J Stroke.
2022 May;24(2):224-235. 10.5853/jos.2021.02152.
Association of Lipids, Lipoproteins, and Apolipoproteins with Stroke Subtypes in an International Case Control Study (INTERSTROKE)
- Affiliations
-
- 1Population Health Research Institute, McMaster University and Hamilton Health Sciences, Hamilton, ON, Canada
- 2Department of Medicine, HRB-Clinical Research Facility, NUI Galway, Galway, Ireland
- 3Division of Cardiology, McGill University Health Center, Montreal, QC, Canada
- 4National Center of Cardiovascular Disease, Beijing, China
- 5School of Medicine and Pharmacology, The University of Western Australia, Perth, Australia
- 6St John’s Medical College and Research Institute, Bangalore, India
- 7Beijing Hypertension League Institute, Beijing, China
- 8Fundacion Oftalmologica de Santander-Clinica Carlos Ardila Lulle (FOSCAL), Bucaramanga, Colombia
- 9Faculty of Medicine, Eduardo Mondlane University, Maputo, Mozambique
- 10Department of Geriatric Medicine, Glasgow Royal Infirmary, University of Glasgow, Glasgow, UK
- 11Department of Molecular and Clinical Medicine, Sahlgrenska Academy and University Hospital, University of Gothenburg, Gothenburg, Sweden
- 12College of Medicine, University of Philippines, Manila, Philippines
- 13Department of Surgery, Al Shaab Teaching Hospital, Khartoum, Sudan
- 14International Research Center, Hospital Alemão Oswaldo Cruz, Sao Paulo, Brazil
- 15Department of Cardiology, Kiruddu National Referral Hospital, Kampala, Uganda
- 16Institute for Medical Informatics, Department of Biometry and Epidemiology, University of Duisburg-Essen, Essen, Germany
- 17Institute of Psychiatry and Neurology, Warsaw, Poland
- 18Department of Neurology, Military Institute of Aviation Medicine, Warsaw, Poland
- 19National Research Center for Preventive Medicine, Ministry of Healthcare of the Russian Federation, Moscow, Russia
- 20Department of Medicine, Aga Khan University Hospital, Karachi, Pakistan
- 21Estudios Clínicos Latino America (ECLA), Instituto Cardiovascular de Rosario (ICR), Rosario, Argentina
- 22University College Sedaya International (UCSI) University, Kuala Lumpur, Malaysia
- 23Department of Medicine, Hatta Hospital, Dubai Health Authority, Dubai Medical College, Dubai, United Arab Emirates
- 24Department of Medicine, Istanbul Medeniyet University, Istanbul, Turkey
- 25Department of Cardiology, Hospital Luis Vernaza, Guayaquil, Ecuador
- 26Faculty of Medicine, University of La Frontera, Temuco, Chile
- 27Division of Cardiovascular Medicine, Department of Medicine, University College Hospital, Ibadan, Nigeria
- 28Department of Medicine, University College Hospital, Ibadan, Nigeria
- 29Rigshospitalet, University of Copenhagen, Copenhagen, Denmark
- 30Cayetano Heredia University, Lima, Peru
- 31Department of Medicine, University of Split, Split, Croatia
- 32Department of Neurology, Rush Alzheimer’s Disease Center, Chicago, IL, USA
- 33King Saud University, Riyadh, Saudi Arabia
- 34Neurology Division, Department of Medicine, Siriraj Hospital, Mahidol University, Bangkok, Thailand
- KMID: 2530525
- DOI: http://doi.org/10.5853/jos.2021.02152
Abstract
- Background and Purpose
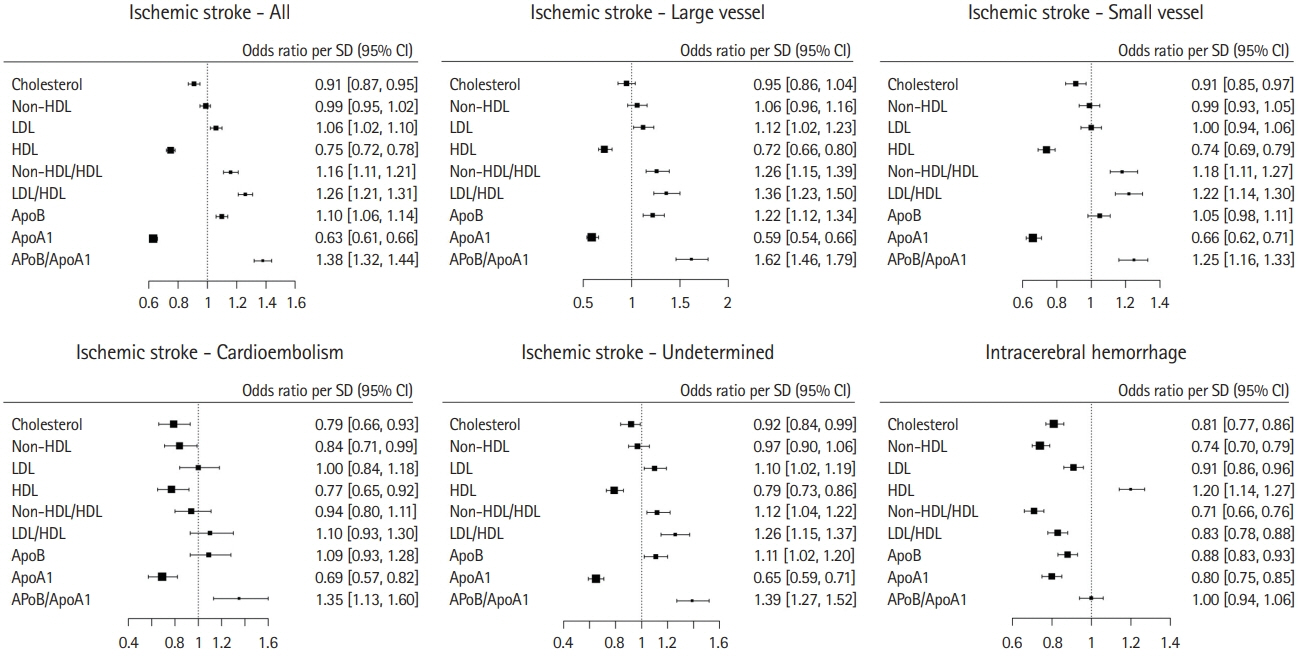
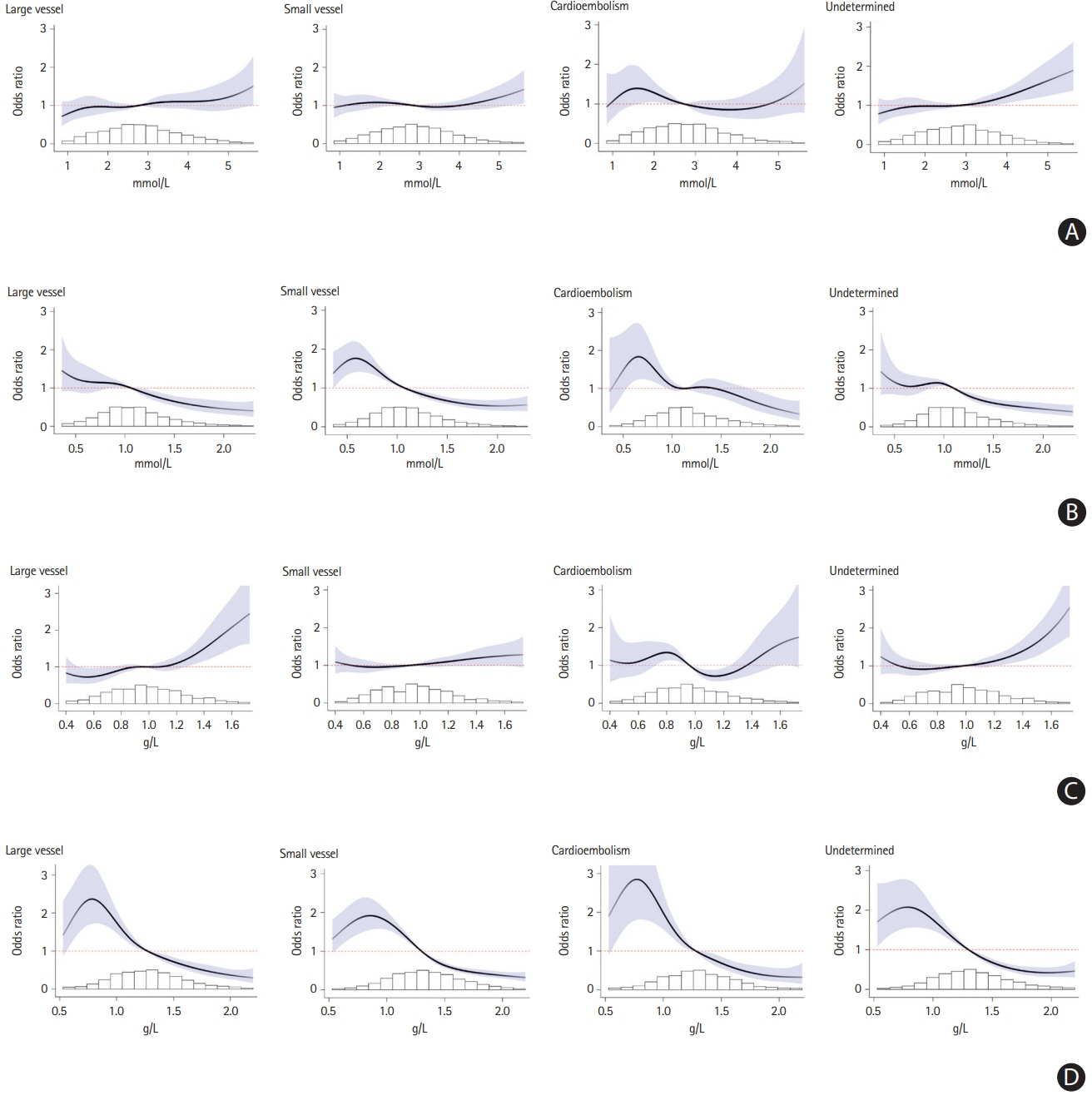
The association of dyslipidemia with stroke has been inconsistent, which may be due to differing associations within etiological stroke subtypes. We sought to determine the association of lipoproteins and apolipoproteins within stroke subtypes.
Methods
Standardized incident case-control STROKE study in 32 countries. Cases were patients with acute hospitalized first stroke, and matched by age, sex and site to controls. Concentrations of total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), apolipoprotein A1 (apoA1), and apoB were measured. Non-HDL-C was calculated. We estimated multivariable odds ratio (OR) and population attributable risk percentage (PAR%). Outcome measures were all stroke, ischemic stroke (and subtypes), and intracerebral hemorrhage (ICH).
Results
Our analysis included 11,898 matched case-control pairs; 77.3% with ischemic stroke and 22.7% with ICH. Increasing apoB (OR, 1.10; 95% confidence interval [CI], 1.06 to 1.14 per standard deviation [SD]) and LDL-C (OR, 1.06; 95% CI, 1.02 to 1.10 per SD) were associated with an increase in risk of ischemic stroke, but a reduced risk of ICH. Increased apoB was significantly associated with large vessel stroke (PAR 13.4%; 95% CI, 5.6 to 28.4) and stroke of undetermined cause. Higher HDL-C (OR, 0.75; 95% CI, 0.72 to 0.78 per SD) and apoA1 (OR, 0.63; 95% CI, 0.61 to 0.66 per SD) were associated with ischemic stroke (and subtypes). While increasing HDL-C was associated with an increased risk of ICH (OR, 1.20; 95% CI, 1.14 to 1.27 per SD), apoA1 was associated with a reduced risk (OR, 0.80; 95% CI, 0.75 to 0.85 per SD). ApoB/A1 (OR, 1.38; 95% CI, 1.32 to 1.44 per SD) had a stronger magnitude of association than the ratio of LDL-C/HDL-C (OR, 1.26; 95% CI, 1.21 to 1.31 per SD) with ischemic stroke (P<0.0001).
Conclusions
The pattern and magnitude of association of lipoproteins and apolipoproteins with stroke varies by etiological stroke subtype. While the directions of association for LDL, HDL, and apoB were opposing for ischemic stroke and ICH, apoA1 was associated with a reduction in both ischemic stroke and ICH. The ratio of apoB/A1 was the best lipid predictor of ischemic stroke risk.
Keyword
Figure
Reference
-
References
1. Thrift AG. Cholesterol is associated with stroke, but is not a risk factor. Stroke. 2004; 35:1524–1525.
Article2. Deedwania PC, Pedersen TR, DeMicco DA, Breazna A, Betteridge DJ, Hitman GA, et al. Differing predictive relationships between baseline LDL-C, systolic blood pressure, and cardiovascular outcomes. Int J Cardiol. 2016; 222:548–556.
Article3. van den Berg MJ, van der Graaf Y, de Borst GJ, Kappelle LJ, Nathoe HM, Visseren FL, et al. Low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, triglycerides, and apolipoprotein B and cardiovascular risk in patients with manifest arterial disease. Am J Cardiol. 2016; 118:804–810.
Article4. Pérez de Isla L, Alonso R, Mata N, Saltijeral A, Muñiz O, Rubio-Marin P, et al. Coronary heart disease, peripheral arterial disease, and stroke in familial hypercholesterolaemia: insights from the SAFEHEART Registry (Spanish Familial Hypercholesterolaemia Cohort Study). Arterioscler Thromb Vasc Biol. 2016; 36:2004–2010.
Article5. Ito T, Arima H, Fujiyoshi A, Miura K, Takashima N, Ohkubo T, et al. Relationship between non-high-density lipoprotein cholesterol and the long-term mortality of cardiovascular diseases: NIPPON DATA 90. Int J Cardiol. 2016; 220:262–267.
Article6. Imamura T, Doi Y, Ninomiya T, Hata J, Nagata M, Ikeda F, et al. Non-high-density lipoprotein cholesterol and the development of coronary heart disease and stroke subtypes in a general Japanese population: the Hisayama Study. Atherosclerosis. 2014; 233:343–348.
Article7. Prospective Studies Collaboration, Lewington S, Whitlock G, Clarke R, Sherliker P, Emberson J, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007; 370:1829–1839.
Article8. Holme I, Aastveit AH, Hammar N, Jungner I, Walldius G. Relationships between lipoprotein components and risk of ischaemic and haemorrhagic stroke in the Apolipoprotein MOrtality RISk study (AMORIS). J Intern Med. 2009; 265:275–287.
Article9. Emerging Risk Factors Collaboration, Di Angelantonio E, Sarwar N, Perry P, Kaptoge S, Ray KK, et al. Major lipids, apolipoproteins, and risk of vascular disease. JAMA. 2009; 302:1993–2000.
Article10. Emerging Risk Factors Collaboration, Danesh J, Erqou S, Walker M, Thompson SG, Tipping R, et al. The Emerging Risk Factors Collaboration: analysis of individual data on lipid, inflammatory and other markers in over 1.1 million participants in 104 prospective studies of cardiovascular diseases. Eur J Epidemiol. 2007; 22:839–869.
Article11. Chang JG, Paulson CP, Smith RF. Apolipoproteins for cardiovascular risk assessment. Am Fam Physician. 2014; 89:662A–662B.12. Ma Y, Li Z, Chen L, Li X. Blood lipid levels, statin therapy and the risk of intracerebral hemorrhage. Lipids Health Dis. 2016; 15:43.
Article13. Lee JS, Chang PY, Zhang Y, Kizer JR, Best LG, Howard BV. Triglyceride and HDL-C dyslipidemia and risks of coronary heart disease and ischemic stroke by glycemic dysregulation status: the Strong Heart Study. Diabetes Care. 2017; 40:529–537.
Article14. Glasser SP, Mosher A, Howard G, Banach M. What is the association of lipid levels and incident stroke? Int J Cardiol. 2016; 220:890–894.
Article15. Pikula A, Beiser AS, Wang J, Himali JJ, Kelly-Hayes M, Kase CS, et al. Lipid and lipoprotein measurements and the risk of ischemic vascular events: Framingham Study. Neurology. 2015; 84:472–479.
Article16. Wu J, Chen S, Liu L, Gao X, Zhou Y, Wang C, et al. Non-highdensity lipoprotein cholesterol vs low-density lipoprotein cholesterol as a risk factor for ischemic stroke: a result from the Kailuan study. Neurol Res. 2013; 35:505–511.
Article17. Araki A, Iimuro S, Sakurai T, Umegaki H, Iijima K, Nakano H, et al. Non-high-density lipoprotein cholesterol: an important predictor of stroke and diabetes-related mortality in Japanese elderly diabetic patients. Geriatr Gerontol Int. 2012; 12 Suppl 1:18–28.
Article18. Berger JS, McGinn AP, Howard BV, Kuller L, Manson JE, Otvos J, et al. Lipid and lipoprotein biomarkers and the risk of ischemic stroke in postmenopausal women. Stroke. 2012; 43:958–966.
Article19. Mora S, Buring JE, Ridker PM, Cui Y. Association of high-density lipoprotein cholesterol with incident cardiovascular events in women, by low-density lipoprotein cholesterol and apolipoprotein B100 levels: a cohort study. Ann Intern Med. 2011; 155:742–750.
Article20. Yokokawa H, Yasumura S, Tanno K, Ohsawa M, Onoda T, Itai K, et al. Serum low-density lipoprotein to high-density lipoprotein ratio as a predictor of future acute myocardial infarction among men in a 2.7-year cohort study of a Japanese northern rural population. J Atheroscler Thromb. 2011; 18:89–98.
Article21. Willey JZ, Xu Q, Boden-Albala B, Paik MC, Moon YP, Sacco RL, et al. Lipid profile components and risk of ischemic stroke: the Northern Manhattan Study (NOMAS). Arch Neurol. 2009; 66:1400–1406.22. Kurth T, Everett BM, Buring JE, Kase CS, Ridker PM, Gaziano JM. Lipid levels and the risk of ischemic stroke in women. Neurology. 2007; 68:556–562.
Article23. Walldius G, Aastveit AH, Jungner I. Stroke mortality and the apoB/apoA-I ratio: results of the AMORIS prospective study. J Intern Med. 2006; 259:259–266.
Article24. Wang X, Dong Y, Qi X, Huang C, Hou L. Cholesterol levels and risk of hemorrhagic stroke: a systematic review and meta-analysis. Stroke. 2013; 44:1833–1839.25. Lv P, Jin H, Liu Y, Cui W, Peng Q, Liu R, et al. Comparison of risk factor between lacunar stroke and large artery atherosclerosis stroke: a cross-sectional study in China. PLoS One. 2016; 11:e0149605.
Article26. Kumral E, Evyapan D, Gökçay F, Karaman B, Orman M. Association of baseline dyslipidemia with stroke recurrence within five-years after ischemic stroke. Int J Stroke. 2014; 9 Suppl A100:119–126.
Article27. Laloux P, Galanti L, Jamart J. Lipids in ischemic stroke subtypes. Acta Neurol Belg. 2004; 104:13–19.28. Bang OY, Saver JL, Liebeskind DS, Pineda S, Ovbiagele B. Association of serum lipid indices with large artery atherosclerotic stroke. Neurology. 2008; 70:841–847.
Article29. O’Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. 2016; 388:761–775.
Article30. O’Donnell M, Xavier D, Diener C, Sacco R, Lisheng L, Zhang H, et al. Rationale and design of INTERSTROKE: a global case-control study of risk factors for stroke. Neuroepidemiology. 2010; 35:36–44.
Article31. Hatano S. Experience from a multicentre stroke register: a preliminary report. Bull World Health Organ. 1976; 54:541–553.32. Bamford J, Sandercock P, Dennis M, Burn J, Warlow C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991; 337:1521–1526.
Article33. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke: definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article34. Aerden L, Luijckx GJ, Ricci S, Hilton A, Kessels F, Lodder J. Validation of the Oxfordshire Community Stroke Project syndrome diagnosis derived from a standard symptom list in acute stroke. J Neurol Sci. 2004; 220:55–58.
Article35. Mead GE, Lewis SC, Wardlaw JM, Dennis MS, Warlow CP. How well does the Oxfordshire community stroke project classification predict the site and size of the infarct on brain imaging? J Neurol Neurosurg Psychiatry. 2000; 68:558–562.
Article36. Bonita R, Beaglehole R. Recovery of motor function after stroke. Stroke. 1988; 19:1497–1500.
Article37. Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004; 364:937–952.
Article38. Benichou J, Gail MH. Variance calculations and confidence intervals for estimates of the attributable risk based on logistic models. Biometrics. 1990; 46:991–1003.
Article39. Hindy G, Engström G, Larsson SC, Traylor M, Markus HS, Melander O, et al. Role of blood lipids in the development of ischemic stroke and its subtypes: a Mendelian Randomization Study. Stroke. 2018; 49:820–827.
Article40. Hosomi N, Nagai Y, Kohriyama T, Ohtsuki T, Aoki S, Nezu T, et al. The Japan Statin Treatment Against Recurrent Stroke (J-STARS): a multicenter, randomized, open-label, parallel-group study. EBioMedicine. 2015; 2:1071–1078.
Article41. Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006; 355:549–559.
Article42. Amarenco P, Kim JS, Labreuche J, Charles H, Abtan J, Béjot Y, et al. A comparison of two LDL cholesterol targets after ischemic stroke. N Engl J Med. 2020; 382:9.
Article43. Yusuf S, Bosch J, Dagenais G, Zhu J, Xavier D, Liu L, et al. Cholesterol lowering in intermediate-risk persons without cardiovascular disease. N Engl J Med. 2016; 374:2021–2031.
Article44. Bhatia M, Howard SC, Clark TG, Neale R, Qizilbash N, Murphy MF, et al. Apolipoproteins as predictors of ischaemic stroke in patients with a previous transient ischaemic attack. Cerebrovasc Dis. 2006; 21:323–328.
Article45. Holmes MV, Millwood IY, Kartsonaki C, Hill MR, Bennett DA, Boxall R, et al. Lipids, lipoproteins, and metabolites and risk of myocardial infarction and stroke. J Am Coll Cardiol. 2018; 71:620–632.
Article46. Longstreth WT Jr, Arnold AM, Beauchamp NJ Jr, Manolio TA, Lefkowitz D, Jungreis C, et al. Incidence, manifestations, and predictors of worsening white matter on serial cranial magnetic resonance imaging in the elderly: the Cardiovascular Health Study. Stroke. 2005; 36:56–61.
Article47. Vernooij MW, van der Lugt A, Ikram MA, Wielopolski PA, Niessen WJ, Hofman A, et al. Prevalence and risk factors of cerebral microbleeds: the Rotterdam Scan Study. Neurology. 2008; 70:1208–1214.
Article48. Collins R, Armitage J, Parish S, Sleight P, Peto R; Heart Protection Study Collaborative Group. Effects of cholesterol-lowering with simvastatin on stroke and other major vascular events in 20536 people with cerebrovascular disease or other high-risk conditions. Lancet. 2004; 363:757–767.
Article49. Allara E, Morani G, Carter P, Gkatzionis A, Zuber V, Foley CN, et al. Genetic determinants of lipids and cardiovascular disease outcomes: a wide-angled Mendelian randomization investigation. Circ Genom Precis Med. 2019; 12:e002711.
Article50. Ko DT, Alter DA, Guo H, Koh M, Lau G, Austin PC, et al. High-density lipoprotein cholesterol and cause-specific mortality in individuals without previous cardiovascular conditions: the CANHEART Study. J Am Coll Cardiol. 2016; 68:2073–2083.
Article51. Boyce G, Button E, Soo S, Wellington C. The pleiotropic vasoprotective functions of high density lipoproteins (HDL). J Biomed Res. 2017; 32:164–182.52. Button EB, Boyce GK, Wilkinson A, Stukas S, Hayat A, Fan J, et al. ApoA-I deficiency increases cortical amyloid deposition, cerebral amyloid angiopathy, cortical and hippocampal astrogliosis, and amyloid-associated astrocyte reactivity in APP/PS1 mice. Alzheimers Res Ther. 2019; 11:44.
Article53. Anderson CD, Falcone GJ, Phuah CL, Radmanesh F, Brouwers HB, Battey TW, et al. Genetic variants in CETP increase risk of intracerebral hemorrhage. Ann Neurol. 2016; 80:730–740.54. Rhee EJ, Byrne CD, Sung KC. The HDL cholesterol/apolipoprotein A-I ratio: an indicator of cardiovascular disease. Curr Opin Endocrinol Diabetes Obes. 2017; 24:148–153.55. Barter PJ, Caulfield M, Eriksson M, Grundy SM, Kastelein JJ, Komajda M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007; 357:2109–2122.
Article56. Brunner FJ, Waldeyer C, Ojeda F, Salomaa V, Kee F, Sans S, et al. Application of non-HDL cholesterol for population-based cardiovascular risk stratification: results from the Multinational Cardiovascular Risk Consortium. Lancet. 2019; 394:2173–2183.
Article57. Mortensen MB, Nordestgaard BG. Elevated LDL cholesterol and increased risk of myocardial infarction and atherosclerotic cardiovascular disease in individuals aged 70-100 years: a contemporary primary prevention cohort. Lancet. 2020; 396:1644–1652.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study of Serum Lipids and Lipoproteins in Patients with Psoriasis
- Change of Serum Lipids, Lipoproteins and Apolipoproteins in Normal Pregnant Women at Term
- Plasma Lipids and Apolipoproteins as Risk Factor of Ischemic Heart Disease
- Lipoproteins and apolipoprotein B in patients with chronic renal failure receiving continuous ambulatory peritoneal dialysis
- Association of levels of serum lipids and lipoproteins with coronary artery disease documented by angiography