J Korean Med Sci.
2021 Nov;36(43):e273. 10.3346/jkms.2021.36.e273.
Antimicrobial Susceptibility Trends and Risk Factors for Antimicrobial Resistance in Pseudomonas aeruginosa Bacteremia: 12-Year Experience in a Tertiary Hospital in Korea
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Hospital, Busan, Korea
- KMID: 2522286
- DOI: http://doi.org/10.3346/jkms.2021.36.e273
Abstract
- Background
Infections caused by multidrug-resistant Pseudomonas aeruginosa (MDRPA) have been on the rise worldwide, and delayed active antimicrobial therapy is associated with high mortality. However, few studies have evaluated increases in P. aeruginosa infections with antimicrobial resistance and risk factors for such antimicrobial resistance in Korea. Here, we analyzed changes in antimicrobial susceptibility associated with P. aeruginosa bacteremia and identified risk factors of antimicrobial resistance.
Methods
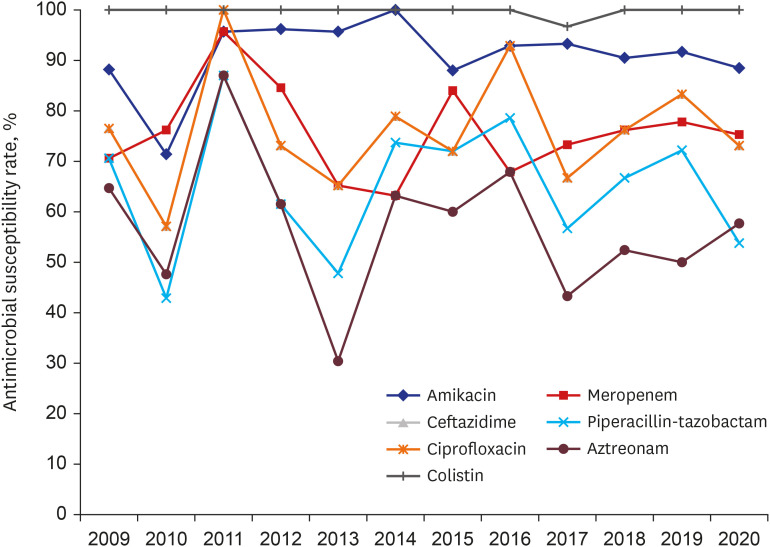
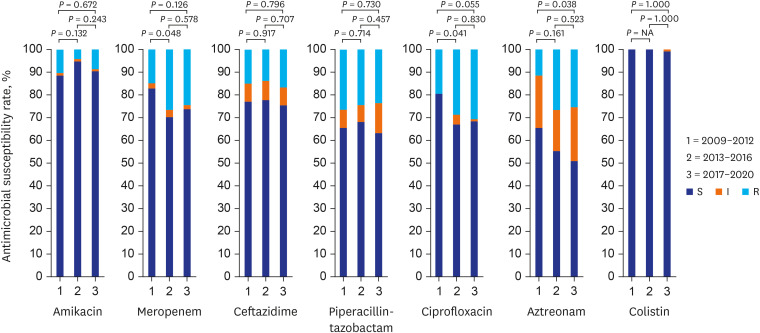
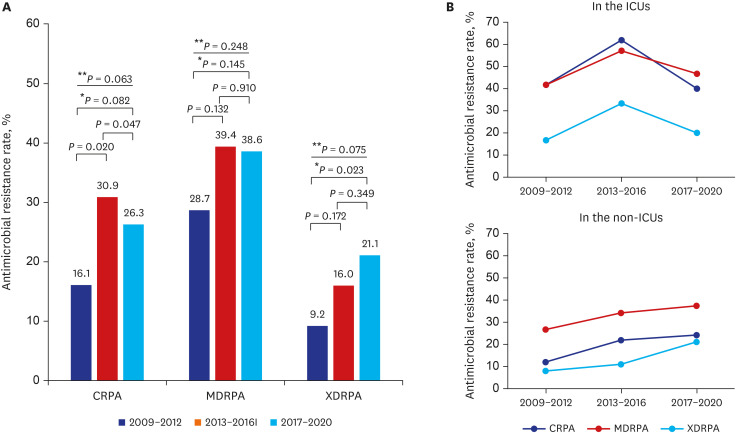
The medical records of patients with P. aeruginosa bacteremia who were admitted to a tertiary hospital between January 2009 and October 2020 were retrospectively reviewed. Antibiotic resistance rates were compared among the time periods of 2009–2012, 2013–2016, and 2017–2020 and between the intensive care unit (ICU) and non-ICU setting. Empirical antimicrobial therapy was considered concordant, if the organism was susceptible to antibiotics in vitro, and discordant, if resistant.
Results
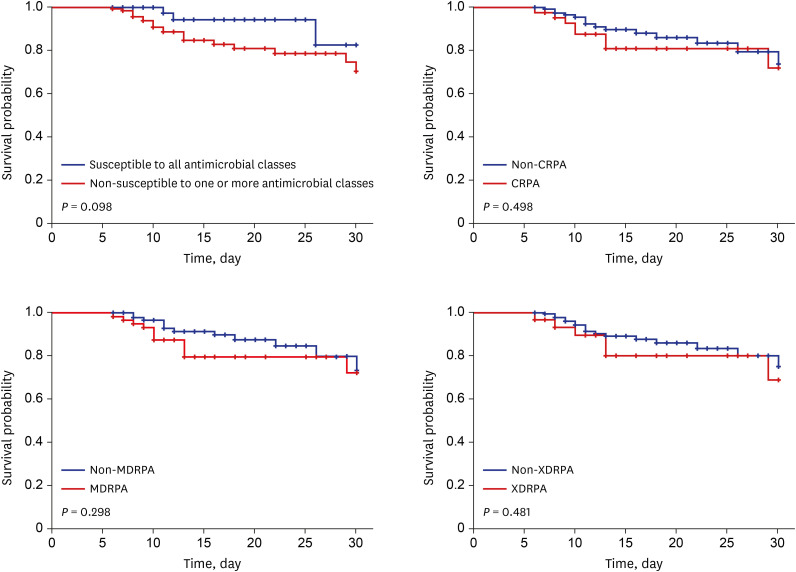
During the study period, 295 patients with P. aeruginosa bacteremia were identified. The hepatobiliary tract (26.8%) was the most common primary site of infection. The rates of carbapenem-resistant P. aeruginosa (CRPA), MDRPA, and extensively drug-resistant P. aeruginosa (XDRPA) were 24.7%, 35.9%, and 15.9%, respectively. XDRPA showed an increasing trend, and CRPA, MDRPA, and XDRPA were also gradually increasing in non-ICU setting. Previous exposure to fluoroquinolones and glycopeptides and urinary tract infection were independent risk factors associated with CRPA, MDRPA, and XDRPA. Previous exposure to carbapenems was an independent risk factor of CRPA. CRPA, MDRPA, and XDRPA were associated with discordant empirical antimicrobial therapy.
Conclusion
The identification of risk factors for antimicrobial resistance and analysis of antimicrobial susceptibility might be important for concordant empirical antimicrobial therapy in patients with P. aeruginosa bacteremia.
Figure
Reference
-
1. Parkins MD, Gregson DB, Pitout JD, Ross T, Laupland KB. Population-based study of the epidemiology and the risk factors for Pseudomonas aeruginosa bloodstream infection. Infection. 2010; 38(1):25–32. PMID: 20012908.2. Callejas-Díaz A, Fernández-Pérez C, Ramos-Martínez A, Múñez-Rubio E, Sánchez-Romero I, Vargas Núñez JA. Impact of Pseudomonas aeruginosa bacteraemia in a tertiary hospital: mortality and prognostic factors. Med Clin (Barc). 2019; 152(3):83–89. PMID: 29885868.3. Kang CI, Kim SH, Kim HB, Park SW, Choe YJ, Oh MD, et al. Pseudomonas aeruginosa bacteremia: risk factors for mortality and influence of delayed receipt of effective antimicrobial therapy on clinical outcome. Clin Infect Dis. 2003; 37(6):745–751. PMID: 12955633.4. Suárez C, Peña C, Tubau F, Gavaldà L, Manzur A, Dominguez MA, et al. Clinical impact of imipenem-resistant Pseudomonas aeruginosa bloodstream infections. J Infect. 2009; 58(4):285–290. PMID: 19297028.5. Buehrle DJ, Shields RK, Clarke LG, Potoski BA, Clancy CJ, Nguyen MH. Carbapenem-resistant Pseudomonas aeruginosa bacteremia: risk factors for mortality and microbiologic treatment failure. Antimicrob Agents Chemother. 2016; 61(1):e01243-16. PMID: 27821456.
Article6. Kadri SS, Adjemian J, Lai YL, Spaulding AB, Ricotta E, Prevots DR, et al. Difficult-to-treat resistance in gram-negative bacteremia at 173 US hospitals: retrospective cohort analysis of prevalence, predictors, and outcome of resistance to all first-line agents. Clin Infect Dis. 2018; 67(12):1803–1814. PMID: 30052813.
Article7. Merchant S, Proudfoot EM, Quadri HN, McElroy HJ, Wright WR, Gupta A, et al. Risk factors for Pseudomonas aeruginosa infections in Asia-Pacific and consequences of inappropriate initial antimicrobial therapy: a systematic literature review and meta-analysis. J Glob Antimicrob Resist. 2018; 14:33–44. PMID: 29454906.8. Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2013. Updated 2013. Accessed July 15, 2021. https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf.9. Centers for Disease Control and Prevention (CDC). Antibiotic resistance threats in the United States, 2019. Updated 2019. Accessed July 15, 2021. https://www.cdc.gov/drugresistance/pdf/threats-report/2019-ar-threats-report-508.pdf.10. Horcajada JP, Montero M, Oliver A, Sorlí L, Luque S, Gómez-Zorrilla S, et al. Epidemiology and treatment of multidrug-resistant and extensively drug-resistant Pseudomonas aeruginosa Infections. Clin Microbiol Rev. 2019; 32(4):e00031-19. PMID: 31462403.
Article11. Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America guidance on the treatment of extended-spectrum β-lactamase producing Enterobacterales (ESBL-E), carbapenem-resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis. 2021; 72(7):e169–e183. PMID: 33106864.12. Korea Centers for Disease Control and Prevention (KCDC). Korean Antimicrobial Resistance Monitoring System: KARMS 2016 Annual Report. Cheongju, Korea: KCDC;2018.13. Liu C, Yoon EJ, Kim D, Shin JH, Shin JH, Shin KS, et al. Antimicrobial resistance in South Korea: a report from the Korean Global Antimicrobial Resistance Surveillance System (Kor-GLASS) for 2017. J Infect Chemother. 2019; 25(11):845–859. PMID: 31311694.
Article14. Raman G, Avendano EE, Chan J, Merchant S, Puzniak L. Risk factors for hospitalized patients with resistant or multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2018; 7:79. PMID: 29997889.
Article15. Aloush V, Navon-Venezia S, Seigman-Igra Y, Cabili S, Carmeli Y. Multidrug-resistant Pseudomonas aeruginosa: risk factors and clinical impact. Antimicrob Agents Chemother. 2006; 50(1):43–48. PMID: 16377665.16. Palavutitotai N, Jitmuang A, Tongsai S, Kiratisin P, Angkasekwinai N. Epidemiology and risk factors of extensively drug-resistant Pseudomonas aeruginosa infections. PLoS One. 2018; 13(2):e0193431. PMID: 29470531.17. Samonis G, Vardakas KZ, Kofteridis DP, Dimopoulou D, Andrianaki AM, Chatzinikolaou I, et al. Characteristics, risk factors and outcomes of adult cancer patients with extensively drug-resistant Pseudomonas aeruginosa infections. Infection. 2014; 42(4):721–728. PMID: 24912861.18. Lee CH, Su TY, Ye JJ, Hsu PC, Kuo AJ, Chia JH, et al. Risk factors and clinical significance of bacteremia caused by Pseudomonas aeruginosa resistant only to carbapenems. J Microbiol Immunol Infect. 2017; 50(5):677–683. PMID: 26188977.19. Joo EJ, Kang CI, Ha YE, Kang SJ, Park SY, Chung DR, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia: clinical impact of antimicrobial resistance on outcome. Microb Drug Resist. 2011; 17(2):305–312. PMID: 21381966.20. Clinical and Laboratory Standards Institute (CLSI). Performance Standards for Antimicrobial Susceptibility Testing. 29th ed. Wayne, PA, USA: CLSI;2019.21. Yo CH, Hsein YC, Wu YL, Hsu WT, Ma MH, Tsai CH, et al. Clinical predictors and outcome impact of community-onset polymicrobial bloodstream infection. Int J Antimicrob Agents. 2019; 54(6):716–722. PMID: 31560960.
Article22. Haque M, Sartelli M, McKimm J, Abu Bakar M. Health care-associated infections - an overview. Infect Drug Resist. 2018; 11:2321–2333. PMID: 30532565.23. Revelas A. Healthcare - associated infections: a public health problem. Niger Med J. 2012; 53(2):59–64. PMID: 23271847.
Article24. Centers for Disease Control and Prevention (CDC). CDC/NHSN surveillance definitions for specific types of infections. Updated 2021. Accessed July 15, 2021. https://www.cdc.gov/nhsn/pdfs/pscmanual/17pscnosinfdef_current.pdf.25. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016; 315(8):801–810. PMID: 26903338.
Article26. Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012; 18(3):268–281. PMID: 21793988.
Article27. Aryee A, Rockenschaub P, Gill MJ, Hayward A, Shallcross L. The relationship between clinical outcomes and empirical antibiotic therapy in patients with community-onset gram-negative bloodstream infections: a cohort study from a large teaching hospital. Epidemiol Infect. 2020; 148:e225. PMID: 32912362.
Article28. Kadri SS, Lai YL, Warner S, Strich JR, Babiker A, Ricotta EE, et al. Inappropriate empirical antibiotic therapy for bloodstream infections based on discordant in-vitro susceptibilities: a retrospective cohort analysis of prevalence, predictors, and mortality risk in US hospitals. Lancet Infect Dis. 2021; 21(2):241–251. PMID: 32916100.
Article29. Korean Disease Control and Prevention Agency (KDCA). National Antimicrobial Resistance Surveillance in Korea 2019 Annual Report. Cheongju, Korea: KDCA;2020.30. Korean National Healthcare-associated Infections Surveillance System (KONIS). ICU reports. Updated 2021. Accessed May 1, 2021. http://konis.cafe24.com/xe/reports_icu_y.31. Tuon FF, Gortz LW, Rocha JL. Risk factors for pan-resistant Pseudomonas aeruginosa bacteremia and the adequacy of antibiotic therapy. Braz J Infect Dis. 2012; 16(4):351–356. PMID: 22846123.32. Nathwani D, Raman G, Sulham K, Gavaghan M, Menon V. Clinical and economic consequences of hospital-acquired resistant and multidrug-resistant Pseudomonas aeruginosa infections: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2014; 3(1):32. PMID: 25371812.
Article33. Bassetti M, Vena A, Croxatto A, Righi E, Guery B. How to manage Pseudomonas aeruginosa infections. Drugs Context. 2018; 7:212527. PMID: 29872449.34. Montero MM, López Montesinos I, Knobel H, Molas E, Sorlí L, Siverio-Parés A, et al. Risk factors for mortality among patients with Pseudomonas aeruginosa bloodstream infections: What is the influence of XDR phenotype on outcomes? J Clin Med. 2020; 9(2):514.35. Kim YJ, Jun YH, Kim YR, Park KG, Park YJ, Kang JY, et al. Risk factors for mortality in patients with Pseudomonas aeruginosa bacteremia; retrospective study of impact of combination antimicrobial therapy. BMC Infect Dis. 2014; 14:161. PMID: 24655422.
Article36. Peña C, Cabot G, Gómez-Zorrilla S, Zamorano L, Ocampo-Sosa A, Murillas J, et al. Influence of virulence genotype and resistance profile in the mortality of Pseudomonas aeruginosa bloodstream infections. Clin Infect Dis. 2015; 60(4):539–548. PMID: 25378459.37. Jeong SJ, Yoon SS, Bae IK, Jeong SH, Kim JM, Lee K. Risk factors for mortality in patients with bloodstream infections caused by carbapenem-resistant Pseudomonas aeruginosa: clinical impact of bacterial virulence and strains on outcome. Diagn Microbiol Infect Dis. 2014; 80(2):130–135. PMID: 25112900.38. Matuschek E, Åhman J, Webster C, Kahlmeter G. Antimicrobial susceptibility testing of colistin - evaluation of seven commercial MIC products against standard broth microdilution for Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter spp. Clin Microbiol Infect. 2018; 24(8):865–870. PMID: 29221995.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antimicrobial Resistance and Clones of Acinetobacter Species and Pseudomonas aeruginosa
- The Trends of the Species and Antimicrobial Susceptibility of Bacteria and Fungi Isolated from Blood Cultures (1986-1996)
- Antimicrobial Susceptibility and Clonal Distribution of the Blood Isolates of Pseudomonas aeruginosa from Two Korean Hospitals
- EUCAST v.12.0 review focused on changes
- Urinary Isolates and Antimicrobial Resistance in the Urine Collected from Patients Admitted into Primary-Care Hospital in Shiheung District