz M, Gan Y, Rivera A, Litofsky NS, et al. 2020; Clinical outcomes of resecting scarpa's ganglion during vestibular schwannoma surgery. J Clin Neurosci. 76:114–7. DOI: 10.1016/j.jocn.2020.04.029. PMID: 32284286.
Article19. Franzini A, Messina G, Franzini A, Marchetti M, Ferroli P, Fariselli L, et al. 2017; Treatments of glossopharyngeal neuralgia: towards standard procedures. Neurol Sci. 38(Suppl 1):51–5. DOI: 10.1007/s10072-017-2909-6. PMID: 28527060.
Article20. de Bree R, van der Waal I, Leemans CR. 2007; Management of Frey syndrome. Head Neck. 29:773–8. DOI: 10.1002/hed.20568. PMID: 17230557.
Article21. Crespi J, Bratbak D, Dodick DW, Matharu MS, Senger M, Angelov DN, et al. 2019; Anatomical landmarks for localizing the otic ganglion: a possible new treatment target for headache disorders. Cephalalgia Rep. doi: 10.1177/2515816319850761. DOI: 10.1177/2515816319850761. PMID: f5851fc367f84c5b8cac3c53c81c4e9b.
Article22. Crespi J, Bratbak D, Dodick DW, Matharu M, Solheim O, Gulati S, et al. 2020; Open-label, multi-dose, pilot safety study of injection of onabotulinumtoxinA toward the otic ganglion for the treatment of intractable chronic cluster headache. Headache. 60:1632–43. DOI: 10.1111/head.13889. PMID: 32583902.
Article23. Miller RB, Boon MS, Atkins JP, Lowry LD. 2000; Vagal paraganglioma: the Jefferson experience. Otolaryngol Head Neck Surg. 122:482–7. DOI: 10.1067/mhn.2000.102807. PMID: 10740165.
Article24. Park JS, Chung MS, Hwang SB, Lee YS, Har DH. 2005; Technical report on semiautomatic segmentation using the Adobe Photoshop. J Digit Imaging. 18:333–43. DOI: 10.1007/s10278-005-6704-1. PMID: 16003588. PMCID: PMC3046725.
Article25. Archie KA, Marcus DS. 2012; DicomBrowser: software for viewing and modifying DICOM metadata. J Digit Imaging. 25:635–45. DOI: 10.1007/s10278-012-9462-x. PMID: 22349992. PMCID: PMC3447088.
Article26. Li X, Morgan PS, Ashburner J, Smith J, Rorden C. 2016; The first step for neuroimaging data analysis: DICOM to NIfTI conversion. J Neurosci Methods. 264:47–56. DOI: 10.1016/j.jneumeth.2016.03.001. PMID: 26945974.
Article27. Sinnreich Z, Nathan H. 1981; The ciliary ganglion in man (anatomical observations). Anat Anz. 150:287–97. PMID: 7305005.28. Tubbs RS, Mortazavi MM, Krishnamurthy S, Verma K, Griessenauer CJ, Cohen-Gadol AA. 2013; The relationship between the superior petrosal sinus and the porus trigeminus: an anatomical study. J Neurosurg. 119:1221–5. DOI: 10.3171/2013.4.JNS122062. PMID: 23706047.
Article29. Lan MY, Shiao JY. 2010; Using greater superficial petrosal nerve and geniculate ganglion as the only two landmarks for identifying internal auditory canal in middle fossa approach. Eur Arch Otorhinolaryngol. 267:1867–71. DOI: 10.1007/s00405-010-1328-6. PMID: 20614126.
Article30. Rong Z, Zixiang Y, Chang L, Guoxing X, Sheng Z, Yuanteng X, et al. 2008; Lacrimal hyposecretion: a surgical complication of juvenile nasopharyngeal angiofibroma. Am J Otolaryngol. 29:367–71. DOI: 10.1016/j.amjoto.2007.10.006. PMID: 19144296.
Article31. Siéssere S, Vitti M, Sousa LG, Semprini M, Iyomasa MM, Regalo SC. 2008; Anatomic variation of cranial parasympathetic ganglia. Braz Oral Res. 22:101–5. DOI: 10.1590/S1806-83242008000200002. PMID: 18622477.
Article32. Mei X, Glueckert R, Schrott-Fischer A, Li H, Ladak HM, Agrawal SK, et al. 2020; Vascular supply of the human spiral ganglion: novel three-dimensional analysis using synchrotron phase-contrast imaging and histology. Sci Rep. 10:5877. Erratum in: Sci Rep 2020; 10: 7681. DOI: 10.1038/s41598-020-62653-0. PMID: 32245997. PMCID: PMC7125215.
Article33. Wu YW, Karandikar A, Goh JP, Tan TY. 2020; Imaging features differentiating vestibular ganglion from intracanalicular schwannoma on single-sequence non-contrast magnetic resonance imaging study. Ann Acad Med Singap. 49:65–71. DOI: 10.47102/annals-acadmedsg.2019156. PMID: 32246707.
Article34. Mancall EL, Brock DG. Mancall EL, Brock DG, editors. 2011. Cervical plexus. Gray’s clinical neuroanatomy: the anatomic basis for clinical neuroscience. Elsevier Health Sciences;Philadelphia: p. 315–7. https://www.worldcat.org/title/grays-clinical-neuroanatomy/oclc/851363117?referer=di&ht=edition.35. Tepper SJ, Caparso A. 2017; Sphenopalatine ganglion (SPG): stimulation mechanism, safety, and efficacy. Headache. 57 Suppl 1:14–28. DOI: 10.1111/head.13035. PMID: 28387016.
Article36. Tolba R, Weiss AL, Denis DJ. 2019; Sphenopalatine ganglion block and radiofrequency ablation: technical notes and efficacy. Ochsner J. 19:32–7. DOI: 10.31486/toj.18.0163. PMID: 30983899. PMCID: PMC6447206.
Article37. Crespi J, Bratbak D, Dodick D, Matharu M, Jamtøy KA, Tronvik E. 2019; Prediction of the sphenopalatine ganglion localization in computerized tomography images. Cephalalgia Rep. doi: 10.1177/2515816318824690. DOI: 10.1177/2515816318824690. PMID: 93c0d46e985f47d49fff983f42cac8ed.
Article38. Song MH, Lee HY, Jeon JS, Lee JD, Lee HK, Lee WS. 2008; Jugular foramen schwannoma: analysis on its origin and location. Otol Neurotol. 29:387–91. DOI: 10.1097/MAO.0b013e318164cb83. PMID: 18277311.39. Roh TH, Oh JW, Jang CK, Choi S, Kim EH, Hong CK, et al. 2021; Virtual dissection of the real brain: integration of photographic 3D models into virtual reality and its effect on neurosurgical resident education. Neurosurg Focus. 51:E16. DOI: 10.3171/2021.5.FOCUS21193. PMID: 34333482.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Manufacture of the Serially Sectioned Images of the Whole Body (First Report: Methods for Embedding and Serial Sectioning)
- Registration of Cadaver's Sectioned Images to Patient's Head MRIs
- Lymph Node Stations of Pancreas Which Are Identified in Real Color Sectioned Images of a Cadaver With Pancreatic Cancer
- Manufacture of the Serially Sectioned Images of the Whole Body (Second Report: Photographing and Processing of the Anatomical Images)
- Three types of the serial segmented images suitable for surface reconstruction