J Korean Med Sci.
2021 Oct;36(39):e280. 10.3346/jkms.2021.36.e280.
Estimation of Excess All-cause Mortality during COVID-19 Pandemic in Korea
- Affiliations
-
- 1Division of Evidence-Based Research, HIRA Research Institute, Health Insurance Review and Assessment Service (HIRA), Wonju, Korea
- 2Division of Healthcare Resource Policy Research, HIRA Research Institute, Health Insurance Review and Assessment Service (HIRA), Wonju, Korea
- 3Department of Public Health and Community Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 4HIRA Research Institute, Health Insurance Review and Assessment Service (HIRA), Wonju, Korea
- 5Public Healthcare Center, Seoul National University Hospital, Seoul, Korea
- 6Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2521196
- DOI: http://doi.org/10.3346/jkms.2021.36.e280
Abstract
- Background
Excess all-cause mortality is helpful to assess the full extent of the health impact, including direct and indirect deaths of coronavirus disease 2019 (COVID-19). The study aimed to estimate overall and regional excess all-cause mortality during the pandemic in Korea.
Methods
We obtained all-cause death data and population statistics from January 2010 to December 2020. The expected mortality in 2020 was estimated using a quasi-Poisson regression model. The model included death year, seasonal variation, cold wave (January), average death counts in the previous month, and population. Excess mortality was defined as the difference between the observed mortality and the expected mortality. Regions were classified into three areas according to the numbers of COVID-19 cases.
Results
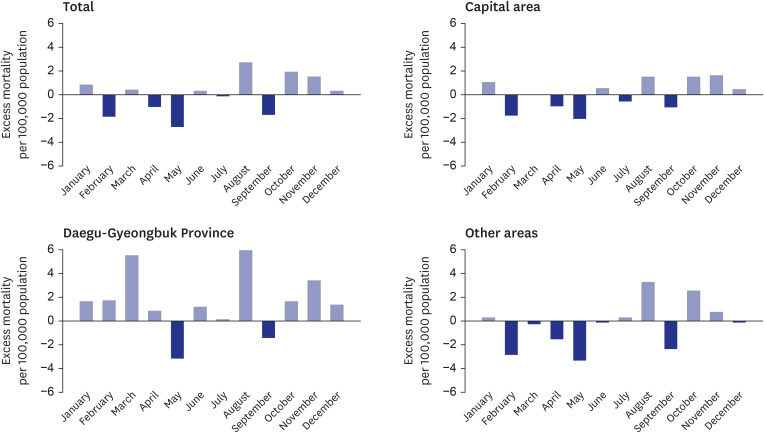
There was no annual excess all-cause mortality in 2020 at the national and regional level compared to the average death for the previous ten years. The observed mortality in 2020 was 582.9 per 100,000 people, and the expected mortality was 582.3 per 100,000 people (95% confidence interval, 568.3–596.7). However, we found monthly and regional variations depending on the waves of the COVID-19 pandemic in Korea. While the mortality in August, October, and November exceeded the expected range, the mortality in September was lower than the expected range. The months in which excess deaths were identified differed by region.
Conclusion
Our results show that the mortality in 2020 was similar to the historical trend. However, in the era of the COVID-19 pandemic, it would be necessary to regularly investigate COVID-19-related mortality and determine its direct and indirect causes.
Keyword
Figure
Cited by 1 articles
-
Analysis of the Effects of COVID-19 on Hip Fractures in Korea Without Lockdown: Interrupted Time Series Analysis Using a Nationwide Cohort
Suk-Yong Jang, Yonghan Cha, Yongwoo Kim, Kap-Jung Kim, Hayong Kim, Wonsik Choy
J Korean Med Sci. 2023;38(18):e137. doi: 10.3346/jkms.2023.38.e137.
Reference
-
1. Mallapaty S. Where did COVID come from? Five mysteries that remain. Nature. 2021; 591(7849):188–189. PMID: 33637873.
Article2. World Health Organization. Coronavirus (COVID-19) dashboard; published online. Updated 2021. Accessed May 8, 2021. https://covid19.who.int.3. Bilinski A, Emanuel EJ. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020; 324(20):2100–2102. PMID: 33044514.
Article4. Beaney T, Clarke JM, Jain V, Golestaneh AK, Lyons G, Salman D, et al. Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? J R Soc Med. 2020; 113(9):329–334. PMID: 32910871.
Article5. Karlinsky A, Kobak D. Tracking excess mortality across countries during the COVID-19 pandemic with the World Mortality Dataset. Elife. 2021; 10:e69336. PMID: 34190045.
Article6. Kaczorowski J, Del Grande C. Beyond the tip of the iceberg: direct and indirect effects of COVID-19. Lancet Digit Health. 2021; 3(4):e205–e206. PMID: 33612431.
Article7. Morgan D, Ino J, Paolantonio GD, Murti F. Excess Mortality: Measuring the direct and indirect impact of COVID-19. OECD Health Working Papers, No. 122. Paris, France: OECD Publishing;2020.8. Vestergaard LS, Mølbak K. Timely monitoring of total mortality associated with COVID-19: informing public health and the public. Euro Surveill. 2020; 25(34):2001591.
Article9. Korea Central Disaster and Safety Countermeasure Health Quarters on COVID-19. Regular briefing on COVID-19 status in Korea. Updated 2021. Accessed December 13, 2021. http://ncov.mohw.go.kr/tcmBoardView.do?brdId=3&brdGubun=31&dataGubun=&ncvContSeq=4541&contSeq=4541&board_id=312&gubun=ALL.10. Sanmarchi F, Golinelli D, Lenzi J, Esposito F, Capodici A, Reno C, et al. Exploring the gap between excess mortality and COVID-19 deaths in 67 countries. JAMA Netw Open. 2021; 4(7):e2117359. PMID: 34269809.
Article11. Islam N, Shkolnikov VM, Acosta RJ, Klimkin I, Kawachi I, Irizarry RA, et al. Excess deaths associated with covid-19 pandemic in 2020: age and sex disaggregated time series analysis in 29 high income countries. BMJ. 2021; 373(1137):n1137. PMID: 34011491.
Article12. Ritchie H, Ortiz-Ospina E, Beltekian D, Mathieu E, Hasell J, Macdonald B, et al. Coronavirus pandemic (COVID-19). Published online at OurWorldInData.org. Updated 2020. Accessed May 8, 2021. https://ourworldindata.org/coronavirus.13. Weinberger DM, Chen J, Cohen T, Crawford FW, Mostashari F, Olson D, et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020; 180(10):1336–1344. PMID: 32609310.
Article14. Sinnathamby MA, Whitaker H, Coughlan L, Lopez Bernal J, Ramsay M, Andrews N. All-cause excess mortality observed by age group and regions in the first wave of the COVID-19 pandemic in England. Euro Surveill. 2020; 25(28):2001239.
Article15. Banerjee A, Chen S, Pasea L, Lai AG, Katsoulis M, Denaxas S, et al. Excess deaths in people with cardiovascular diseases during the COVID-19 pandemic. Eur J Prev Cardiol. Forthcoming. 2021; DOI: 10.1093/eurjpc/zwaa155.
Article16. Faust JS, Krumholz HM, Du C, Mayes KD, Lin Z, Gilman C, et al. All-cause excess mortality and COVID-19–related mortality among US adults aged 25–44 years, March-July 2020. JAMA. 2021; 325(8):785–787. PMID: 33325994.
Article17. Michelozzi P, de'Donato F, Scortichini M, Pezzotti P, Stafoggia M, De Sario M, et al. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health. 2020; 20(1):1238. PMID: 32795276.
Article18. Scortichini M, Schneider Dos Santos R, De' Donato F, De Sario M, Michelozzi P, Davoli M, et al. Excess mortality during the COVID-19 outbreak in Italy: a two-stage interrupted time-series analysis. Int J Epidemiol. 2021; 49(6):1909–1917. PMID: 33053172.
Article19. Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L, Taylor DD. Excess deaths from COVID-19 and other causes, March–July 2020. JAMA. 2020; 324(15):1562–1564. PMID: 33044483.
Article20. Douglas M, Katikireddi SV, Taulbut M, McKee M, McCartney G. Mitigating the wider health effects of covid-19 pandemic response. BMJ. 2020; 369:m1557. PMID: 32341002.
Article21. Center of Disease Control and Prevention. Excess Deaths Associated with COVID-19. Updated 2021. Accessed April 12, 2021. https://www.cdc.gov/nchs/nvss/vsrr/covid19/excess_deaths.htm.22. Statistics Canada. Infographic 1: Provisional adjusted weekly number of deaths and expected number of deaths, Canada. Updated 2020. Accessed April 12, 2021. https://www150.statcan.gc.ca/n1/daily-quotidien/201224/g-b001-eng.htm.23. Australian Bureau of Statistics. Measuring excess mortality in Australia during the COVID-19 pandemic. Updated 2020. Accessed April 12, 2021. https://www.abs.gov.au/articles/measuring-excess-mortality-australia-during-covid-19-pandemic.24. The Statistics Korea. Excess mortality during the COVID-19 pandemic. Updated 2021. Accessed April 12, 2021. https://kosis.kr/covid/statistics_excessdeath.do.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Excess Deaths in Korea During the COVID-19 Pandemic: 2020-2022
- Excess mortality in older adults and cumulative excess mortality across all ages during the COVID-19 pandemic in the 20 countries with the highest mortality rates worldwide
- The epidemiologic characteristics of dog-bite injury during COVID-19 pandemic in Korea
- Estimating Excess Mortality During the COVID-19 Pandemic Between 2020–2022 in Korea
- Age-Related Morbidity and Mortality among Patients with COVID-19