First Course of treatment and Prognosis of Exocrine Pancreatic Cancer in Korea from 2006 to 2017
- Affiliations
-
- 1Center for Liver and Pancreatobiliary Cancer, National Cancer Center, Goyang, Korea
- 2Division of Cancer Registration and Surveillance, National Cancer Center, Goyang, Korea
- 3Department of Cancer Control & Population Health, Graduate School of Cancer Science and Policy, National Cancer Center, Goyang, Korea
- KMID: 2524601
- DOI: http://doi.org/10.4143/crt.2021.421
Abstract
- Purpose
Hospital-based clinical studies have limitations in holistic assessment of cancer treatment and prognosis, as they omit out-of-hospital patients including elderly individuals. This study aimed to investigate trends in initial treatment and corresponding prognosis of patients with exocrine pancreatic cancer (EPC) in Korea.
Materials and Methods
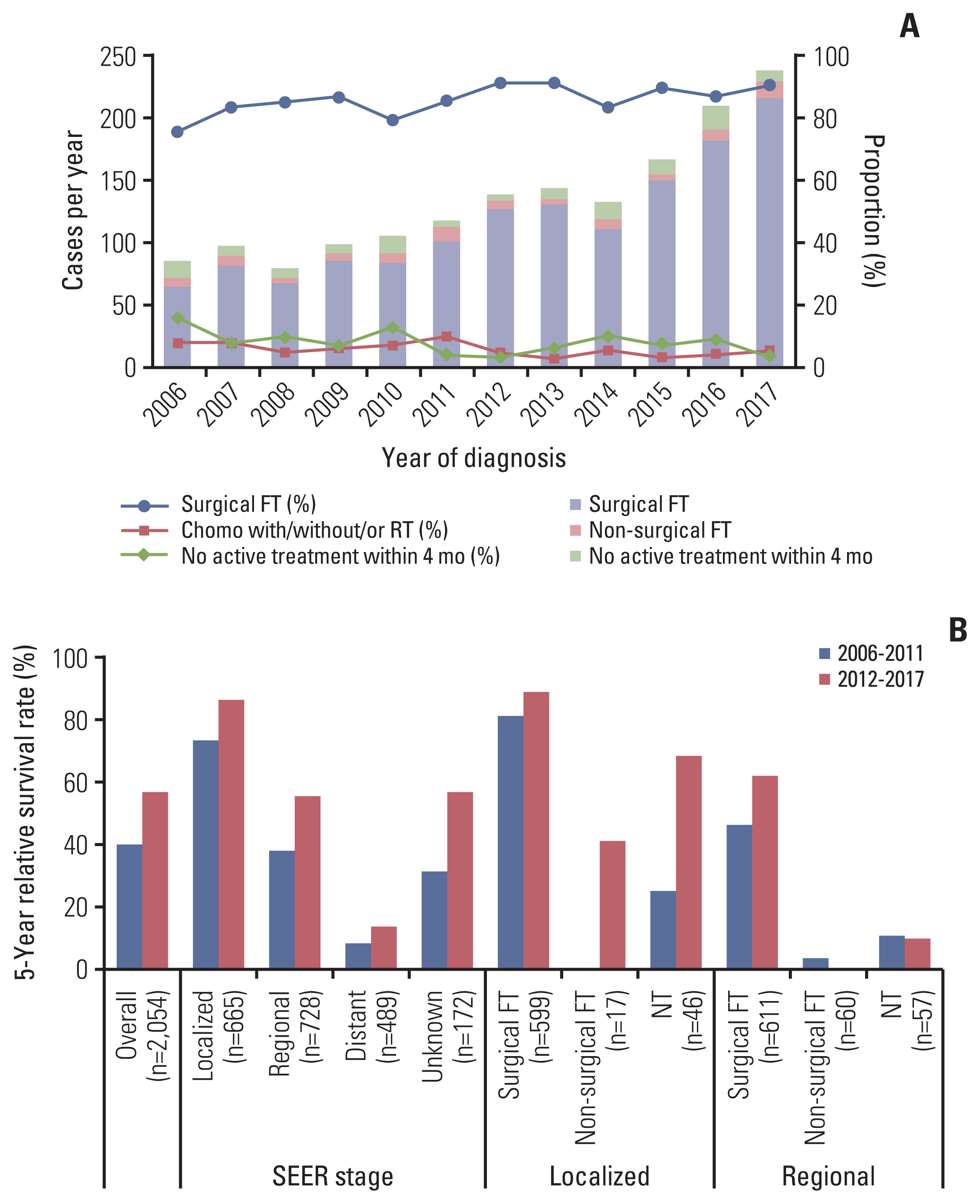
The Korea Central Cancer Registry data of patients with EPC from 2006 to 2017 were retrospectively reviewed. We defined the first course of treatment (FT) as the cancer-directed treatment administered within four months after cancer diagnosis according to Surveillance, Epidemiology, and End Results (SEER) program.
Results
Among 62,209 patients with EPC, localized and regional (LR) SEER stage; patients over 70 years old; and ductal adenocarcinoma excluding cystic or mucinous (DAC) accounted for 40.6%, 50.1%, and 95.9%, respectively. “No active treatment” (NT, 46.5%) was the most frequent, followed by non-surgical FT (28.7%) and surgical FT (22.0%). Among 25,198 patients with LR EPC, surgical FT increased (35.9% to 46.3%) and NT decreased (45.0% to 29.5%) from 2006 to 2017. The rate of surgical FT was inversely related to age (55.1% [< 70 years], 37.3% [70-79 years], 10.9% [≥ 80 years]). Five-year relative survival rates of LR DAC were higher after surgical FT than after NT in localized (46.1% vs. 12.9%) and regional stage (23.6% vs. 4.9%) from 2012 to 2017.
Conclusion
Less than half of overall patients with LR EPC underwent surgical FT, and this proportion decreased significantly in elderly individuals. Clinicians should focus attention on elderly patients with EPC to provide appropriate medical advice.
Keyword
Figure
Cited by 5 articles
-
Trend Analysis and Prediction of Hepatobiliary Pancreatic Cancer Incidence and Mortality in Korea
Hyeong Min Park, Young-Joo Won, Mee Joo Kang, Sang-Jae Park, Sun-Whe Kim, Kyu-Won Jung, Sung-Sik Han
J Korean Med Sci. 2022;37(28):e216. doi: 10.3346/jkms.2022.37.e216.Surgical management for elderly patients with pancreatic cancer
Sun-Whe Kim
Ann Surg Treat Res. 2023;105(2):63-68. doi: 10.4174/astr.2023.105.2.63.Incidence, mortality and survival of gallbladder, extrahepatic bile duct, and pancreatic cancer using Korea central cancer registry database: 1999-2019
Mee Joo Kang, E Hwa Yun, Kyu-Won Jung, Sang-Jae Park
Int J Stem Cells. 2022;26(3):220-228. doi: 10.14701/ahbps.22-041.Incidence, mortality, and survival of liver cancer using Korea central cancer registry database: 1999-2019
Sung Yeon Hong, Mee Joo Kang, Taegyu Kim, Kyu-Won Jung, Bong-Wan Kim
Int J Stem Cells. 2022;26(3):211-219. doi: 10.14701/ahbps.22-044.Exocrine pancreatic cancer as a second primary malignancy: A population-based study
Mee Joo Kang, Jiwon Lim, Sung-Sik Han, Hyeong Min Park, Sung Chun Cho, Sang-Jae Park, Sun-Whe Kim, Young-Joo Won
Ann Hepatobiliary Pancreat Surg. 2023;27(4):415-422. doi: 10.14701/ahbps.23-053.
Reference
-
References
1. The Global Cancer Observatory Cancer today; pancreas (C25) [Internet]. Lyon: International Agency for Research on Cancer;c2020. [cited 2021 Mar 5]. Available from: https://gco.iarc.fr/today/data/factsheets/cancers/13-Pancreas-fact-sheet.pdf .2. National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: pancreatic adenocarcinoma, version 2, 2021 [Internet]. Plymouth Meeting, PA: National Comprehensive Cancer Network;c2021. [cited 2021 Mar 5]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf .3. Khorana AA, McKernin SE, Berlin J, Hong TS, Maitra A, Moravek C, et al. Potentially curable pancreatic adenocarcinoma: ASCO clinical practice guideline update. J Clin Oncol. 2019; 37:2082–8.
Article4. Ducreux M, Cuhna AS, Caramella C, Hollebecque A, Burtin P, Goere D, et al. Cancer of the pancreas: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2015; 26(Suppl 5):v56–68.
Article5. Lutfi W, Zenati MS, Zureikat AH, Zeh HJ, Hogg ME. Health disparities impact expected treatment of pancreatic ductal adenocarcinoma nationally. Ann Surg Oncol. 2018; 25:1860–7.
Article6. Huang L, Jansen L, Balavarca Y, van der Geest L, Lemmens V, Van Eycken L, et al. Nonsurgical therapies for resected and unresected pancreatic cancer in Europe and USA in 2003–2014: a large international population-based study. Int J Cancer. 2018; 143:3227–39.
Article7. World Bank Group. Indicators: life expectancy at birth, total (years) [Internet]. Washington, DC: The World Bank Group;c2021. [cited 2021 Mar 5]. Available from: https://data.worldbank.org/indicator .8. National Cancer Institute. Surveillance, Epidemiology, and End Results Program Cancer stat facts: pancreatic cancer [Internet]. Bethesda, MD: U.S. National Institutes of Health, National Cancer Institute;c2020. [cited 2021 Mar 5]. Available from: https://seer.cancer.gov/statfacts/html/pancreas.html .9. Dimou F, Sineshaw H, Parmar AD, Tamirisa NP, Jemal A, Riall TS. Trends in receipt and timing of multimodality therapy in early-stage pancreatic cancer. J Gastrointest Surg. 2016; 20:93–103.
Article10. Hue JJ, Bingmer K, Sugumar K, Ocuin LM, Rothermel LD, Winter JM, et al. Mortality and survival among octogenarians with localized pancreatic head xancer: a national cancer database analysis. J Gastrointest Surg. 2021; 25:2582–92.11. Kang MJ, Lim J, Han SS, Park HM, Kim SW, Won YJ, et al. Impact of changes in the topographic classification of Klatskin tumor on incidence of intra- and extrahepatic bile duct cancer: a population-based national cancer registry study. J Hepatobiliary Pancreat Sci. 2021; 28:740–50.
Article12. National Cancer Institute. SEER training modules [Internet]. Bethesda, MD: U.S. National Institutes of Health, National Cancer Institute;2020. [cited 2021 Mar 5]. Available from: https://training.seer.cancer.gov/ .13. Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J Oncol. 2019; 10:10–27.
Article14. World Health Organization. World Health Organization. ICD-10: international statistical classification of diseases and related health problems. 10th revision, version for 2010. Geneva: World Health Organization;2010.15. Man D, Wu J, Shen Z, Zhu X. Prognosis of patients with neuroendocrine tumor: a SEER database analysis. Cancer Manag Res. 2018; 10:5629–38.
Article16. Gordon-Dseagu VL, Devesa SS, Goggins M, Stolzenberg-Solomon R. Pancreatic cancer incidence trends: evidence from the Surveillance, Epidemiology and End Results (SEER) population-based data. Int J Epidemiol. 2018; 47:427–39.
Article17. American College of Surgeons. Standards for oncology registry entry (STORE) 2018 [Internet]. Chicago, IL: American College of Surgeons;[cited 2021 Mar 5]. Available from: https://www.facs.org/-/media/files/quality-programs/cancer/ncdb/store_manual_2018.ashx .18. Ederer F, Heise H. Instructions to IBM 650 programmers in processing survival computations. Vol. 10 Methodological note. Bethesda, MD: National Cancer Institute;1959.19. World Health Organization. Barriers to early cancer diagnosis and treatment [Internet]. Copenhagen: WHO Regional Office for Europe;2019. [cited 2021 Mar 3]. Available from: https://www.euro.who.int/en/health-topics/noncommunicable-diseases/cancer/policy/screening-and-early-detection/barriers-to-early-cancer-diagnosis-and-treatment .20. Kasumova GG, Eskander MF, de Geus SWL, Neto MM, Tabatabaie O, Ng SC, et al. Regional variation in the treatment of pancreatic adenocarcinoma: decreasing disparities with multimodality therapy. Surgery. 2017; 162:275–84.
Article21. Abdel-Rahman O, Xu Y, Tang PA, Lee-Ying RM, Cheung WY. A real-world, population-based study of patterns of referral, treatment, and outcomes for advanced pancreatic cancer. Cancer Med. 2018; 7:6385–92.
Article22. Mavros MN, Coburn NG, Davis LE, Mahar AL, Liu Y, Beyfuss K, et al. Low rates of specialized cancer consultation and cancer-directed therapy for noncurable pancreatic adenocarcinoma: a population-based analysis. CMAJ. 2019; 191:E574–80.
Article23. Shin Y, Lee L. The health insurance system in Korea and its implications. World Hosp Health Serv. 1995; 31:3–9.24. Eom BW, Jung KW, Won YJ, Kim YW. Trends and outcomes of non-compliance with treatment for gastric cancer in Korea over the 16 years from 1999 to 2015. J Gastric Cancer. 2019; 19:92–101.
Article25. Bilimoria KY, Bentrem DJ, Ko CY, Stewart AK, Winchester DP, Talamonti MS. National failure to operate on early stage pancreatic cancer. Ann Surg. 2007; 246:173–80.
Article26. Kirkegard J, Mortensen FV, Hansen CP, Mortensen MB, Sall M, Fristrup C. Waiting time to surgery and pancreatic cancer survival: a nationwide population-based cohort study. Eur J Surg Oncol. 2019; 45:1901–5.27. van der Geest LG, Besselink MG, van Gestel YR, Busch OR, de Hingh IH, de Jong KP, et al. Pancreatic cancer surgery in elderly patients: balancing between short-term harm and long-term benefit. A population-based study in the Netherlands. Acta Oncol. 2016; 55:278–85.
Article28. Suzuki T, Kawai S, Ueno M, Lin Y, Kikuchi S. Treatment patterns in pancreatic cancer patients based on a hospital claims database in Japan. Jpn J Clin Oncol. 2021; 51:228–34.
Article29. King JC, Zenati M, Steve J, Winters SB, Bartlett DL, Zureikat AH, et al. Deviations from expected treatment of pancreatic cancer in octogenarians: analysis of patient and surgeon factors. Ann Surg Oncol. 2016; 23:4149–55.
Article30. Marosi C, Koller M. Challenge of cancer in the elderly. ESMO Open. 2016; 1:e000020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Treatment of Chronic Pancreatitis
- The Use of Pancreatic Exocrine Insufficiency-Questionnaire (PEI-Q)
- Pancreatic Diseases: Genetics and Modeling Using Human Pluripotent Stem Cells
- Medication, Nutrition, and Diet in Chronic Pancreatitis
- Canine exocrine pancreatic insufficiency treated with porcine pancreatic extract