J Korean Med Sci.
2022 Feb;37(6):e45. 10.3346/jkms.2022.37.e45.
Self-Injurious Behavior Rate in the Short-Term Period of the COVID-19 Pandemic in Korea
- Affiliations
-
- 1Department of Research Planning, Mental Health Research Institute, National Center for Mental Health, Seoul, Korea
- 2Mental Health Research Institute, National Center for Mental Health, Seoul, Korea
- KMID: 2526033
- DOI: http://doi.org/10.3346/jkms.2022.37.e45
Abstract
- Background
The objective of this study was to investigate the trend of self-injurious behavior (SIB) among persons who were directly impacted by coronavirus disease 2019 (COVID-19), especially those with pre-existing mental disorders.
Methods
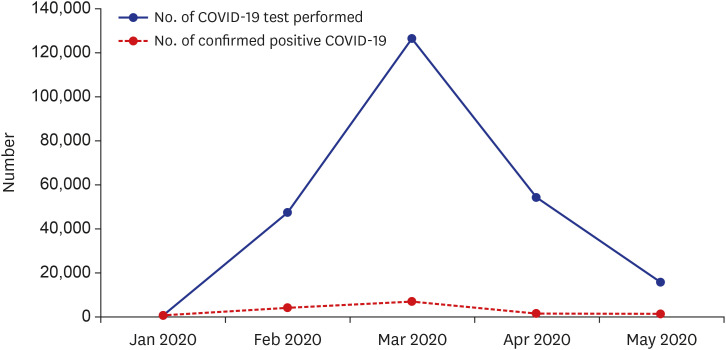
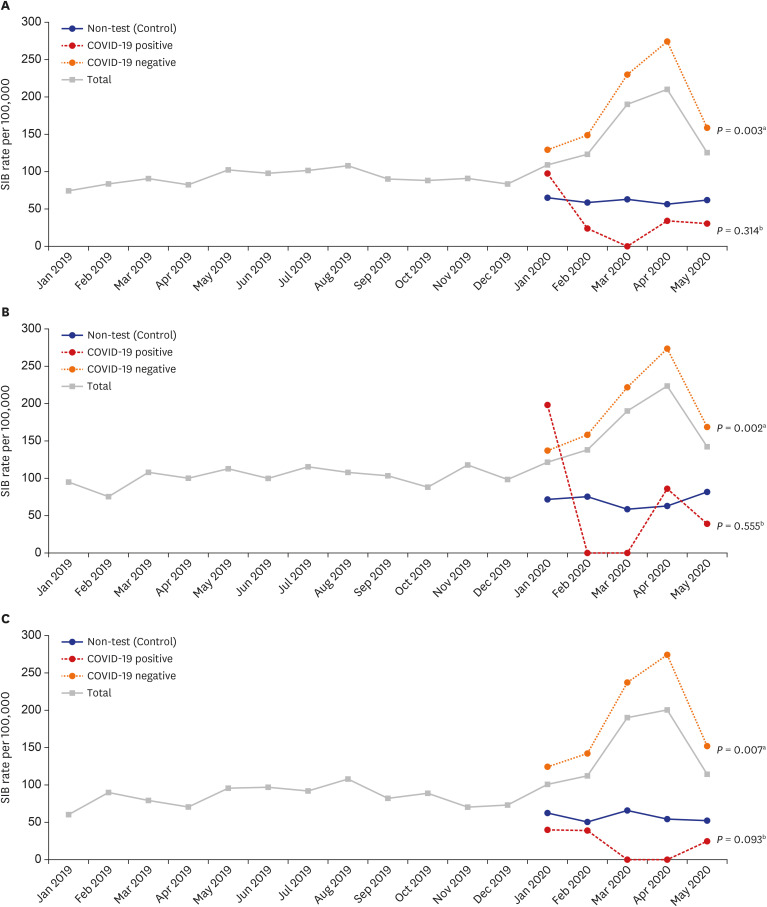
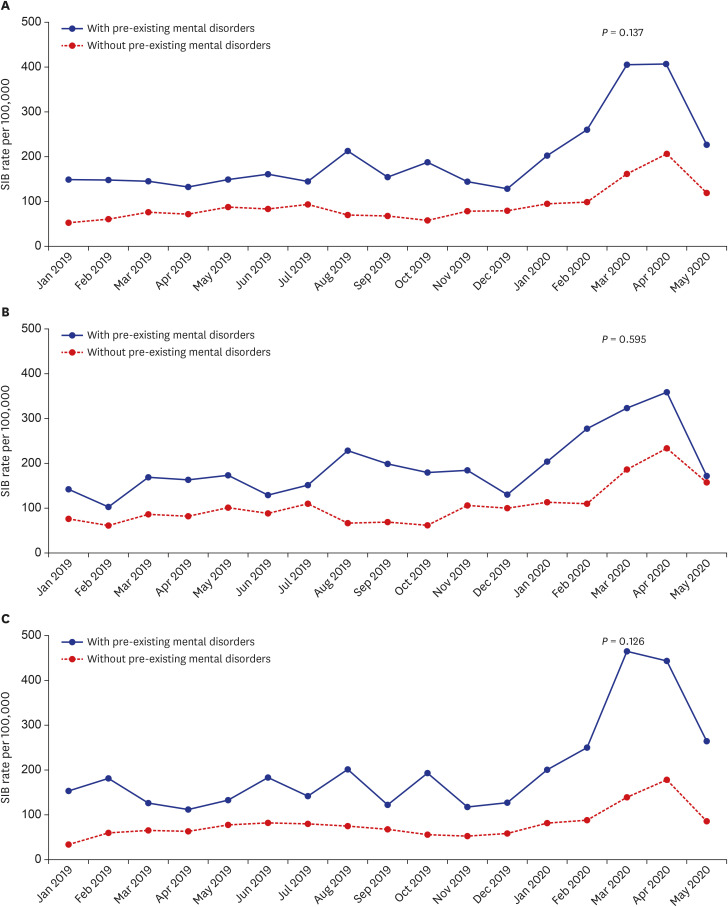
Using the National Health Insurance Service-COVID-19 database cohort, the monthly SIB rate was calculated by COVID-19 subgroups (i.e., positive for COVID-19 test, negative for COVID-19 test, and non-COVID-19 test [control]). In addition, moderated regression analysis was utilized to examine the statistical difference of SIB (suicide attempt and non-suicidal self-injury using ICD-10 code) trend between COVID-19 subgroups and with and without pre-existing mental disorder.
Results
A total of 328,373 persons were included in the cohort study. Of these, 212,678 had been tested for COVID-19, and 7,713 of them were confirmed positive. During the pandemic peak, the “negative for COVID-19” group showed a large increase (P = 0.003) in SIB rates compared to the control group, the “positive for COVID-19” group showed a decreasing trend, but not significant (P = 0.314). Among those who were tested for COVID-19, those with pre-existing mental disorders showed an increasing trend of SIB compared to those without pre-existing mental disorders, however statistically insignificant (P= 0.137).
Conclusion
Our results suggest that people who are tested for COVID-19 are at a high risk of SIB during the peak COVID-19 pandemic. Therefore, screening for suicide risk and psychological interventions is needed for these high-risk groups.
Keyword
Figure
Reference
-
1. Korea Disease Control and Prevention Agency. The updates on COVID-19 in Korea as of Feb 25. Updated 2021. Accessed May 7, 2021. https://www.kdca.go.kr/board/board.es?mid=a20501010000&bid=0015 .2. Park HY. Mental health in patients with coronavirus disease-19 and the quarantined people. J Korean Neuropsychiatr Assoc. 2021; 60(1):11–18.3. Park SC, Park YC. Secondary emotional reactions to the COVID-19 outbreak should be identified and treated in Korea. J Korean Med Sci. 2020; 35(17):e161. PMID: 32356422.4. Jung SJ, Jun JY. Mental health and psychological intervention amid COVID-19 outbreak: perspectives from South Korea. Yonsei Med J. 2020; 61(4):271–272. PMID: 32233168.5. Lee HS, Dean D, Baxter T, Griffith T, Park S. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. 2021; 295:113570. PMID: 33234326.6. Cheng SK, Tsang JS, Ku KH, Wong CW, Ng YK. Psychiatric complications in patients with severe acute respiratory syndrome (SARS) during the acute treatment phase: a series of 10 cases. Br J Psychiatry. 2004; 184(4):359–360. PMID: 15056583.7. Chua SE, Cheung V, McAlonan GM, Cheung C, Wong JW, Cheung EP, et al. Stress and psychological impact on SARS patients during the outbreak. Can J Psychiatry. 2004; 49(6):385–390. PMID: 15283533.8. Jalloh MF, Li W, Bunnell RE, Ethier KA, O'Leary A, Hageman KM, et al. Impact of Ebola experiences and risk perceptions on mental health in Sierra Leone, July 2015. BMJ Glob Health. 2018; 3(2):e000471.9. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004; 10(7):1206–1212. PMID: 15324539.10. Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020; 7(6):468–471. PMID: 32330430.11. Ozili PK. COVID-19 pandemic and economic crisis: the Nigerian experience and structural causes. J Econ Adm Sci. 2021; 37(4):401–418.12. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiatry. 2020; 77(11):1093–1094. PMID: 32275300.13. Kim AM. The short-term impact of the COVID-19 outbreak on suicides in Korea. Psychiatry Res. 2021; 295:113632. PMID: 33338860.14. Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open. 2021; 4(2):e2037378. PMID: 33528554.15. Leske S, Kõlves K, Crompton D, Arensman E, de Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. 2021; 8(1):58–63. PMID: 33212023.16. Knudsen AKS, Stene-Larsen K, Gustavson K, Hotopf M, Kessler RC, Krokstad S, et al. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Reg Health Eur. 2021; 4:100071. PMID: 34557811.17. Pirkis J, John A, Shin S, DelPozo-Banos M, Arya V, Analuisa-Aguilar P, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. 2021; 8(7):579–588. PMID: 33862016.18. Radeloff D, Papsdorf R, Uhlig K, Vasilache A, Putnam K, von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. 2021; 30:e16. PMID: 33461639.19. Hyun J, You S, Sohn S, Kim SJ, Bae J, Baik M, et al. Psychosocial support during the COVID-19 outbreak in Korea: activities of multidisciplinary mental health professionals. J Korean Med Sci. 2020; 35(22):e211. PMID: 32508070.20. Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. 2020; 177(7):574–575. PMID: 32375540.21. Druss BG. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020; 77(9):891–892. PMID: 32242888.22. Wolff J, Frazier EA, Esposito-Smythers C, Burke T, Sloan E, Spirito A. Cognitive and social factors associated with NSSI and suicide attempts in psychiatrically hospitalized adolescents. J Abnorm Child Psychol. 2013; 41(6):1005–1013. PMID: 23588400.23. Cooper J, Kapur N, Webb R, Lawlor M, Guthrie E, Mackway-Jones K, et al. Suicide after deliberate self-harm: a 4-year cohort study. Am J Psychiatry. 2005; 162(2):297–303. PMID: 15677594.24. Kim H, Kim Y, Shin MH, Choi KW, Chung MK, Jeon HJ. Risk of suicide attempt after thyroidectomy: a nationwide population study in South Korea. Psychiatry Investig. 2021; 18(1):39–47.25. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020; 395(10227):912–920. PMID: 32112714.26. Jung SJ, Lim SS, Yoon JH. Fluctuations in influenza-like illness epidemics and suicide mortality: a time-series regression of 13-year mortality data in South Korea. PLoS One. 2021; 16(2):e0244596. PMID: 33577567.27. COVID-19 National Emergency Response Center, Epidemiology & Case Management Team, Korea Centers for Disease Control & Prevention. Contact transmission of COVID-19 in South Korea: novel investigation techniques for tracing contacts. Osong Public Health Res Perspect. 2020; 11(1):60–63. PMID: 32149043.28. Kang E, Lee SY, Kim MS, Jung H, Kim KH, Kim KN, et al. The psychological burden of COVID-19 stigma: evaluation of the mental health of isolated mild condition COVID-19 patients. J Korean Med Sci. 2021; 36(3):e33. PMID: 33463098.29. Lee JH, Lee D, Hyun S, Hong JS, Kim CH, Kim W, et al. Online mental health assessments of COVID-19 patients in South Korea. Front Psychiatry. 2021; 12:685445. PMID: 34295275.30. Park HY, Park WB, Lee SH, Kim JL, Lee JJ, Lee H, et al. Posttraumatic stress disorder and depression of survivors 12 months after the outbreak of Middle East respiratory syndrome in South Korea. BMC Public Health. 2020; 20(1):605. PMID: 32410603.31. Hao F, Tan W, Jiang L, Zhang L, Zhao X, Zou Y, et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav Immun. 2020; 87:100–106. PMID: 32353518.32. Jung J. A long way to the recovery: COVID-19 will not disappear. J Korean Med Sci. 2021; 36(32):e231. PMID: 34402229.33. Ko M, Cho HM, Park J, Chi S, Han C, Yi HS, et al. Impact of the coronavirus disease pandemic on mental health among local residents in Korea: a cross sectional study. J Korean Med Sci. 2021; 36(46):e322. PMID: 34845878.34. Jang OJ, Chung YI, Lee JW, Kim HC, Seo JS. Emotional distress of the COVID-19 cluster infection on health care workers working at a national hospital in Korea. J Korean Med Sci. 2021; 36(47):e324. PMID: 34873887.35. Ju G, Lee J, Ahn MH, Lee J, Kim EJ, Suh S, et al. Effects of depression and resilience of public workers on work-related stress and anxiety in response to the COVID-19 pandemic. J Korean Med Sci. 2021; 36(36):e262. PMID: 34519189.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The COVID-19 pandemic's impact on prostate cancer screening and diagnosis in Korea
- The Management of Thyroid Disease in COVID-19 Pandemic
- Factors Influencing Changes in Parenting Behavior during Coronavirus Disease 2019 Pandemic
- Short-Term Impact of Temporary Shutdown of a University-Affiliated Hospital on Patients With Colorectal Cancer During the Coronavirus Disease 2019 Pandemic
- The coronavirus disease 2019 pandemic and chronic diseases