Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2019
- Affiliations
-
- 1Korea Central Cancer Registry, National Cancer Center, Goyang, Korea
- 2Division of Cancer Registration and Surveillance, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 3National Cancer Center Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- 4National Cancer Control Institute, National Cancer Center, Goyang, Korea
- KMID: 2528203
- DOI: http://doi.org/10.4143/crt.2022.128
Abstract
- Purpose
The current study provides national cancer statistics and their secular trends in Korea, including incidence, mortality, survival, and prevalence in 2019.
Materials and Methods
Incidence, survival, and prevalence rates of cancer were calculated using the Korea National Cancer Incidence Database, from 1999 to 2019, with survival follow-up until December 31, 2020. Deaths from cancer were assessed using causes-of-death data obtained from Statistics Korea.
Results
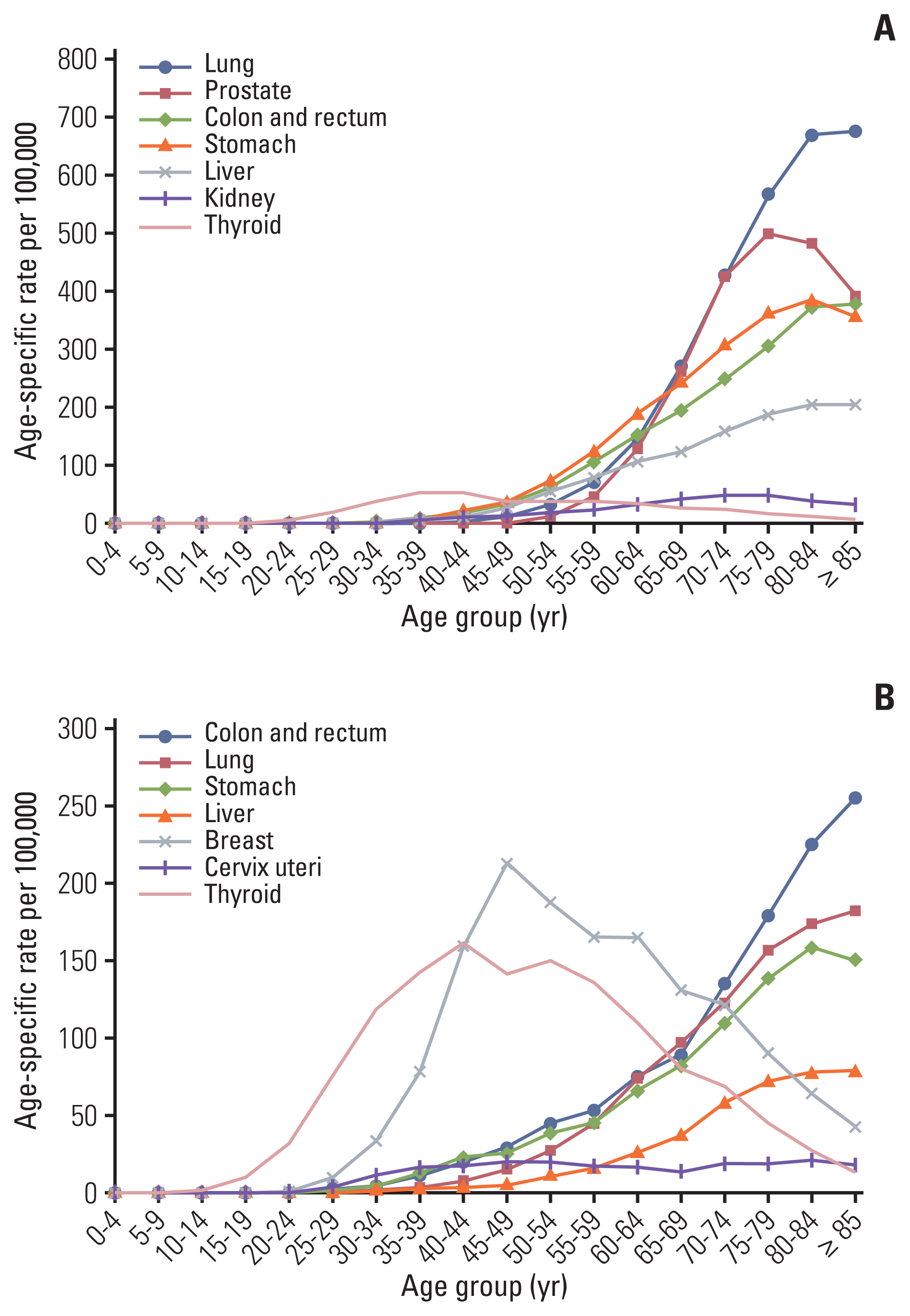
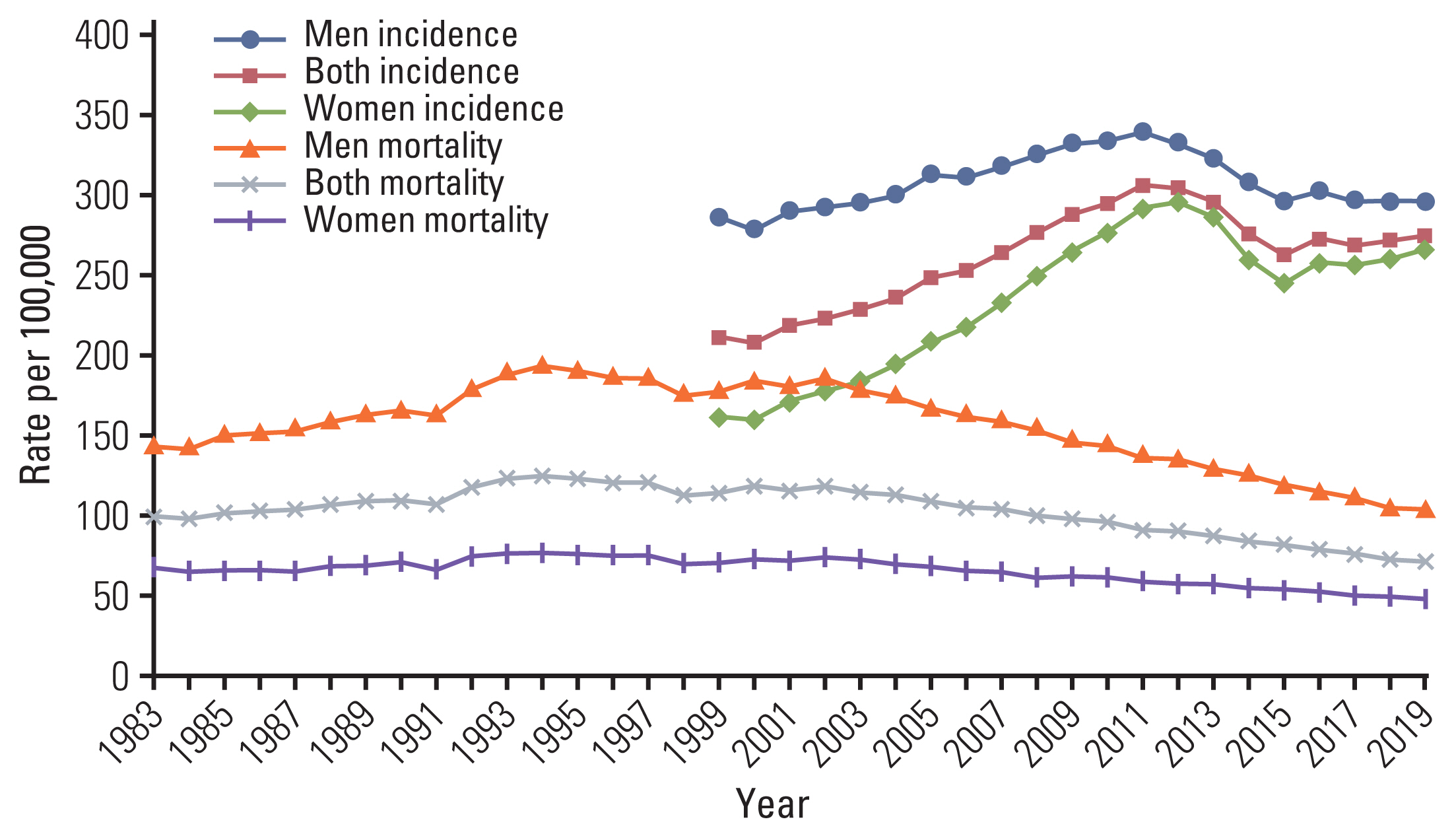
In 2019, newly diagnosed cancer cases and deaths from cancer were reported as 254,718 (ASR, 275.4 per 100,000) and 81,203 (ASR, 72.2 per 100,000), respectively. For the first time, lung cancer (n=29,960) became the most frequent cancer in Korea, excluding thyroid cancer. The overall cancer incidence rates increased by 3.3% annually from 1999 to 2012, and decreased by 5.3% annually from 2012 to 2015, thereafter, followed by nonsignificant changes. The incidence of thyroid cancer increased again from 2016 (annual percentage change, 6.2%). Cancer mortality rates have been decreasing since 2002, with more rapid decline in recent years (annual decrease of 2.7% from 2002 to 2013; 3.3% from 2013 to 2019). The 5-year relative survival between 2015 and 2019 was 70.7%, which contributed to prevalent cases reaching over 2 million in 2019.
Conclusion
Cancer survival rates have improved over the past decades, but the number of newly diagnosed cancers is still increasing, with some cancers showing only marginal improvement in survival outcomes. As the number of cancer survivors increases, a comprehensive cancer control strategy should be implemented in line with the changing aspects of cancer statistics.
Figure
Cited by 19 articles
-
Update on Diagnosis and Treatment of Colorectal Cancer
Chan Wook Kim
Ewha Med J. 2022;45(4):e8. doi: 10.12771/emj.2022.e8.Cancer Rehabilitation Fact Sheet in Korea
Jin A Yoon, Bo Young Hong
Ann Rehabil Med. 2022;46(4):155-162. doi: 10.5535/arm.22102.Analysis of prognostic factors through survival rate analysis of oral squamous cell carcinoma patients treated at the National Cancer Center: 20 years of experience
Yong-Seok Choi, Min Gyeong Kim, Jong-Ho Lee, Joo-Yong Park, Sung-Weon Choi
J Korean Assoc Oral Maxillofac Surg. 2022;48(5):284-291. doi: 10.5125/jkaoms.2022.48.5.284.Quality Assessment and Trend for Breast Cancer Treatment Practice across South Korea Based on Nationwide Analysis of Korean Health Insurance Data during 2013–2017
Kyu Hye Choi, Soo-Yoon Sung, Sea-Won Lee, Ye Won Jeon, Sung Hwan Kim, Jong Hoon Lee
Cancer Res Treat. 2023;55(2):570-579. doi: 10.4143/crt.2022.882.Overview of the National Cancer Screening Program for Colorectal Cancer in Korea over 14 Years (2004–2017)
Bomi Park, Eun Young Her, Kyeongmin Lee, Fatima Nari, Jae Kwan Jun, Kui Son Choi, Mina Suh
Cancer Res Treat. 2023;55(3):910-917. doi: 10.4143/crt.2022.1432.Right Then, Wrong Now: Early-Onset Colorectal Cancer in Korea
Aesun Shin, Kyu-Won Jung, Seung-Yong Jeong
Cancer Res Treat. 2023;55(3):1058-1060. doi: 10.4143/crt.2022.1612.Comprehensive Analysis of Iron Deficiency Anemia and Its Related Disorders in Premenopausal Women Based on a Propensity Score Matching Case Control Study Using National Health Insurance Service Database in Korea
Hyun Jung Lee, Haeyong Pak, Jae Joon Han, Myung Hee Chang
J Korean Med Sci. 2023;38(37):e299. doi: 10.3346/jkms.2023.38.e299.Increased Screening Rates for Thyroid Cancer Among Residents Living Near Nuclear Power Plants
Ga Bin Lee, Soojin Park, Won Il Jang, Sunhoo Park, Jae Kwan Jun, Songwon Seo
J Korean Med Sci. 2023;38(44):e369. doi: 10.3346/jkms.2023.38.e369.Incidence, mortality and survival of gallbladder, extrahepatic bile duct, and pancreatic cancer using Korea central cancer registry database: 1999-2019
Mee Joo Kang, E Hwa Yun, Kyu-Won Jung, Sang-Jae Park
Int J Stem Cells. 2022;26(3):220-228. doi: 10.14701/ahbps.22-041.Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999-2019
Sung Yeon Hong, Mee Joo Kang, Taegyu Kim, Kyu-Won Jung, Bong-Wan Kim
Int J Stem Cells. 2022;26(3):211-219. doi: 10.14701/ahbps.22-044.Post-percutaneous core needle biopsy sputum cytology: diagnostic value and factors for positive prediction in diagnosing malignancy
Sang Kyu Lee, Hee Kang, Min Jung Jung, Sekyoung Park, Ki Nam Lee
Kosin Med J. 2023;38(3):201-209. doi: 10.7180/kmj.23.127.Exocrine pancreatic cancer as a second primary malignancy: A population-based study
Mee Joo Kang, Jiwon Lim, Sung-Sik Han, Hyeong Min Park, Sung Chun Cho, Sang-Jae Park, Sun-Whe Kim, Young-Joo Won
Ann Hepatobiliary Pancreat Surg. 2023;27(4):415-422. doi: 10.14701/ahbps.23-053.Implication of Pre- and Post-radiotherapy ctDNA Dynamics in Patients with Residual Triple-Negative Breast Cancer at Surgery after Neoadjuvant Chemotherapy: Findings from a Prospective Observational Study
Tae Hoon Lee, Haeyoung Kim, Yeon Jeong Kim, Woong-Yang Park, Won Park, Won Kyung Cho, Nalee Kim
Cancer Res Treat. 2024;56(2):531-537. doi: 10.4143/crt.2023.996.Advancing Korean nationwide registry for hepatocellular carcinoma: a systematic sampling approach utilizing the Korea Central Cancer Registry database
Bo Hyun Kim, E Hwa Yun, Jeong-Hoon Lee, Geun Hong, Jun Yong Park, Ju Hyun Shim, Eunyang Kim, Hyun-Joo Kong, Kyu-Won Jung, Young-Suk Lim
J Liver Cancer. 2024;24(1):57-61. doi: 10.17998/jlc.2024.03.03.Korean National Burden of Disease: The Importance of Diabetes Management
Chung-Nyun Kim, Yoon-Sun Jung, Young-Eun Kim, Minsu Ock, Seok-Jun Yoon
Diabetes Metab J. 2024;48(4):518-530. doi: 10.4093/dmj.2024.0087.Neoadjuvant Cisplatin-Based Chemotherapy Followed by Selective Bladder Preservation Chemoradiotherapy in Muscle-Invasive Urothelial Carcinoma of the Bladder:
Post Hoc Analysis of Two Prospective Studies
Sung Wook Cho, Sung Hee Lim, Ghee Young Kwon, Chan Kyo Kim, Won Park, Hongryull Pyo, Jae Hoon Chung, Wan Song, Hyun Hwan Sung, Byong Chang Jeong, Se Hoon Park
Cancer Res Treat. 2024;56(3):893-897. doi: 10.4143/crt.2024.015.Development and Feasibility Evaluation of Smart Cancer Care 2.0 Based on Patient-Reported Outcomes for Post-Discharge Management of Patients with Cancer
Jin Ah Kwon, Songsoo Yang, Su-Jin Koh, Young Ju Noh, Dong Yoon Kang, Sol Bin Yang, Eun Ji Kwon, Jeong-Wook Seo, Jin Sung Kim, Minsu Ock
Cancer Res Treat. 2024;56(4):1040-1049. doi: 10.4143/crt.2024.003.Prognostic Significance of Bulky Nodal Disease in Anal Cancer Management: A Multi-institutional Study
Seok-Joo Chun, Eunji Kim, Won Il Jang, Mi-Sook Kim, Hyun-Cheol Kang, Byoung Hyuck Kim, Eui Kyu Chie
Cancer Res Treat. 2024;56(4):1197-1206. doi: 10.4143/crt.2024.258.The effects of sarcopenic obesity on immediate postoperative outcomes after pancreatoduodenectomy: a retrospective cohort study
Jae Hwan Jeong, Ji Su Kim, Seung-seob Kim, Seung Soo Hong, Ho Kyoung Hwang, Chang Moo Kang, Hyoung-Il Kim, Kyung Sik Kim, Sung Hyun Kim
Ann Surg Treat Res. 2024;107(4):203-211. doi: 10.4174/astr.2024.107.4.203.
Reference
-
References
1. Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Pineros M, et al. Global cancer observatory: cancer today [Internet]. Lyon: International Agency for Research on Cancer;2020. [cited 2022 Feb 13]. Available from: https://gco.iarc.fr/today .2. Bray F, Laversanne M, Weiderpass E, Soerjomataram I. The ever-increasing importance of cancer as a leading cause of premature death worldwide. Cancer. 2021; 127:3029–30.
Article3. Statistics Korea [Internet]. Daejeon: Statistics Korea;2020. [cited 2022 Feb 13]. Available from: http://kosis.kr .4. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999~2001; first result using the national cancer incidence database. Cancer Res Treat. 2005; 37:325–31.
Article5. Ajiki W, Tsukuma H, Oshima A. Index for evaluating completeness of registration in population-based cancer registries and estimation of registration rate at the Osaka Cancer Registry between 1966 and 1992 using this index. Nihon Koshu Eisei Zasshi. 1998; 45:1011–7.6. Fritz A, Percy C, Jack A, Shanmugaratnam K, Sobin L, Parkin DM, et al. International classification of diseases for oncology. 3rd ed 1st rev. Geneva: World Health Organization;2013.7. World Health Organization. International statistical classification of diseases and related health problems. 10th rev. Geneva: World Health Organization;1994.8. Ferlay J, Ervik M, Lam F, Colombet M, Mery L, Pineros M, et al. Global cancer observatory: cancer today – data and methods [Internet]. Lyon: International Agency for Research on Cancer;2020. [cited 2022 Feb 13]. Available from: https://gco.iarc.fr/today/data-sources-methods .9. Cancer incidence in five continents, XI Chapter 3 Classification and coding [Internet]. Lyon: International Agency for Research on Cancer;2020. [cited 2022 Feb 13]. Available from: http://ci5.iarc.fr/CI5-XI/Pages/Chapter3.aspx .10. Young JL Jr, Roffers SD, Ries LA, Fritz AG, Hurlbut AA. SEER summary staging manual 2000: codes and coding instructions. National Cancer Institute NIH Pub No 01-4969. Bethesda, MD: National Cancer Institute;2001.11. Cancer incidence in five continents, Vol XI Chapter 7 Age standardization [Internet]. Lyon: International Agency for Research on Cancer;2020. [cited 2022 Feb 13]. Available from: http://ci5.iarc.fr/CI5-XI/Pages/Chapter7.aspx .12. Segi M. Cancer mortality for selected sites in 24 countries 1950–1957. Sendai: Tohoku University School of Medicine;1960.13. Surveillance Research Program Joinpoint Regression Program, version 4801 [Internet]. Bethesda, MD: Surveillance Research Program, National Cancer Institute;2020. [cited 2022 Feb 13]. Available from: https://surveillance.cancer.gov/join-point/ .14. Ederer F, Heise H. Instructions to IBM 650 programmers in processing survival computations. Methodological note, No 10. Bethesda, MD: National Cancer Institute;1959.15. Paul Dickman [Internet]. Stockholm: PaulDickman.com;2016. [cited 2022 Feb 13]. Available from: http://www.pauldickman.com .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2016
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2008
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2018
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2020
- Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2014