J Stroke.
2022 May;24(2):179-188. 10.5853/jos.2022.00843.
Therapeutic Trends of Cerebrovascular Disease during the COVID-19 Pandemic and Future Perspectives
- Affiliations
-
- 1Cooper Neurological Institute, Cooper University Hospital, Camden, NJ, USA
- 2Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
- 3Service of Neurology, Department of Clinical Neurosciences, Lausanne University Hospital, University of Lausanne, Lausanne, Switzerland
- KMID: 2530522
- DOI: http://doi.org/10.5853/jos.2022.00843
Abstract
- As of May 2022, there have been more than 400 million cases (including re-infections) of the systemic acute respiratory syndrome-coronavirus 2 (SARS-CoV-2), and nearly 5 million deaths worldwide. Not only has the coronavirus disease 2019 (COVID-19) pandemic been responsible for diagnosis and treatment delays of a wide variety of conditions, and overwhelmed the allocation of healthcare resources, it has impacted the epidemiology and management of cerebrovascular disease. In this narrative review, we summarize the changing paradigms and latest data regarding the complex relationship between COVID-19 and cerebrovascular disease. Paradoxically, although SARS-CoV-2 has been associated with many thrombotic complications—including ischemic stroke—there have been global declines in ischemic stroke and other cerebrovascular diseases. These epidemiologic shifts may be attributed to patient avoidance of healthcare institutions due to fear of contracting the novel human coronavirus, and also related to declines in other transmissible infectious illnesses which may trigger ischemic stroke. Despite the association between SARS-CoV-2 and thrombotic events, there are inconsistent data regarding targeted antithrombotics to prevent venous and arterial events. In addition, we provide recommendations for the conduct of stroke research and clinical trial planning during the ongoing COVID-19 pandemic, and for future healthcare crises.
Figure
Cited by 1 articles
-
Global Impact of the COVID-19 Pandemic on Cerebral Venous Thrombosis and Mortality
Thanh N. Nguyen, Muhammad M. Qureshi, Piers Klein, Hiroshi Yamagami, Mohamad Abdalkader, Robert Mikulik, Anvitha Sathya, Ossama Yassin Mansour, Anna Czlonkowska, Hannah Lo, Thalia S. Field, Andreas Charidimou, Soma Banerjee, Shadi Yaghi, James E. Siegler, Petra Sedova, Joseph Kwan, Diana Aguiar de Sousa, Jelle Demeestere, Violiza Inoa, Setareh Salehi Omran, Liqun Zhang, Patrik Michel, Davide Strambo, João Pedro Marto, Raul G. Nogueira
J Stroke. 2022;24(2):256-265. doi: 10.5853/jos.2022.00752.
Reference
-
References
1. Nogueira RG, Qureshi MM, Abdalkader M, Martins SO, Yamagami H, Qiu Z, et al. Global impact of COVID-19 on stroke care and IV thrombolysis. Neurology. 2021; 96:e2824–e2838.2. Nogueira RG, Abdalkader M, Qureshi MM, Frankel MR, Mansour OY, Yamagami H, et al. Global impact of COVID-19 on stroke care. Int J Stroke. 2021; 16:573–584.3. Nguyen TN, Haussen DC, Qureshi MM, Yamagami H, Fujinaka T, Mansour OY, et al. Decline in subarachnoid haemorrhage volumes associated with the first wave of the COVID-19 pandemic. Stroke Vasc Neurol. 2021; 6:542–552.4. Siegler JE, Cardona P, Arenillas JF, Talavera B, Guillen AN, Chavarría-Miranda A, et al. Cerebrovascular events and outcomes in hospitalized patients with COVID-19: the SVIN COVID-19 Multinational Registry. Int J Stroke. 2021; 16:437–447.
Article5. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020; 51:1996–2001.
Article6. Kansagra AP, Goyal MS, Hamilton S, Albers GW. Collateral effect of COVID-19 on stroke evaluation in the United States. N Engl J Med. 2020; 383:400–401.
Article7. Ortega-Gutierrez S, Farooqui M, Zha A, Czap A, Sebaugh J, Desai S, et al. Decline in mild stroke presentations and intravenous thrombolysis during the COVID-19 pandemic: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Clin Neurol Neurosurg. 2021; 201:106436.8. Olsen SJ, Azziz-Baumgartner E, Budd AP, Brammer L, Sullivan S, Pineda RF, et al. Decreased influenza activity during the COVID-19 pandemic: United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:1305–1309.
Article9. Htun P, Fateh-Moghadam S, Tomandl B, Handschu R, Klinger K, Stellos K, et al. Course of platelet activation and plateletleukocyte interaction in cerebrovascular ischemia. Stroke. 2006; 37:2283–2287.
Article10. Lee KR, Bae JH, Hwang IC, Kim KK, Suh HS, Ko KD. Effect of influenza vaccination on risk of stroke: a systematic review and meta-analysis. Neuroepidemiology. 2017; 48:103–110.
Article11. Lafond KE, Porter RM, Whaley MJ, Suizan Z, Ran Z, Aleem MA, et al. Global burden of influenza-associated lower respiratory tract infections and hospitalizations among adults: a systematic review and meta-analysis. PLoS Med. 2021; 18:e1003550.
Article12. Research and data to make progress against the world's largest problems. Our World in Data. https://ourworldindata.org. Accessed April 8, 2022.13. Yavagal DR, Saini V, Inoa V, Gardener HE, Martins SO, Fakey M, et al. International survey of mechanical thrombectomy stroke systems of care during COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021; 30:105806.
Article14. Srivastava PK, Zhang S, Xian Y, Xu H, Rutan C, Alger HM, et al. Acute ischemic stroke in patients with COVID-19: an analysis from get with the guidelines-stroke. Stroke. 2021; 52:1826–1829.15. Qureshi AI, Baskett WI, Huang W, Shyu D, Myers D, Raju M, et al. Acute ischemic stroke and COVID-19: an analysis of 27676 patients. Stroke. 2021; 52:905–912.16. de Havenon A, Ney JP, Callaghan B, Delic A, Hohmann S, Shippey E, et al. Impact of COVID-19 on outcomes in ischemic stroke patients in the United States. J Stroke Cerebrovasc Dis. 2021; 30:105535.
Article17. Sasanejad P, Afshar Hezarkhani L, Arsang-Jang S, Tsivgoulis G, Ghoreishi A, Kristian B, et al. Safety and outcomes of intravenous thrombolytic therapy in ischemic stroke patients with COVID-19: CASCADE Initiative. J Stroke Cerebrovasc Dis. 2021; 30:106121.
Article18. Leasure AC, Khan YM, Iyer R, Elkind M, Sansing LH, Falcone GJ, et al. Intracerebral hemorrhage in patients with COVID-19: an analysis from the COVID-19 Cardiovascular Disease Registry. Stroke. 2021; 52:e321–e323.19. Poyiadji N, Shahin G, Noujaim D, Stone M, Patel S, Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020; 296:E119–E120.20. Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Blood. 2020; 135:2033–2040.
Article21. Henry BM, Cheruiyot I, Benoit JL, Lippi G, Prohászka Z, Favaloro EJ, et al. Circulating levels of tissue plasminogen activator and plasminogen activator inhibitor-1 are independent predictors of coronavirus disease 2019 severity: a prospective, observational study. Semin Thromb Hemost. 2021; 47:451–455.
Article22. Bhatia R, Pedapati R, Komakula S, Srivastava M, Vishnubhatla S, Khurana D. Stroke in coronavirus disease 2019: a systematic review. J Stroke. 2020; 22:324–335.
Article23. Ramos-Araque ME, Siegler JE, Ribo M, Requena M, López C, de Lera M, et al. Stroke etiologies in patients with COVID-19: the SVIN COVID-19 multinational registry. BMC Neurol. 2021; 21:43.
Article24. Strambo D, De Marchis GM, Bonati LH, Arnold M, Carrera E, Galletta S, et al. Ischemic stroke in COVID-19 patients: Mechanisms, treatment, and outcomes in a consecutive Swiss Stroke Registry analysis. Eur J Neurol. 2022; 29:732–743.
Article25. Wolter N, Jassat W, Walaza S, Welch R, Moultrie H, Groome M, et al. Early assessment of the clinical severity of the SARS-CoV-2 Omicron variant in South Africa. bioRxiv. 2021; Dec. 21. [Preprint]. https://doi.org/10.1101/2021.12.21.21268116.
Article26. Hottz ED, Azevedo-Quintanilha IG, Palhinha L, Teixeira L, Barreto EA, Pão C, et al. Platelet activation and plateletmonocyte aggregate formation trigger tissue factor expression in patients with severe COVID-19. Blood. 2020; 136:1330–1341.
Article27. Tan M, Liu Y, Zhou R, Deng X, Li F, Liang K, et al. Immunopathological characteristics of coronavirus disease 2019 cases in Guangzhou, China. Immunology. 2020; 160:261–268.
Article28. Syed F, Li W, Relich RF, Russell PM, Zhang S, Zimmerman MK, et al. Excessive matrix metalloproteinase-1 and hyperactivation of endothelial cells occurred in COVID-19 patients and were associated with the severity of COVID-19. J Infect Dis. 2021; 224:60–69.
Article29. Velavan TP, Meyer CG. Mild versus severe COVID-19: laboratory markers. Int J Infect Dis. 2020; 95:304–307.
Article30. Manne BK, Denorme F, Middleton EA, Portier I, Rowley JW, Stubben C, et al. Platelet gene expression and function in patients with COVID-19. Blood. 2020; 136:1317–1329.
Article31. Yatim N, Boussier J, Chocron R, Hadjadj J, Philippe A, Gendron N, et al. Platelet activation in critically ill COVID-19 patients. Ann Intensive Care. 2021; 11:113.
Article32. Ma A, Kase CS, Shoamanesh A, Abdalkader M, Pikula A, Sathya A, et al. Stroke and thromboprophylaxis in the era of COVID-19. J Stroke Cerebrovasc Dis. 2021; 30:105392.
Article33. Bonaventura A, Vecchié A, Dagna L, Martinod K, Dixon DL, Van Tassell BW, et al. Endothelial dysfunction and immunothrombosis as key pathogenic mechanisms in COVID-19. Nat Rev Immunol. 2021; 21:319–329.
Article34. Lallana S, Chen A, Requena M, Rubiera M, Sanchez A, Siegler JE, et al. Posterior reversible encephalopathy syndrome (PRES) associated with COVID-19. J Clin Neurosci. 2021; 88:108–112.
Article35. Smadja DM, Guerin CL, Chocron R, Yatim N, Boussier J, Gendron N, et al. Angiopoietin-2 as a marker of endothelial activation is a good predictor factor for intensive care unit admission of COVID-19 patients. Angiogenesis. 2020; 23:611–620.
Article36. McAlpine LS, Zubair AS, Maran I, Chojecka P, Lleva P, Jasne AS, et al. Ischemic stroke, inflammation, and endotheliopathy in COVID-19 patients. Stroke. 2021; 52:e233–e238.
Article37. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020; 395:1417–1418.
Article38. Keller E, Brandi G, Winklhofer S, Imbach LL, Kirschenbaum D, Frontzek K, et al. Large and small cerebral vessel involvement in severe COVID-19: detailed clinical workup of a case series. Stroke. 2020; 51:3719–3722.
Article39. Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City health system. JAMA. 2020; 324:799–801.
Article40. Jiménez D, García-Sanchez A, Rali P, Muriel A, Bikdeli B, Ruiz-Artacho P, et al. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest. 2021; 159:1182–1196.
Article41. ATTACC Investigators; ACTIV-4a Investigators; REMAP-CAP Investigators, Lawler PR, Goligher EC, Berger JS, et al. Therapeutic anticoagulation with heparin in noncritically ill patients with COVID-19. N Engl J Med. 2021; 385:790–802.
Article42. Lopes RD, de Barros E Silva P, Furtado R, Macedo A, Bronhara B, Damiani LP, et al. Therapeutic versus prophylactic anticoagulation for patients admitted to hospital with COVID-19 and elevated D-dimer concentration (ACTION): an open-label, multicentre, randomised, controlled trial. Lancet. 2021; 397:2253–2263.43. REMAP-CAP Investigators; ACTIV-4a Investigators; ATTACC Investigators, Goligher EC, Bradbury CA, McVerry BJ, et al. Therapeutic anticoagulation with heparin in critically ill patients with COVID-19. N Engl J Med. 2021; 385:777–789.
Article44. INSPIRATION Investigators, Sadeghipour P, Talasaz AH, Rashidi F, Sharif-Kashani B, Beigmohammadi MT, et al. Effect of intermediate-dose vs standard-dose prophylactic anticoagulation on thrombotic events, extracorporeal membrane oxygenation treatment, or mortality among patients with COVID-19 admitted to the intensive care unit: the INSPIRATION randomized clinical trial. JAMA. 2021; 325:1620–1630.45. Chatterjee S, Chakraborty A, Weinberg I, Kadakia M, Wilensky RL, Sardar P, et al. Thrombolysis for pulmonary embolism and risk of all-cause mortality, major bleeding, and intracranial hemorrhage: a meta-analysis. JAMA. 2014; 311:2414–2421.
Article46. Harris SK, Bone RC, Ruth WE. Gastrointestinal hemorrhage in patients in a respiratory intensive care unit. Chest. 1977; 72:301–304.
Article47. Nguyen TN, Abdalkader M, Jovin TG, Nogueira RG, Jadhav AP, Haussen DC, et al. Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams. A guidance statement from the Society of Vascular and Interventional Neurology. Stroke. 2020; 51:1896–1901.
Article48. Katsanos AH, Palaiodimou L, Zand R, Yaghi S, Kamel H, Navi BB, et al. Changes in stroke hospital care during the COVID-19 pandemic: a systematic review and meta-analysis. Stroke. 2021; 52:3651–3660.
Article49. Siegler JE, Zha AM, Czap AL, Ortega-Gutierrez S, Farooqui M, Liebeskind DS, et al. Influence of the COVID-19 pandemic on treatment times for acute ischemic stroke: the Society of Vascular and Interventional Neurology Multicenter Collaboration. Stroke. 2021; 52:40–47.
Article50. Plumereau C, Cho TH, Buisson M, Amaz C, Cappucci M, Derex L, et al. Effect of the COVID-19 pandemic on acute stroke reperfusion therapy: data from the Lyon Stroke Center Network. J Neurol. 2021; 268:2314–2319.
Article51. Fuentes B, Alonso de Leciñana M, García-Madrona S, Díaz-Otero F, Aguirre C, Calleja P, et al. Stroke acute management and outcomes during the COVID-19 outbreak: a cohort study from the Madrid Stroke Network. Stroke. 2021; 52:552–562.
Article52. Chen Y, Nguyen TN, Wellington J, Mofatteh M, Yao W, Hu Z, et al. Shortening door-to-needle time by multidisciplinary collaboration and workflow optimization during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2022; 31:106179.
Article53. Hall J, Thon JM, Heslin M, Thau L, Yeager T, Siegal T, et al. Tenecteplase improves door-to-needle time in real-world acute stroke treatment. Stroke Vasc Interv Neurol. 2021; 1:e000102.
Article54. Warach SJ, Saver JL. Stroke thrombolysis with tenecteplase to reduce emergency department spread of coronavirus disease 2019 and shortages of alteplase. JAMA Neurol. 2020; 77:1203–1204.
Article55. Meinel TR, Kaesmacher J, Mosimann PJ, Seiffge D, Jung S, Mordasini P, et al. Association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2020; 95:e2331–e2342.
Article56. Meinel TR, Kaesmacher J, Fischer U. Author response: association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2021; 96:916–917.
Article57. Siegler JE, Thon JM. Reader response: association of initial imaging modality and futile recanalization after thrombectomy. Neurology. 2021; 96:915–916.
Article58. Kaesmacher J, Chaloulos-Iakovidis P, Panos L, Mordasini P, Michel P, Hajdu SD, et al. Mechanical thrombectomy in ischemic stroke patients with Alberta Stroke Program Early Computed Tomography Score 0-5. Stroke. 2019; 50:880–888.
Article59. Nguyen TN, Abdalkader M, Nagel S, Qureshi MM, Ribo M, Caparros F, et al. Noncontrast computed tomography vs computed tomography perfusion or magnetic resonance imaging selection in late presentation of stroke with largevessel occlusion. JAMA Neurol. 2022; 79:22–31.
Article60. Seker F, Qureshi MM, Möhlenbruch M, Nogueira RG, AbdalKader M, Ribo M, et al. Abstract TMP67: Predictors of unfavourable events despite successful mechanical thrombectomy in the extended window. Stroke. 2022; 53(Suppl 1):ATMP67.
Article61. Nguyen TN, Nogueira RG, Jovin TG. Response by Nguyen et al to letter regarding article, “Mechanical thrombectomy in the era of the COVID-19 pandemic: emergency preparedness for neuroscience teams: a guidance statement from the society of vascular and interventional neurology”. Stroke. 2020; 51:e172–e173.
Article62. Al Kasab S, Almallouhi E, Alawieh A, Levitt MR, Jabbour P, Sweid A, et al. International experience of mechanical thrombectomy during the COVID-19 pandemic: insights from STAR and ENRG. J Neurointerv Surg. 2020; 12:1039–1044.
Article63. Campbell D, Diprose WK, Deng C, Barber PA. General anesthesia versus conscious sedation in endovascular thrombectomy for stroke: a meta-analysis of 4 randomized controlled trials. J Neurosurg Anesthesiol. 2021; 33:21–27.
Article64. AHA/ASA Stroke Council Leadership. Temporary emergency guidance to US stroke centers during the coronavirus disease 2019 (COVID-19) pandemic: on behalf of the American Heart Association/American Stroke Association Stroke Council Leadership. Stroke. 2020; 51:1910–1912.65. Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020; 21:1023–1034.
Article66. Williams R, Jenkins DA, Ashcroft DM, Brown B, Campbell S, Carr MJ, et al. Diagnosis of physical and mental health conditions in primary care during the COVID-19 pandemic: a retrospective cohort study. Lancet Public Health. 2020; 5:e543–e550.
Article67. Sisó-Almirall A, Kostov B, Sánchez E, Benavent-Àreu J, Paz LG. Impact of the COVID-19 pandemic on primary health care disease incidence rates: 2017 to 2020. Ann Fam Med. 2022; 20:63–68.
Article68. Thau L, Siegal T, Heslin ME, Rana A, Yu S, Kamen S, et al. Decline in rehab transfers among rehab-eligible stroke patients during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021; 30:105857.
Article69. Hatcher-Martin JM, Adams JL, Anderson ER, Bove R, Burrus TM, Chehrenama M, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology. 2020; 94:30–38.70. Nam HS, Park E, Heo JH. Facilitating stroke management using modern information technology. J Stroke. 2013; 15:135–143.
Article71. Wilcock AD, Schwamm LH, Zubizarreta JR, Zachrison KS, Uscher-Pines L, Richard JV, et al. Reperfusion treatment and stroke outcomes in hospitals with telestroke capacity. JAMA Neurol. 2021; 78:527–535.
Article72. Guzik AK, Martin-Schild S, Tadi P, Chapman SN, Al Kasab S, Martini SR, et al. Telestroke across the continuum of care: lessons from the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2021; 30:105802.
Article73. Moghimi N, Di Napoli M, Biller J, Siegler JE, Shekhar R, McCullough LD, et al. The neurological manifestations of postacute sequelae of SARS-CoV-2 infection. Curr Neurol Neurosci Rep. 2021; 21:44.
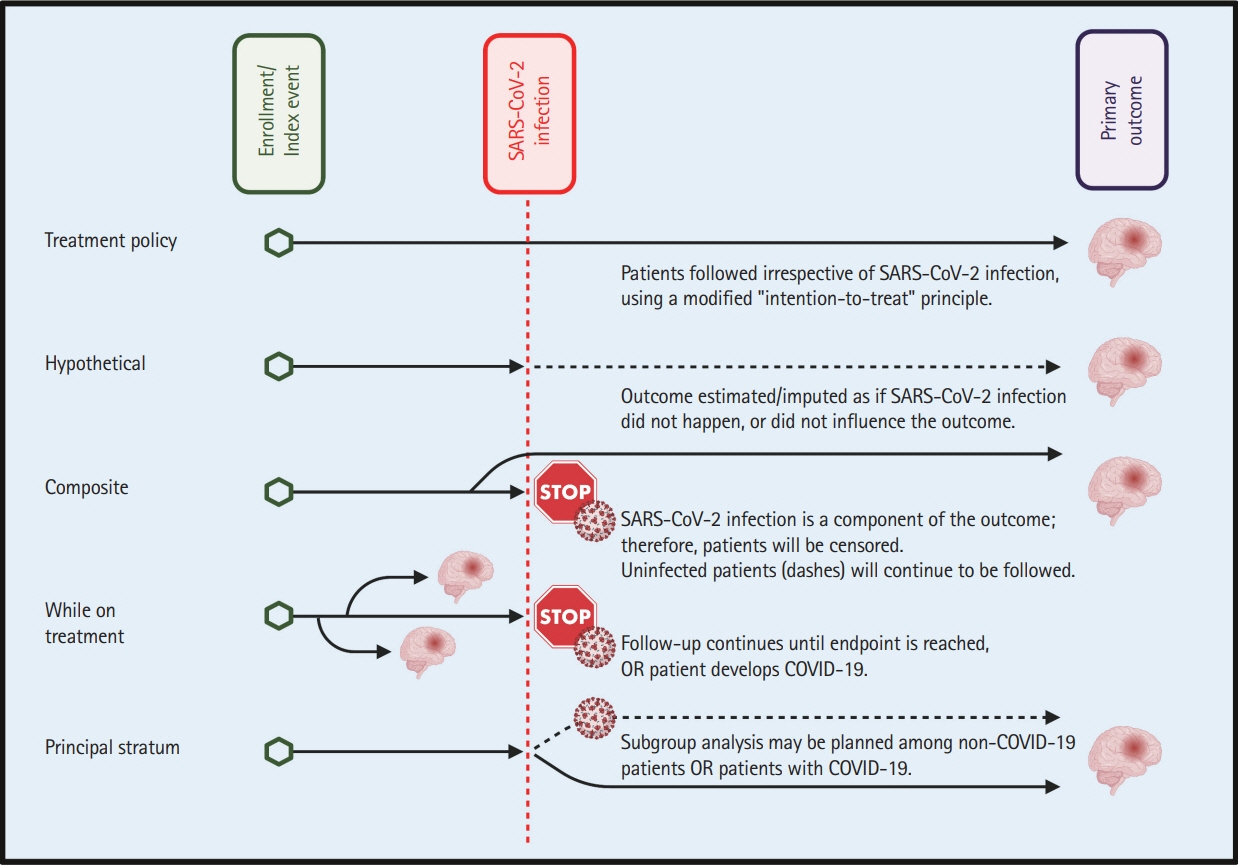
Article74. Yassi N, Hayward KS, Campbell B, Churilov L. Use of the estimand framework to manage the disruptive effects of COVID-19 on stroke clinical trials. Stroke. 2021; 52:3739–3747.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Food service industry in the era of COVID-19: trends and research implications
- Age-Related Morbidity and Mortality among Patients with COVID-19
- The Management of Thyroid Disease in COVID-19 Pandemic
- Management of Patients with Chronic Liver Disease: The Era of the COVID-19 Pandemic
- Laryngoscopy During the COVID-19 Pandemic