Kosin Med J.
2023 Sep;38(3):193-200. 10.7180/kmj.23.116.
The COVID-19 pandemic's impact on prostate cancer screening and diagnosis in Korea
- KMID: 2546154
- DOI: http://doi.org/10.7180/kmj.23.116
Abstract
- Background
The global coronavirus disease 2019 (COVID-19) pandemic, which started in early 2020, has had multiple impacts on cancer care. This study assessed how the COVID-19 pandemic influenced prostate cancer (PCa) screening and diagnosis in South Korea.
Methods
Patients who visited the outpatient clinic at a single institution for PCa evaluation were included in this study and divided into a pre-COVID-19 group and a COVID-19 pandemic group, based on the start of the COVID-19 pandemic and social distancing policies on March 1, 2020. The number of prostate-specific antigen (PSA) tests, patients with elevated PSA levels, and prostate biopsy results were analyzed.
Results
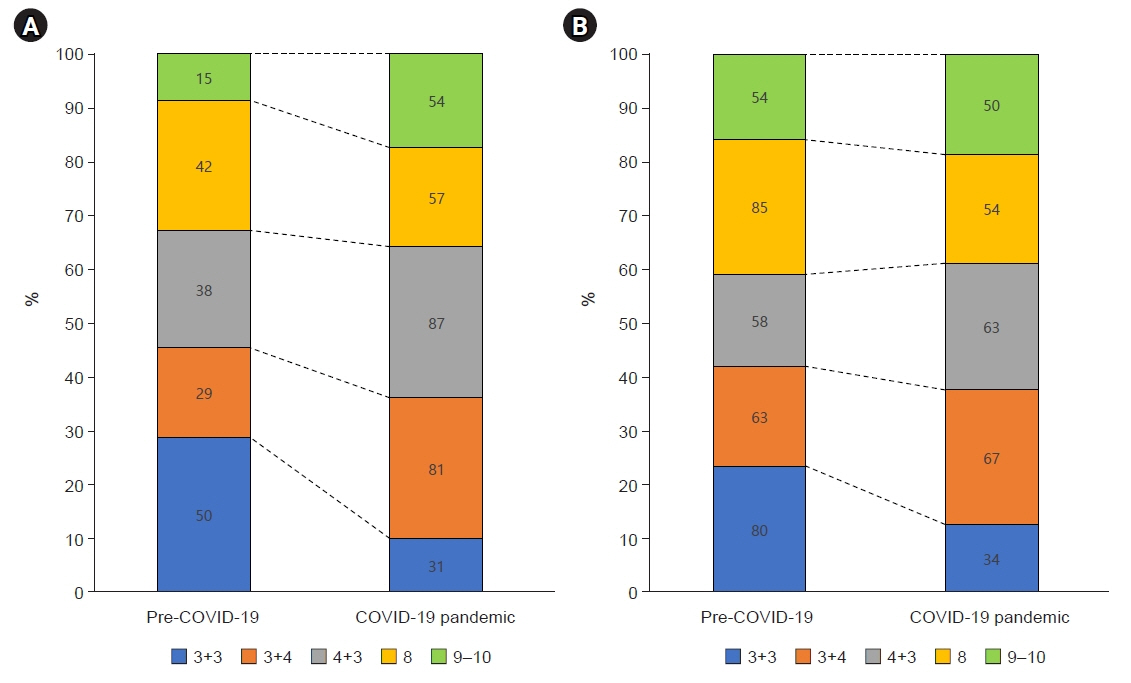
In total, 8,926 PSA tests were administered during the COVID-19 pandemic, compared to 15,654 before the pandemic (p<0.05). Of 2,132 patients with high PSA levels, 1,055 (49.5%) received prostate biopsies before the pandemic and 1,077 (50.5%) did so during the COVID-19 pandemic. The COVID-19 pandemic group had a higher detection rate of PC, and increased rates of Gleason scores (GS) 7 and 9–10, while the rate of GS 6 decreased compared to the pre-COVID-19 group (p<0.05). The rate of clinically significant PCa (csPCa) was also higher during the pandemic (p<0.05). In both magnetic resonance imaging-guided and standard biopsies, the GS 6 rate decreased, and the csPCa rate increased during the COVID-19 pandemic (each, p<0.05).
Conclusions
During the COVID-19 pandemic, the detection rate of prostate biopsies and the rate of csPCa increased significantly. Thus, PCa was diagnosed at a more advanced state in Korea during the COVID-19 pandemic.
Figure
Reference
-
References
1. Lim JH, Lee WY, Yun SH, Kim HC, Cho YB, Huh JW, et al. Has the COVID-19 pandemic caused upshifting in colorectal cancer stage? Ann Coloproctol. 2021; 37:253–8.
Article2. Ko HJ, Cho YJ, Kim KK, Kang JH, Kim YS, Haam JH, et al. COVID-19 and related social distancing measures induce significant metabolic complications without prominent weight gain in Korean adults. Front Med (Lausanne). 2022; 9:951793.
Article3. London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C. Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform. 2020; 4:657–65.
Article4. Kaufman HW, Chen Z, Niles J, Fesko Y. Changes in the number of US patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open. 2020; 3:e2017267.
Article5. Lee KM, Bryant AK, Alba P, Anglin T, Robison B, Rose BS, et al. Impact of COVID-19 on the incidence of localized and metastatic prostate cancer among White and Black Veterans. Cancer Med. 2023; 12:3727–30.6. Englum BR, Prasad NK, Lake RE, Mayorga-Carlin M, Turner DJ, Siddiqui T, et al. Impact of the COVID-19 pandemic on diagnosis of new cancers: a national multicenter study of the Veterans Affairs Healthcare System. Cancer. 2022; 128:1048–56.
Article7. Chen RC, Haynes K, Du S, Barron J, Katz AJ. Association of cancer screening deficit in the United States with the COVID-19 pandemic. JAMA Oncol. 2021; 7:878–84.
Article8. Nyk L, Kamecki H, Zagozdzon B, Tokarczyk A, Baranek P, Mielczarek L, et al. The impact of the ongoing COVID-19 epidemic on the increasing risk of adverse pathology in prostate cancer patients undergoing radical prostatectomy. Curr Oncol. 2022; 29:2768–75.
Article9. Deukeren DV, Heesterman BL, Roelofs L, Kiemeney LA, Witjes JA, Smilde TJ, et al. Impact of the COVID-19 outbreak on prostate cancer care in the Netherlands. Cancer Treat Res Commun. 2022; 31:100553.
Article10. Jain A, Macneil J, Kim L, Patel MI. The effect of COVID-19 on prostate cancer testing in Australia. BMC Urol. 2022; 22:88.
Article11. Fallara G, Sandin F, Styrke J, Carlsson S, Lissbrant IF, Ahlgren J, et al. Prostate cancer diagnosis, staging, and treatment in Sweden during the first phase of the COVID-19 pandemic. Scand J Urol. 2021; 55:184–91.
Article12. Kang YJ, Baek JM, Kim YS, Jeon YW, Yoo TK, Rhu J, et al. Impact of the COVID-19 pandemic on the diagnosis and surgery of breast cancer: a multi-institutional study. J Breast Cancer. 2021; 24:491–503.
Article13. Huang GL, Kang CH, Lee WC, Chiang PH. Comparisons of cancer detection rate and complications between transrectal and transperineal prostate biopsy approaches: a single center preliminary study. BMC Urol. 2019; 19:101.14. Kortenbach KC, Logager V, Thomsen HS, Boesen L. Comparison of PSA density and lesion volume strategies for selecting men with equivocal PI-RADS 3 lesions on bpMRI for biopsies. Abdom Radiol (NY). 2023; 48:688–93.
Article15. Yarlagadda VK, Lai WS, Gordetsky JB, Porter KK, Nix JW, Thomas JV, et al. MRI/US fusion-guided prostate biopsy allows for equivalent cancer detection with significantly fewer needle cores in biopsy-naive men. Diagn Interv Radiol. 2018; 24:115–20.
Article16. Wiener S, Haddock P, Cusano J, Staff I, McLaughlin T, Wagner J. Incidence of clinically significant prostate cancer after a diagnosis of atypical small acinar proliferation, high-grade prostatic intraepithelial neoplasia, or benign tissue. Urology. 2017; 110:161–5.
Article17. National Cancer Center (NCC). Annual report of cancer statistics in Korea in 2020 [Internet]. NCC;c2020. [cited 2023 Jun 18]. https://ncc.re.kr/cancerStatsView.ncc?bbsnum=638&searchKey=total&searchValue=&pageNum=1.18. Mottet N, van den Bergh RC, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, et al. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol. 2021; 79:243–62.19. Diamand R, Ploussard G, Roumiguie M, Oderda M, Benamran D, Fiard G, et al. Timing and delay of radical prostatectomy do not lead to adverse oncologic outcomes: results from a large European cohort at the times of COVID-19 pandemic. World J Urol. 2021; 39:1789–96.
Article20. Moyer VA; U.S. Preventive Services Task Force. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012; 157:120–34.
Article21. Burgess L, Aldrighetti CM, Ghosh A, Niemierko A, Chino F, Huynh MJ, et al. Association of the USPSTF grade D recommendation against prostate-specific antigen screening with prostate cancer-specific mortality. JAMA Netw Open. 2022; 5:e2211869.
Article22. Butler SS, Muralidhar V, Zhao SG, Sanford NN, Franco I, Fullerton ZH, et al. Prostate cancer incidence across stage, NCCN risk groups, and age before and after USPSTF Grade D recommendations against prostate-specific antigen screening in 2012. Cancer. 2020; 126:717–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of the COVID-19 Pandemic on Gastric Cancer Screening in South Korea: Results From the Korean National Cancer Screening Survey (2017–2021)
- Changes in cancer screening before and during COVID‐19: findings from the Korean National Cancer Screening Survey 2019 and 2020
- The coronavirus disease 2019 pandemic and chronic diseases
- The impact of COVID-19 on screening for colorectal, gastric, breast, and cervical cancer in Korea
- Influence of the COVID-19 Pandemic on the Treatment Patterns and Outcomes of Colorectal Cancer