J Stroke.
2022 May;24(2):245-255. 10.5853/jos.2022.01095.
Etiology-Related Outcome of Endovascular Therapy in Posterior Circulation Stroke Compared to Anterior Circulation Stroke
- Affiliations
-
- 1Department of Neurology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Neurology, Uijeongbu Eulji Medical Center, Eulji University School of Medicine, Uijeugbu, Korea
- 4Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2530527
- DOI: http://doi.org/10.5853/jos.2022.01095
Abstract
- Background and Purpose
We investigated the impact of stroke etiology on the endovascular treatment (EVT) procedure and clinical outcome of posterior circulation stroke (PCS) patients with EVT compared to anterior circulation stroke (ACS) patients.
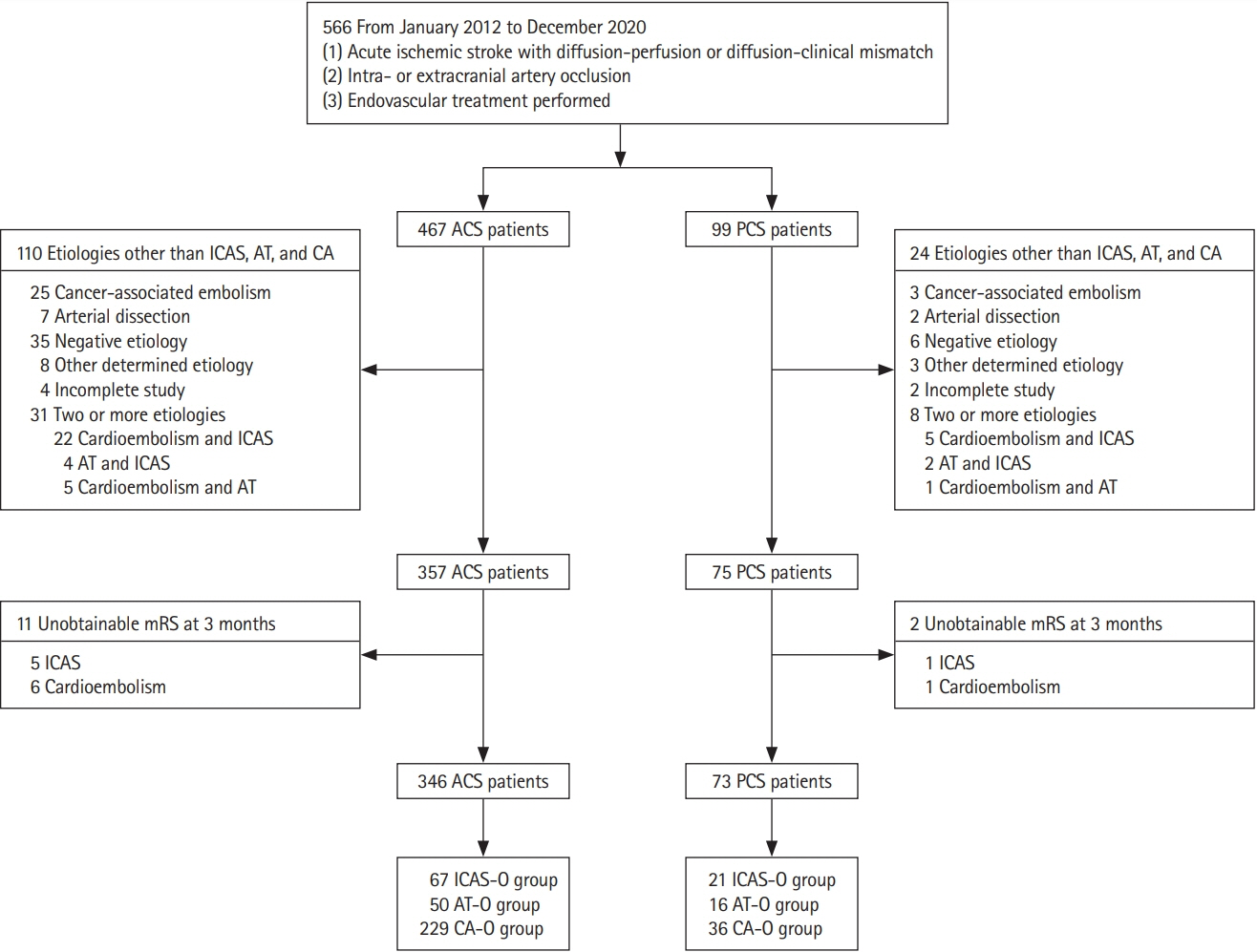
Methods
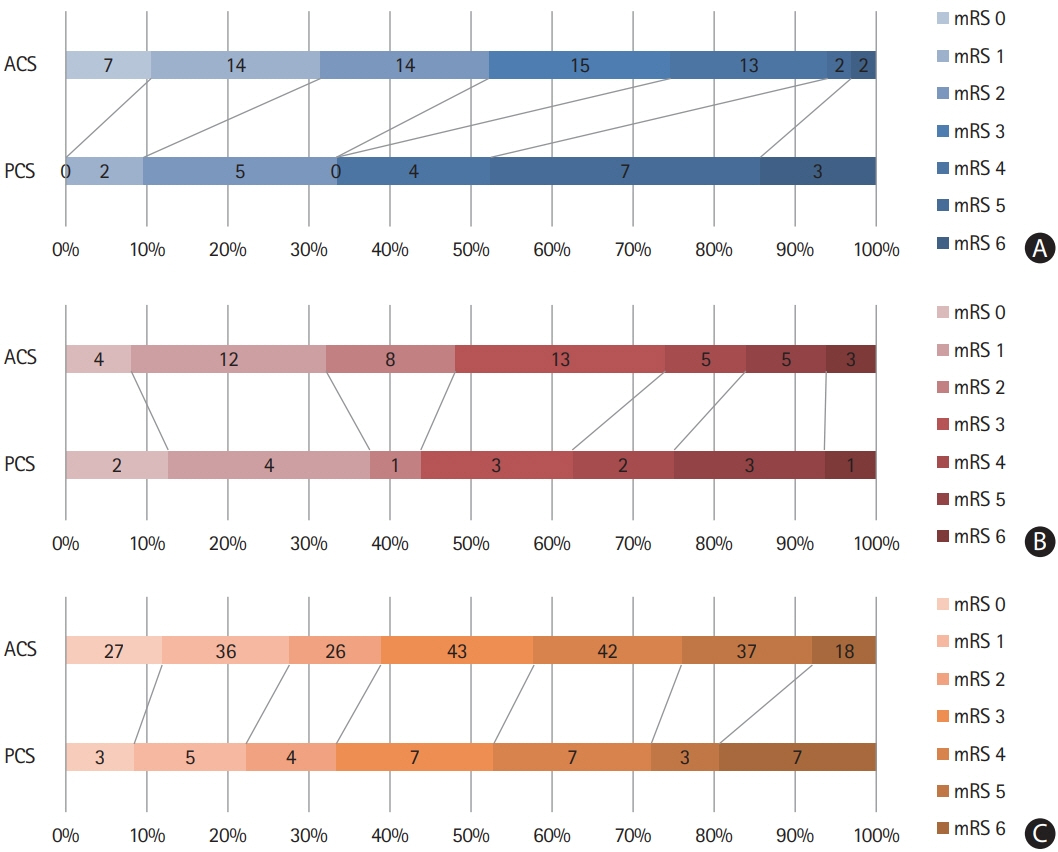
We retrospectively analyzed ischemic stroke patients who underwent EVT between January 2012 and December 2020. Enrolled ACS and PCS patients were compared according to etiologies (intracranial arterial steno-occlusion [ICAS-O], artery-to-artery embolic occlusion [AT-O], and cardioembolic occlusion [CA-O]). EVT procedure and favorable clinical outcomes at 3 months (modified Rankin Scale 0–2) were compared between the ACS and PCS groups for each etiology.
Results
We included 419 patients (ACS, 346; PCS, 73) including 88 ICAS-O (ACS, 67; PCS, 21), 66 AT-O (ACS, 50; PCS, 16), and 265 CA-O (ACS, 229; PCS, 36) patients in the study. The onset-to-recanalization time was longer in the PCS group than in the ACS group (median 628.0 minutes vs. 421.0 minutes, P=0.01). In CA-O patients, the door-to-puncture time was longer, whereas the puncture-to-recanalization time was shorter in the PCS group than in the ACS group. The proportions of successful recanalization and favorable clinical outcomes were similar between the ACS and PCS groups for all three etiologies. Low baseline National Institutes of Health Stroke Scale (NIHSS) scores and absence of intracerebral hemorrhage at follow-up imaging were associated with favorable clinical outcomes in both groups, whereas successful recanalization (odds ratio, 11.74; 95% confidence interval, 2.60 to 52.94; P=0.001) was only associated in the ACS group.
Conclusions
The proportions of successful recanalization and favorable clinical outcomes were similar among all three etiologies between PCS and ACS patients who underwent EVT. Initial baseline NIHSS score and absence of hemorrhagic transformation were related to favorable outcomes in the PCS and ACS groups, whereas successful recanalization was related to favorable outcomes only in the ACS group.
Figure
Cited by 3 articles
-
Resurrection of Endovascular Thrombectomy for Posterior Circulation Stroke
Jong S. Kim
J Stroke. 2022;24(2):177-178. doi: 10.5853/jos.2022.01620.Endovascular Treatment for Posterior Circulation Stroke: Ways to Maximize Therapeutic Efficacy
Seong-Joon Lee, Ji Man Hong, Jong S. Kim, Jin Soo Lee
J Stroke. 2022;24(2):207-223. doi: 10.5853/jos.2022.00941.A Review of Endovascular Treatment for Posterior Circulation Strokes
Sung Hyun Baik, Jun Yup Kim, Cheolkyu Jung
Neurointervention. 2023;18(2):90-106. doi: 10.5469/neuroint.2023.00213.
Reference
-
References
1. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; 378:708–718.
Article2. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; 378:11–21.3. Schonewille WJ, Wijman CA, Michel P, Rueckert CM, Weimar C, Mattle HP, et al. Treatment and outcomes of acute basilar artery occlusion in the Basilar Artery International Cooperation Study (BASICS): a prospective registry study. Lancet Neurol. 2009; 8:724–730.
Article4. Langezaal LC, van der Hoeven EJ, Mont’Alverne FJ, de Carvalho JJ, Lima FO, Dippel DW, et al. Endovascular therapy for stroke due to basilar-artery occlusion. N Engl J Med. 2021; 384:1910–1920.
Article5. Liu X, Dai Q, Ye R, Zi W, Liu Y, Wang H, et al. Endovascular treatment versus standard medical treatment for vertebrobasilar artery occlusion (BEST): an open-label, randomised controlled trial. Lancet Neurol. 2020; 19:115–122.6. Rentzos A, Karlsson JE, Lundqvist C, Rosengren L, Hellström M, Wikholm G. Endovascular treatment of acute ischemic stroke in the posterior circulation. Interv Neuroradiol. 2018; 24:405–411.
Article7. van Houwelingen RC, Luijckx GJ, Mazuri A, Bokkers RP, Eshghi OS, Uyttenboogaart M. Safety and outcome of intra-arterial treatment for basilar artery occlusion. JAMA Neurol. 2016; 73:1225–1230.
Article8. Yoon W, Kim SK, Park MS, Baek BH, Lee YY. Predictive factors for good outcome and mortality after stent-retriever thrombectomy in patients with acute anterior circulation stroke. J Stroke. 2017; 19:97–103.
Article9. Kim SJ, Seok JM, Bang OY, Kim GM, Kim KH, Jeon P, et al. MR mismatch profiles in patients with intracranial atherosclerotic stroke: a comprehensive approach comparing stroke subtypes. J Cereb Blood Flow Metab. 2009; 29:1138–1145.
Article10. Tiedt S, Herzberg M, Küpper C, Feil K, Kellert L, Dorn F, et al. Stroke etiology modifies the effect of endovascular treatment in acute stroke. Stroke. 2020; 51:1014–1016.11. Kang DH, Kim YW, Hwang YH, Park SP, Kim YS, Baik SK. Instant reocclusion following mechanical thrombectomy of in situ thromboocclusion and the role of low-dose intra-arterial tirofiban. Cerebrovasc Dis. 2014; 37:350–355.
Article12. Xun K, Mo J, Ruan S, Dai J, Zhang W, Lv Y, et al. A meta-analysis of prognostic factors in patients with posterior circulation stroke after mechanical thrombectomy. Cerebrovasc Dis. 2021; 50:185–199.
Article13. Yoon W, Kim SK, Heo TW, Baek BH, Lee YY, Kang HK. Predictors of good outcome after stent-retriever thrombectomy in acute basilar artery occlusion. Stroke. 2015; 46:2972–2975.
Article14. Lee SJ, Hong JM, Choi JW, Park JH, Park B, Kang DH, et al. Predicting endovascular treatment outcomes in acute vertebrobasilar artery occlusion: a model to aid patient selection from the ASIAN KR Registry. Radiology. 2020; 294:628–637.
Article15. Wu L, Rajah GB, Cosky EE, Wu X, Li C, Chen J, et al. Outcomes in endovascular therapy for basilar artery occlusion: intracranial atherosclerotic disease vs. embolism. Aging Dis. 2021; 12:404–414.
Article16. Luo G, Mo D, Tong X, Liebeskind DS, Song L, Ma N, et al. Factors associated with 90-day outcomes of patients with acute posterior circulation stroke treated by mechanical thrombectomy. World Neurosurg. 2018; 109:e318–e328.
Article17. Sefcik RK, Tonetti DA, Desai SM, Casillo SM, Lang MJ, Jadhav AP, et al. Does stroke etiology influence outcome in the posterior circulation?: an analysis of 107 consecutive acute basilar occlusion thrombectomies. Neurosurg Focus. 2021; 51:E7.
Article18. Lee D, Lee DH, Suh DC, Kim BJ, Kwon SU, Kwon HS, et al. Endovascular treatment in patients with cerebral artery occlusion of three different etiologies. J Stroke. 2020; 22:234–244.
Article19. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article20. Archer CR, Horenstein S. Basilar artery occlusion: clinical and radiological correlation. Stroke. 1977; 8:383–390.
Article21. Lee D, Lee DH, Suh DC, Kwon HS, Jeong DE, Kim JG, et al. Intra-arterial thrombectomy for acute ischaemic stroke patients with active cancer. J Neurol. 2019; 266:2286–2293.
Article22. Fiorelli M, Bastianello S, von Kummer R, del Zoppo GJ, Larrue V, Lesaffre E, et al. Hemorrhagic transformation within 36 hours of a cerebral infarct: relationships with early clinical deterioration and 3-month outcome in the European Cooperative Acute Stroke Study I (ECASS I) cohort. Stroke. 1999; 30:2280–2284.
Article23. von Kummer R, Broderick JP, Campbell BC, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification: classification of bleeding events after ischemic stroke and reperfusion therapy. Stroke. 2015; 46:2981–2986.24. Meyer L, Stracke CP, Jungi N, Wallocha M, Broocks G, Sporns PB, et al. Thrombectomy for primary distal posterior cerebral artery occlusion stroke: the TOPMOST Study. JAMA Neurol. 2021; 78:434–444.
Article25. Baik SH, Park HJ, Kim JH, Jang CK, Kim BM, Kim DJ. Mechanical thrombectomy in subtypes of basilar artery occlusion: relationship to recanalization rate and clinical outcome. Radiology. 2019; 291:730–737.
Article26. Lindsberg PJ, Soinne L, Tatlisumak T, Roine RO, Kallela M, Häppölä O, et al. Long-term outcome after intravenous thrombolysis of basilar artery occlusion. JAMA. 2004; 292:1862–1866.
Article27. Alverne FJ, Lima FO, Rocha FA, Bandeira DA, Lucena AF, Silva HC, et al. Unfavorable vascular anatomy during endovascular treatment of stroke: challenges and bailout strategies. J Stroke. 2020; 22:185–202.
Article28. Lindsberg PJ, Pekkola J, Strbian D, Sairanen T, Mattle HP, Schroth G. Time window for recanalization in basilar artery occlusion: speculative synthesis. Neurology. 2015; 85:1806–1815.
Article29. Malik AM, Vora NA, Lin R, Zaidi SF, Aleu A, Jankowitz BT, et al. Endovascular treatment of tandem extracranial/intracranial anterior circulation occlusions: preliminary single-center experience. Stroke. 2011; 42:1653–1657.
Article30. Wilson MP, Murad MH, Krings T, Pereira VM, O’Kelly C, Rempel J, et al. Management of tandem occlusions in acute ischemic stroke: intracranial versus extracranial first and extracranial stenting versus angioplasty alone: a systematic review and meta-analysis. J Neurointerv Surg. 2018; 10:721–728.
Article31. Compter A, van der Hoeven EJ, van der Worp HB, Vos JA, Weimar C, Rueckert CM, et al. Vertebral artery stenosis in the Basilar Artery International Cooperation Study (BASICS): prevalence and outcome. J Neurol. 2015; 262:410–417.
Article32. Piechowiak EI, Kaesmacher J, Zibold F, Dobrocky T, Mosimann PJ, Jung S, et al. Endovascular treatment of tandem occlusions in vertebrobasilar stroke: technical aspects and outcome compared with isolated basilar artery occlusion. J Neurointerv Surg. 2020; 12:25–29.
Article33. Cohen JE, Leker RR, Gomori JM, Eichel R, Rajz G, Moscovici S, et al. Emergent revascularization of acute tandem vertebrobasilar occlusions: endovascular approaches and technical considerations: confirming the role of vertebral artery ostium stenosis as a cause of vertebrobasilar stroke. J Clin Neurosci. 2016; 34:70–76.
Article34. Wang F, Wang J, He Q, Wang L, Cao Y, Zhang H, et al. Mechanical thrombectomy for posterior circulation occlusion: a comparison of outcomes with the anterior circulation occlusion: a meta-analysis. J Atheroscler Thromb. 2020; 27:1325–1339.
Article35. Huo X, Gao F, Ma N, Mo D, Sun X, et al. Characteristic and prognosis of acute large vessel occlusion in anterior and posterior circulation after endovascular treatment: the ANGEL registry real world experience. J Thromb Thrombolysis. 2020; 49:527–532.
Article36. Romano JG, Gardener H, Campo-Bustillo I, Khan Y, Tai S, Riley N, et al. Predictors of outcomes in patients with mild ischemic stroke symptoms: MaRISS. Stroke. 2021; 52:1995–2004.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Resurrection of Endovascular Thrombectomy for Posterior Circulation Stroke
- Endovascular Treatment for Posterior Circulation Stroke: Ways to Maximize Therapeutic Efficacy
- Intravenous Versus Intra-arterial Thrombolysis for Acute Ischemic Stroke Secondary to Basilar Artery Occlusion
- Treatment of the Posterior Circulation Aneurysms
- Collateral Circulation in Ischemic Stroke: An Updated Review