Ann Surg Treat Res.
2022 Feb;102(2):65-72. 10.4174/astr.2022.102.2.65.
In vivo study for the hemostatic efficacy and foreign body reaction of a new powder-type polysaccharide hemostatic agent
- Affiliations
-
- 1Department of Surgery, Uijeongbu Eulji Medical Center, Eulji University School of Medicine, Uijeongbu, Korea
- 2Theracion Biomedical Co., Ltd., Seongnam, Korea
- 3Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 4Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2525443
- DOI: http://doi.org/10.4174/astr.2022.102.2.65
Abstract
- Purpose
Various hemostatic agents have been introduced in therapy as postoperative bleeding is a poor prognostic factor for postoperative outcomes. These products can be divided into those that directly promote the hemostatic cascade and those that physically form a barrier by absorbing blood. The latter, powder-type hemostatic agents have the advantages of being inexpensive and more absorbable with less foreign body reactions (FBRs) and are applicable to a relatively wide area. This study was conducted to verify the safety and efficacy of a newly invented polysaccharide product (OOZFIX, Theracion Biomedical), which improves blood absorption and hemostatic effects.
Methods
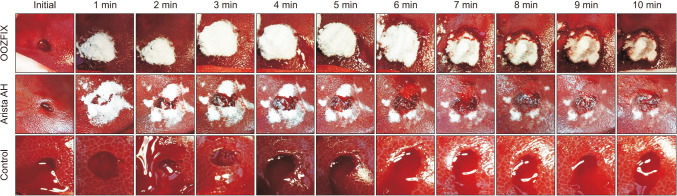
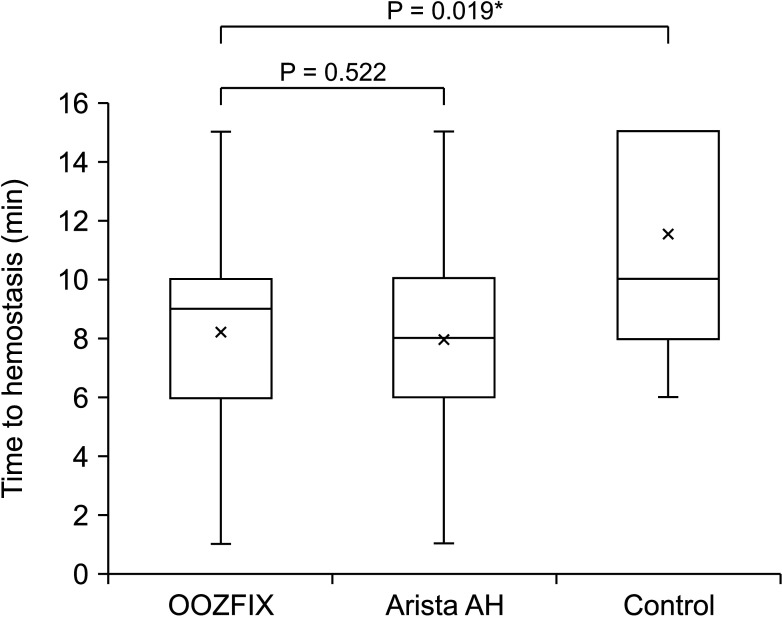
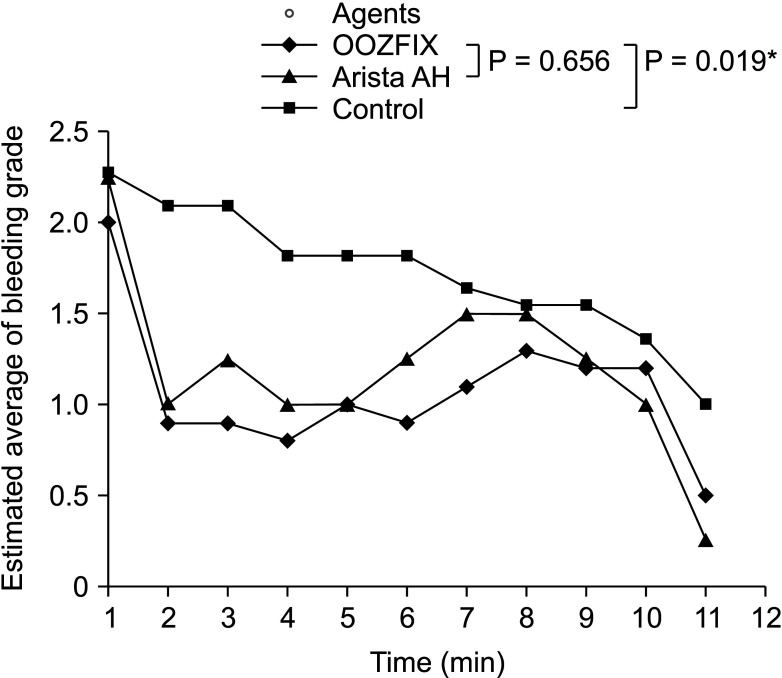
Two separate animal experiments were performed. The first evaluated FBRs histologically at 3 days, 2 weeks, and 4 weeks, after implantation of OOZFIX in rats, and the second compared hemostatic performance of OOZFIX and Arista AH (Bard) in the porcine liver punch biopsy model.
Results
We found minimal FBRs in the 3-day group and no reactions in both the 2-week and 4-week groups after implantation of hemostatic agents. The time to hemostasis of OOZFIX was not significantly different from that of Arista AH (median [interquartile range]: 9 [6–10] minutes vs. 8 [6–10] minutes, respectively; P = 0.522). When comparing the serial bleeding grade tendency, there was no statistical difference between OOZFIX and Arista AH (P = 0.656).
Conclusion
OOZFIX caused a minimal FBR that disappeared within 2 weeks in vivo, and its hemostatic performance was comparable with that of an existing agent, Arista AH. Further clinical studies are required in the future.
Keyword
Figure
Reference
-
1. Montán C, Wannberg M, Holst J, Wahlgren CM. Perioperative haemorrhage in endovascular abdominal aneurysm repair affects outcome. Eur J Vasc Endovasc Surg. 2013; 46:87–92. PMID: 23582344.
Article2. Hachem LD, Ghanekar A, Selzner M, Famure O, Li Y, Kim SJ. Postoperative surgical-site hemorrhage after kidney transplantation: incidence, risk factors, and outcomes. Transpl Int. 2017; 30:474–483. PMID: 28120465.
Article3. Schrem H, Klußmann A, Focken M, Emmanouilidis N, Oldhafer F, Klempnauer J, et al. Post-operative hemorrhage after liver transplantation: risk factors and long-term outcome. Ann Transplant. 2016; 21:46–55. PMID: 26818716.
Article4. Shah A, Palmer AJ, Klein AA. Strategies to minimize intraoperative blood loss during major surgery. Br J Surg. 2020; 107:e26–e38. PMID: 31903592.
Article5. Seyednejad H, Imani M, Jamieson T, Seifalian AM. Topical haemostatic agents. Br J Surg. 2008; 95:1197–1225. PMID: 18763249.
Article6. Boonstra EA, Molenaar IQ, Porte RJ, de Boer MT. Topical haemostatic agents in liver surgery: do we need them? HPB (Oxford). 2009; 11:306–310. PMID: 19718357.
Article7. Brustia R, Granger B, Scatton O. An update on topical haemostatic agents in liver surgery: systematic review and meta analysis. J Hepatobiliary Pancreat Sci. 2016; 23:609–621. PMID: 27580747.
Article8. Lewis KM, Atlee HD, Mannone AJ, Dwyer J, Lin L, Goppelt A, et al. Comparison of two gelatin and thrombin combination hemostats in a porcine liver abrasion model. J Invest Surg. 2013; 26:141–148. PMID: 23514063.
Article9. Singh RK, Baumgartner B, Mantei JR, Parreno RN, Sanders PJ, Lewis KM, et al. Hemostatic comparison of a polysaccharide powder and a gelatin powder. J Invest Surg. 2019; 32:393–401. PMID: 29420097.
Article10. MacDonald MH, Wang AY, Clymer JW, Hutchinson RW, Kocharian R. An in vivo comparison of the efficacy of hemostatic powders, using two porcine bleeding models. Med Devices (Auckl). 2017; 10:273–279. PMID: 29238233.11. Lewis KM, Li Q, Jones DS, Corrales JD, Du H, Spiess PE, et al. Development and validation of an intraoperative bleeding severity scale for use in clinical studies of hemostatic agents. Surgery. 2017; 161:771–781. PMID: 27839931.
Article12. Rosselli DD, Brainard BM, Schmiedt CW. Efficacy of a topical bovine-derived thrombin solution as a hemostatic agent in a rodent model of hepatic injury. Can J Vet Res. 2015; 79:303–308. PMID: 26424911.13. Franceschini G. Internal surgical use of biodegradable carbohydrate polymers. Warning for a conscious and proper use of oxidized regenerated cellulose. Carbohydr Polym. 2019; 216:213–216. PMID: 31047059.
Article14. Yang YL, Zhang C, Zhang HW, Wu P, Ma YF, Lin MJ, et al. Common bile duct injury by fibrin glue: report of a rare complication. World J Gastroenterol. 2015; 21:2854–2857. PMID: 25759561.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biologic response of local hemostatic agents used in endodontic microsurgery
- Wound healing effect of regenerated oxidized cellulose versus fibrin sealant patch: An in vivo study
- Endoscopic Hemostatic Treatment of Peptic Ulcer Bleeding
- Difference in Bonding Strength of RMGIC according to Type of Hemostatic Agent in Primary Tooth
- Efficacy of Intra-Articular Injection of Thrombin-Based Hemostatic Agent in the Control of Bleeding after Primary Total Knee Arthroplasty