J Korean Assoc Oral Maxillofac Surg.
2021 Dec;47(6):480-483. 10.5125/jkaoms.2021.47.6.480.
Autologous blood derived cell therapy in maxillofacial bone graft surgery
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital, School of Dentistry, Seoul National University, Seoul, Korea
- KMID: 2524709
- DOI: http://doi.org/10.5125/jkaoms.2021.47.6.480
Abstract
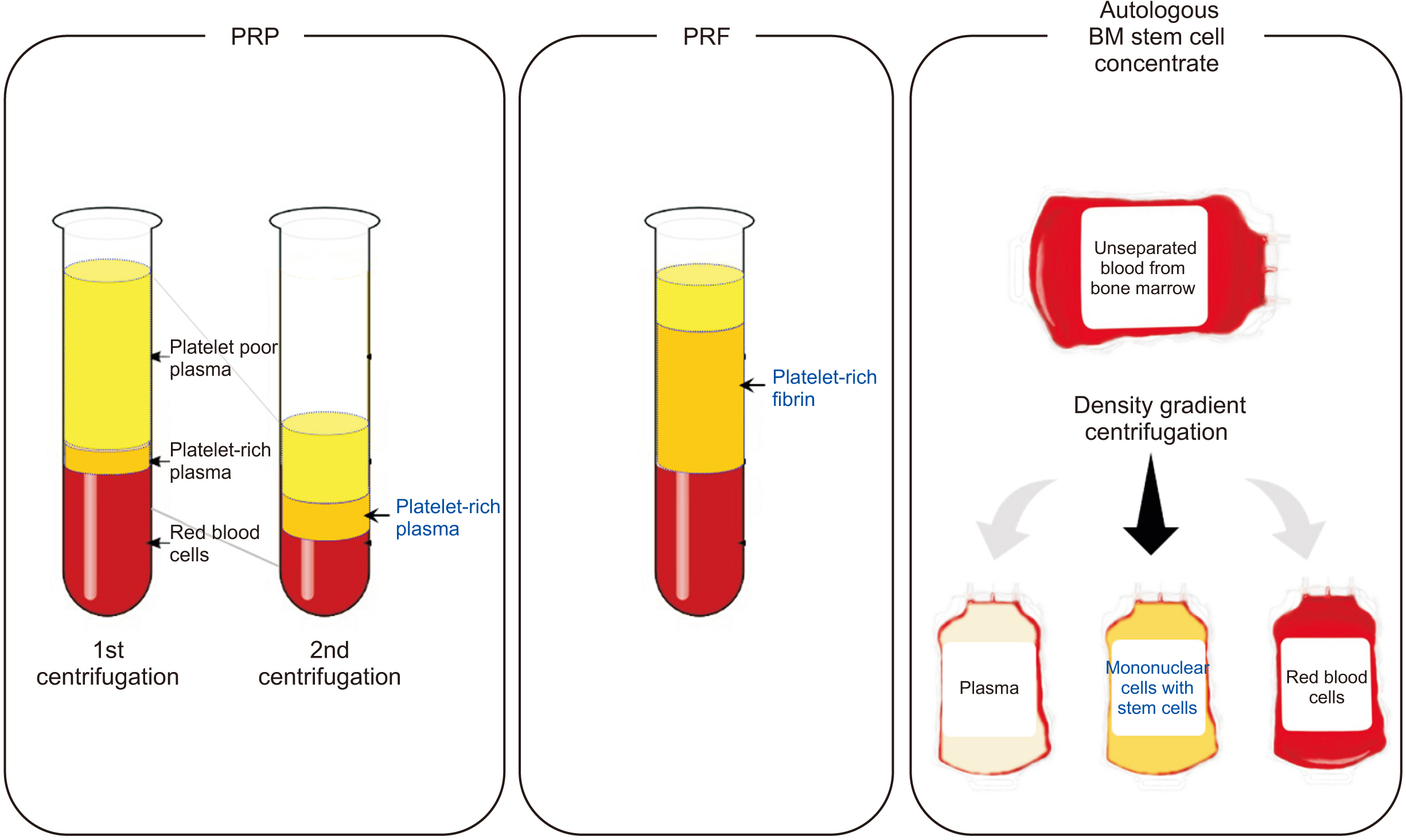
- Tissue regeneration is one of the ultimate goals of maxillofacial surgery and various types of tissue engineering technologies have been utilized in clinics. Healthy resources of host cells and growth factors are essential for the tissue engineering, therefore autologous blood-derived cell therapy was introduced. In this article, clinical applications of the autologous platelet concentrates and stem cell separation therapy will be summarized and evaluated for their efficacy and feasibility in the current maxillofacial clinics.
Keyword
Figure
Reference
-
References
1. Ceccarelli G, Presta R, Benedetti L, Cusella De Angelis MG, Lupi SM. Rodriguez Y Baena R. 2017; Emerging perspectives in scaffold for tissue engineering in oral surgery. Stem Cells Int. 2017:4585401. https://doi.org/10.1155/2017/4585401. DOI: 10.1155/2017/4585401. PMID: 28337223. PMCID: PMC5346390.
Article2. Doonquah L, Holmes PJ, Ranganathan LK, Robertson H. 2021; Bone grafting for implant surgery. Oral Maxillofac Surg Clin North Am. 33:211–29. https://doi.org/10.1016/j.coms.2021.01.006. DOI: 10.1016/j.coms.2021.01.006. PMID: 33750652.
Article3. Rakhmatia YD, Ayukawa Y, Furuhashi A, Koyano K. 2013; Current barrier membranes: titanium mesh and other membranes for guided bone regeneration in dental applications. J Prosthodont Res. 57:3–14. https://doi.org/10.1016/j.jpor.2012.12.001. DOI: 10.1016/j.jpor.2012.12.001. PMID: 23347794.
Article4. Zhao R, Yang R, Cooper PR, Khurshid Z, Shavandi A, Ratnayake J. 2021; Bone grafts and substitutes in dentistry: a review of current trends and developments. Molecules. 26:3007. https://doi.org/10.3390/molecules26103007. DOI: 10.3390/molecules26103007. PMID: 34070157. PMCID: PMC8158510.
Article5. Masoudi E, Ribas J, Kaushik G, Leijten J, Khademhosseini A. 2016; Platelet-rich blood derivatives for stem cell-based tissue engineering and regeneration. Curr Stem Cell Rep. 2:33–42. https://doi.org/10.1007/s40778-016-0034-8. DOI: 10.1007/s40778-016-0034-8. PMID: 27047733. PMCID: PMC4817373.
Article6. Marx RE. 2004; Platelet-rich plasma: evidence to support its use. J Oral Maxillofac Surg. 62:489–96. https://doi.org/10.1016/j.joms.2003.12.003. DOI: 10.1016/j.joms.2003.12.003. PMID: 15085519.
Article7. Marx RE, Carlson ER, Eichstaedt RM, Schimmele SR, Strauss JE, Georgeff KR. 1998; Platelet-rich plasma: growth factor enhancement for bone grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 85:638–46. https://doi.org/10.1016/s1079-2104(98)90029-4. DOI: 10.1016/S1079-2104(98)90029-4.
Article8. Xu J, Gou L, Zhang P, Li H, Qiu S. 2020; Platelet-rich plasma and regenerative dentistry. Aust Dent J. 65:131–42. https://doi.org/10.1111/adj.12754. DOI: 10.1111/adj.12754. PMID: 32145082. PMCID: PMC7384010.
Article9. Miron RJ, Fujioka-Kobayashi M, Bishara M, Zhang Y, Hernandez M, Choukroun J. 2017; Platelet-rich fibrin and soft tissue wound healing: a systematic review. Tissue Eng Part B Rev. 23:83–99. https://doi.org/10.1089/ten.TEB.2016.0233. DOI: 10.1089/ten.teb.2016.0233. PMID: 27672729.
Article10. Miron RJ, Zucchelli G, Pikos MA, Salama M, Lee S, Guillemette V, et al. 2017; Use of platelet-rich fibrin in regenerative dentistry: a systematic review. Clin Oral Investig. 21:1913–27. https://doi.org/10.1007/s00784-017-2133-z. DOI: 10.1007/s00784-017-2133-z. PMID: 28551729.
Article11. Naik B, Karunakar P, Jayadev M, Marshal VR. 2013; Role of platelet rich fibrin in wound healing: a critical review. J Conserv Dent. 16:284–93. https://doi.org/10.4103/0972-0707.114344. DOI: 10.4103/0972-0707.114344. PMID: 23956527. PMCID: PMC3740636.
Article12. Strauer BE, Brehm M, Zeus T, Gattermann N, Hernandez A, Sorg RV, et al. 2001; [Intracoronary, human autologous stem cell transplantation for myocardial regeneration following myocardial infarction]. Dtsch Med Wochenschr. 126:932–8. German. https://doi.org/10.1055/s-2001-16579-2. DOI: 10.1055/s-2001-16579-2. PMID: 11523014.
Article13. Aktas M, Radke TF, Strauer BE, Wernet P, Kogler G. 2008; Separation of adult bone marrow mononuclear cells using the automated closed separation system Sepax. Cytotherapy. 10:203–11. https://doi.org/10.1080/14653240701851324. DOI: 10.1080/14653240701851324. PMID: 18368599.
Article14. Güven S, Karagianni M, Schwalbe M, Schreiner S, Farhadi J, Bula S, et al. 2012; Validation of an automated procedure to isolate human adipose tissue-derived cells by using the Sepax® technology. Tissue Eng Part C Methods. 18:575–82. https://doi.org/10.1089/ten.TEC.2011.0617. DOI: 10.1089/ten.tec.2011.0617. PMID: 22372873. PMCID: PMC3401386.
Article15. Mazzanti B, Urbani S, Dal Pozzo S, Bufano P, Ballerini L, Gelli A, et al. 2017; Fully automated, clinical-grade bone marrow processing: a single-centre experience. Blood Transfus. 15:577–84. https://doi.org/10.2450/2016.0057-16. DOI: 10.2450/2016.0057-16.
Article16. Kobayashi E, Flückiger L, Fujioka-Kobayashi M, Sawada K, Sculean A, Schaller B, et al. 2016; Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin Oral Investig. 20:2353–60. https://doi.org/10.1007/s00784-016-1719-1. DOI: 10.1007/s00784-016-1719-1. PMID: 26809431.
Article17. Cruz-Barrera M, Flórez-Zapata N, Lemus-Diaz N, Medina C, Galindo CC, González-Acero LX, et al. 2020; Integrated analysis of transcriptome and secretome from umbilical cord mesenchymal stromal cells reveal new mechanisms for the modulation of inflammation and immune activation. Front Immunol. 11:575488. https://doi.org/10.3389/fimmu.2020.575488. DOI: 10.3389/fimmu.2020.575488. PMID: 33117373. PMCID: PMC7561386.
Article18. Li C, Li J, Li Y, Lang S, Yougbare I, Zhu G, et al. 2012; Crosstalk between platelets and the immune system: old systems with new discoveries. Adv Hematol. 2012:384685. https://doi.org/10.1155/2012/384685. DOI: 10.1155/2012/384685. PMID: 23008717. PMCID: PMC3447344.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Platelet-rich Plasma
- The reconstruction of posttraumatic craniofacial deformity using modified lefort II and III osteotomy and autogenous iliac bone graft
- Comparison of vertical bone resorption following various types of autologous block bone grafts
- Tissue Engineering of Vascular Graft Using Autogenous Bone Marrow Cell and Allogenous Acellular Vessel
- Temporomandibular joint re-ankylosis: a case report and literature review