J Stroke.
2021 Sep;23(3):327-342. 10.5853/jos.2021.02306.
Clot Composition Analysis as a Diagnostic Tool to Gain Insight into Ischemic Stroke Etiology: A Systematic Review
- Affiliations
-
- 1Joint Cerebrovascular Research Unit, La Fe Health Research Institute, University of Valencia, Valencia, Spain
- 2Department of Physiology, University of Valencia, Valencia, Spain
- 3Stroke Unit, Neurology Service, La Fe University and Polytechnic Hospital, Valencia, Spain
- KMID: 2520911
- DOI: http://doi.org/10.5853/jos.2021.02306
Abstract
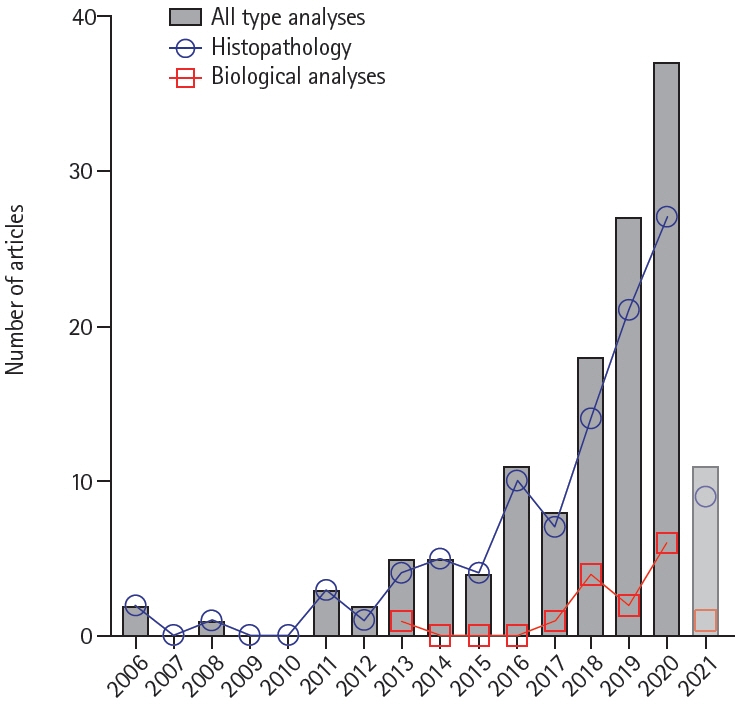
- Mechanical thrombectomy renders the occluding clot available for analysis. Insights into thrombus composition could help establish the stroke cause. We aimed to investigate the value of clot composition analysis as a complementary diagnostic tool in determining the etiology of large vessel occlusion (LVO) ischemic strokes (International Prospective Register of Systematic Reviews [PROSPERO] registration # CRD42020199436). Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, we ran searches on Medline (using the PubMed interface) and Web of Science for studies reporting analyses of thrombi retrieved from LVO stroke patients subjected to mechanical thrombectomy (January 1, 2006 to September 21, 2020). The PubMed search was updated weekly up to February 22, 2021. Reference lists of included studies and relevant reviews were hand-searched. From 1,714 identified studies, 134 eligible studies (97 cohort studies, 31 case reports, and six case series) were included in the qualitative synthesis. Physical, histopathological, biological, and microbiological analyses provided information about the gross appearance, mechanical properties, structure, and composition of the thrombi. There were non-unanimous associations of thrombus size, structure, and composition (mainly proportions of fibrin and blood formed elements) with the Trial of Org 10172 in Acute Stroke Treatment (TOAST) etiology and underlying pathologies, and similarities between cryptogenic thrombi and those of known TOAST etiology. Individual thrombus analysis contributed to the diagnosis, mainly in atypical cases. Although cohort studies report an abundance of quantitative rates of main thrombus components, a definite clot signature for accurate diagnosis of stroke etiology is still lacking. Nevertheless, the qualitative examination of the embolus remains an invaluable tool for diagnosing individual cases, particularly regarding atypical stroke causes.
Figure
Cited by 1 articles
-
Cancer-Associated Stroke: Thrombosis Mechanism, Diagnosis, Outcome, and Therapeutic Strategies
Ji Hoe Heo, Jaeseob Yun, Kwang Hyun Kim, Jae Wook Jung, Joonsang Yoo, Young Dae Kim, Hyo Suk Nam
J Stroke. 2024;26(2):164-178. doi: 10.5853/jos.2023.03279.
Reference
-
References
1. De Meyer SF, Andersson T, Baxter B, Bendszus M, Brouwer P, Brinjikji W, et al. Analyses of thrombi in acute ischemic stroke: a consensus statement on current knowledge and future directions. Int J Stroke. 2017; 12:606–614.
Article2. Bacigaluppi M, Semerano A, Gullotta GS, Strambo D. Insights from thrombi retrieved in stroke due to large vessel occlusion. J Cereb Blood Flow Metab. 2019; 39:1433–1451.
Article3. Brinjikji W, Duffy S, Burrows A, Hacke W, Liebeskind D, Majoie CB, et al. Correlation of imaging and histopathology of thrombi in acute ischemic stroke with etiology and outcome: a systematic review. J Neurointerv Surg. 2017; 9:529–534.
Article4. Jolugbo P, Ariëns RA. Thrombus composition and efficacy of thrombolysis and thrombectomy in acute ischemic stroke. Stroke. 2021; 52:1131–1142.
Article5. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100.
Article6. Salom JB, Aliena-Valero A, Torregrosa G, Baixauli-Martín J. Clot composition analysis as complementary diagnostic tool to gain insight into ischemic stroke etiology: A systematic review of clinical studies and case reports. National Institute for Health Reearch. https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020199436. August 17, 2020. Accessed September 27, 2021.7. Marder VJ, Chute DJ, Starkman S, Abolian AM, Kidwell C, Liebeskind D, et al. Analysis of thrombi retrieved from cerebral arteries of patients with acute ischemic stroke. Stroke. 2006; 37:2086–93.
Article8. Multimodal Investigation of Intracranial Clot Environment (MISO). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04421326. 2020. Accessed September 27, 2021.9. Investigation of Clot in Ischemic Stroke and Hematoma Evacuation (INSIGHT). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT04693767. 2021. Accessed September 27, 2021.10. Thrombus Composition in Ischemic Stroke: Analysis of the Correlation With Plasma Biomarkers, Efficacy of Treatment, Etiology and Prognosis (COMPO-CLOT). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03268668. 2021. Accessed September 27, 2021.11. Blood And Clot Thrombectomy Registry And Collaboration (BACTRAC). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03153683. 2021. Accessed September 27, 2021.12. https://clinicaltrials.gov/ct2/show/NCT031536RNA Sequencing Analysis in Large Vessel Occlusion Stroke DATA Bank (RNASA-LVOSB). ClinicalTrials.gov. https://clinicaltrials.gov/ct2/show/NCT03490552. 2018. Accessed September 27, 2021.13. Staessens S, Fitzgerald S, Andersson T, Clarençon F, Denorme F, Gounis MJ, et al. Histological stroke clot analysis after thrombectomy: technical aspects and recommendations. Int J Stroke. 2020; 15:467–476.
Article14. Abdel-Wahed L, Shaban A, Hayakawa M, Limaye K. Retrieved arterial clot helps guide antibiotic therapy in infective endocarditis. Am J Med. 2019; 132:e795–e796.
Article15. Biraschi F, Diana F, Alesini F, Guidetti G, Peschillo S. Effective ADAPT thrombectomy in a patient with acute stroke due to cardiac papillary elastofibroma: histological thrombus confirmation. J Stroke Cerebrovasc Dis. 2016; 25:e185–e187.
Article16. Salam KA, Rafeeque M, Hashim H, Mampilly N, Noone ML. Histology of thrombectomy specimen reveals cardiac tumor embolus in cryptogenic young stroke. J Stroke Cerebrovasc Dis. 2018; 27:e70–e72.
Article17. Salinas P, Moreno R, Frutos R, Lopez-Sendon JL. Neurovascular rescue for thrombus-related embolic stroke during transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2013; 6:981–982.
Article18. Scharf EL, Chakraborty T, Rabinstein A, Miranpuri AS. Endovascular management of cerebral septic embolism: three recent cases and review of the literature. J Neurointerv Surg. 2017; 9:463–465.
Article19. Semerano A, Genchi A, Callea M, Sanvito F, Simionato F, Panni P, et al. Thrombus hallmarks reveal atherothrombotic stroke aetiology. J Neurol. 2019; 266:1533–1535.
Article20. Tejada J, Galiana A, Balboa O, Clavera B, Redondo-Robles L, Alonso N, et al. Mechanical endovascular procedure for the treatment of acute ischemic stroke caused by total detachment of a papillary fibroelastoma. J Neurointerv Surg. 2014; 6:e37.
Article21. Thomas MC, Delgado Almandoz JE, Todd AJ, Young ML, Fease JL, Scholz JM, et al. A case of right middle cerebral artery ‘tendonectomy’ following mitral valve replacement surgery. J Neurointerv Surg. 2017; 9:e35.
Article22. Valente M, Saab J, Cordato D, Manning N, Cappelen-Smith C. The diagnostic utility of routine clot analysis after endovascular thrombectomy in a patient with systemic lupus erythematosus and antiphospholipid syndrome. J Clin Neurosci. 2019; 70:247–249.
Article23. Wollenweber FA, Remi J, Bauer A, Theiss H, Massberg S, Patzig M, et al. Thrombectomy recovers an aortic wall fragment from middle cerebral artery immediately after TAVI. Neurology. 2016; 86:2111–2112.
Article24. Anuwatworn A, Raizada A, Kelly S, Stys T, Jonsson O, Stys A. Stroke with valve tissue embolization during transcatheter aortic valve replacement treated with endovascular intervention. JACC Cardiovasc Interv. 2015; 8:1261–1263.
Article25. Chapot R, Wassef M, Bisdorff A, Rogopoulos A, Merland JJ, Houdart E. Occlusion of the middle cerebral artery due to synthetic fibers. AJNR Am J Neuroradiol. 2006; 27:148–150.26. Elodie O, Labeyrie PE, Aubry M, Cecile D, Roux S, Ferry T, et al. Whipple’s endocarditis diagnosed by thrombus analysis retrieved by successful mechanical thrombectomy. J Neurol Sci. 2019; 400:42–43.
Article27. Fassa AA, Mazighi M, Himbert D, Deschamps L, Ducrocq G, Cheong AP, et al. Successful endovascular stroke rescue with retrieval of an embolized calcium fragment after transcatheter aortic valve replacement. Circ Cardiovasc Interv. 2014; 7:125–126.
Article28. Fitzpatrick N, Motyer R, Gibney B, Duffy S, Murphy S, O’Brien P, et al. Expanding the role of stent-retriever endovascular thrombectomy: a case series of free-floating thrombus. J Neurointerv Surg. 2018; 10:1164–1167.
Article29. Garcia-Ptacek S, Matias-Guiu JA, Valencia-Sánchez C, Gil A, Bernal-Becerra I, De las Heras-Revilla V, et al. Mechanical endovascular treatment of acute stroke due to cardiac myxoma. J Neurointerv Surg. 2014; 6:e1.
Article30. Genchi A, Schwarz G, Semerano A, Callea M, Sanvito F, Simionato F, et al. Large vessel occlusion stroke due to dislodged aortic valve calcification revealed by imaging and histopathology. J Neurol Sci. 2020; 408:116573.
Article31. Kan P, Webb S, Siddiqui AH, Levy EI. First reported use of retrievable stent technology for removal of a large septic embolus in the middle cerebral artery. World Neurosurg. 2012; 77:591.
Article32. Kim JM, Jeon JS, Kim YW, Kang DH, Hwang YH, Kim YS. Forced arterial suction thrombectomy of septic embolic middle cerebral artery occlusion due to infective endocarditis: an illustrative case and review of the literature. Neurointervention. 2014; 9:101–5.
Article33. Matsumoto N, Fukuda H, Handa A, Kawasaki T, Kurosaki Y, Chin M, et al. Histological examination of trousseau syndrome-related thrombus retrieved through acute endovascular thrombectomy: report of 2 cases. J Stroke Cerebrovasc Dis. 2016; 25:e227–e230.
Article34. Pisano TJ, Hakkinen I, Rybinnik I. Large vessel occlusion secondary to COVID-19 hypercoagulability in a young patient: a case report and literature review. J Stroke Cerebrovasc Dis. 2020; 29:105307.
Article35. Bourcier R, Duchmann Z, Sgreccia A, Desal H, Carità G, Desilles JP, et al. Diagnostic performances of the susceptibility vessel sign on MRI for the prediction of macroscopic thrombi features in acute ischemic stroke. J Stroke Cerebrovasc Dis. 2020; 29:105245.
Article36. Sgreccia A, Duchmann Z, Desilles JP, Lapergue B, Labreuche J, Kyheng M, et al. Association between acute ischemic stroke etiology and macroscopic aspect of retrieved clots: is a clot’s color a warning light for underlying pathologies? J Neurointerv Surg. 2019; 11:1197–1200.
Article37. Choi MH, Park GH, Lee JS, Lee SE, Lee SJ, Kim JH, et al. Erythrocyte fraction within retrieved thrombi contributes to thrombolytic response in acute ischemic stroke. Stroke. 2018; 49:652–659.
Article38. Fu CH, Chen CH, Lin YH, Lee CW, Tsai LK, Tang SC, et al. Fibrin and platelet-rich composition in retrieved thrombi hallmarks stroke with active cancer. Stroke. 2020; 51:3723–3727.
Article39. Fitzgerald S, Rossi R, Mereuta OM, Jabrah D, Okolo A, Douglas A, et al. Per-pass analysis of acute ischemic stroke clots: impact of stroke etiology on extracted clot area and histological composition. J Neurointerv Surg . 2020 Dec 9 [Epub]. https://doi.org/10.1136/neurintsurg-2020-016966.
Article40. Fitzgerald S, Rossi R, Mereuta OM, Molina S, Okolo A, Douglas A, et al. Large artery atherosclerotic clots are larger than clots of other stroke etiologies and have poorer recanalization rates. J Stroke Cerebrovasc Dis. 2021; 30:105463.
Article41. Rossi R, Fitzgerald S, Molina S, Mereuta OM, Douglas A, Pandit A, et al. The administration of rtPA before mechanical thrombectomy in acute ischemic stroke patients is associated with a significant reduction of the retrieved clot area but it does not influence revascularization outcome. J Thromb Thrombolysis. 2021; 51:545–551.
Article42. Horie N, Shobayashi K, Morofuji Y, Sadakata E, Iki Y, Matsunaga Y, et al. Impact of mechanical thrombectomy device on thrombus histology in acute embolic stroke. World Neurosurg. 2019; 132:e418–e422.
Article43. Almekhlafi MA, Hu WY, Hill MD, Auer RN. Calcification and endothelialization of thrombi in acute stroke. Ann Neurol. 2008; 64:344–348.
Article44. Chueh JY, Wakhloo AK, Hendricks GH, Silva CF, Weaver JP, Gounis MJ. Mechanical characterization of thromboemboli in acute ischemic stroke and laboratory embolus analogs. AJNR Am J Neuroradiol. 2011; 32:1237–1244.
Article45. Liu Y, Zheng Y, Reddy AS, Gebrezgiabhier D, Davis E, Cockrum J, et al. Analysis of human emboli and thrombectomy forces in large-vessel occlusion stroke. J Neurosurg. 2020; 134:893–901.
Article46. Vidmar J, Bajd F, Milosevic ZV, Kocijancic IJ, Jeromel M, Sersa I. Retrieved cerebral thrombi studied by T2 and ADC mapping: preliminary results. Radiol Oncol. 2019; 53:427–433.47. Meher V, Pushie J, Sylvain N, Weese Maley S, Hou H, Peeling L, et al. Analysis of retrieved stroke thrombi from mechanical thrombectomy using X-ray fluorescence imaging and fourier-transform infrared spectroscopy. Int J Stroke. 2018; 13:150.48. Fitzgerald S, Wang S, Dai D, Murphree DH Jr, Pandit A, Douglas A, et al. Orbit image analysis machine learning software can be used for the histological quantification of acute ischemic stroke blood clots. PLoS One. 2019; 14:e0225841.
Article49. Fitzgerald ST, Wang S, Dai D, Douglas A, Kadirvel R, Gounis MJ, et al. Platelet-rich clots as identified by Martius Scarlet Blue staining are isodense on NCCT. J Neurointerv Surg. 2019; 11:1145–1149.
Article50. Fitzgerald S, Dai D, Wang S, Douglas A, Kadirvel R, Layton KF, et al. Platelet-rich emboli in cerebral large vessel occlusion are associated with a large artery atherosclerosis source. Stroke. 2019; 50:1907–1910.
Article51. Kim B, Kim YM, Jin SC, Lee JW, Lee BI, Kim SE, et al. Development of a predictive scale for cardioembolic stroke using extracted thrombi and angiographic findings. J Clin Neurosci. 2020; 73:224–230.
Article52. Schuhmann MK, Gunreben I, Kleinschnitz C, Kraft P. Immunohistochemical analysis of cerebral thrombi retrieved by mechanical thrombectomy from patients with acute ischemic stroke. Int J Mol Sci. 2016; 17:298.
Article53. Staessens S, Denorme F, Francois O, Desender L, Dewaele T, Vanacker P, et al. Structural analysis of ischemic stroke thrombi: histological indications for therapy resistance. Haematologica. 2020; 105:498–507.
Article54. Ye G, Qi P, Chen K, Tan T, Cao R, Chen J, et al. Risk of secondary embolism events during mechanical thrombectomy for acute ischemic stroke: a single-center study based on histological analysis. Clin Neurol Neurosurg. 2020; 193:105749.
Article55. Ye G, Gao Q, Qi P, Wang J, Hu S, Chen K, et al. The role of diabetes mellitus on the thrombus composition in patients with acute ischemic stroke. Interv Neuroradiol. 2020; 26:329–336.
Article56. Mereuta OM, Fitzgerald S, Christensen TA, Jaspersen AL, Dai D, Abbasi M, et al. High-resolution scanning electron microscopy for the analysis of three-dimensional ultrastructure of clots in acute ischemic stroke. J Neurointerv Surg. 2021; 13:906–911.
Article57. Ahn SH, Hong R, Choo IS, Heo JH, Nam HS, Kang HG, et al. Histologic features of acute thrombi retrieved from stroke patients during mechanical reperfusion therapy. Int J Stroke. 2016; 11:1036–1044.
Article58. Benson JC, Fitzgerald ST, Kadirvel R, Johnson C, Dai D, Karen D, et al. Clot permeability and histopathology: is a clot’s perviousness on CT imaging correlated with its histologic composition? J Neurointerv Surg. 2020; 12:38–42.
Article59. Brinjikji W, Fitzgerald S, Kallmes DF, Layton K, Hanel R, Pereira VM, et al. Outcomes of the stroke thromboembolism registry of imaging and pathology: a multicenter international study. Stroke. 2020; 51(Suppl 1):A147.
Article60. Douglas A, Fitzgerald S, Mereuta OM, Rossi R, O’Leary S, Pandit A, et al. Platelet-rich emboli are associated with von Willebrand factor levels and have poorer revascularization outcomes. J Neurointerv Surg. 2020; 12:557–562.
Article61. Duffy S, McCarthy R, Farrell M, Thomas S, Brennan P, Power S, et al. Per-pass analysis of thrombus composition in patients with acute ischemic stroke undergoing mechanical thrombectomy. Stroke. 2019; 50:1156–1163.
Article62. Khismatullin RR, Shakirova AZ, Weisel JW, Litvinov RI. Agedependent differential staining of fibrin in blood clots and thrombi. BioNanoScience. 2020; 10:370–374.
Article63. Di Meglio L, Desilles JP, Ollivier V, Nomenjanahary MS, Di Meglio S, Deschildre C, et al. Acute ischemic stroke thrombi have an outer shell that impairs fibrinolysis. Neurology. 2019; 93:e1686–e1698.
Article64. Niesten JM, van der Schaaf IC, van Dam L, Vink A, Vos JA, Schonewille WJ, et al. Histopathologic composition of cerebral thrombi of acute stroke patients is correlated with stroke subtype and thrombus attenuation. PLoS One. 2014; 9:e88882.
Article65. Park H, Kim J, Ha J, Hwang IG, Song TJ, Yoo J, et al. Histological features of intracranial thrombi in stroke patients with cancer. Ann Neurol. 2019; 86:143–149.
Article66. Novotny J, Oberdieck P, Titova A, Pelisek J, Chandraratne S, Nicol P, et al. Thrombus NET content is associated with clinical outcome in stroke and myocardial infarction. Neurology. 2020; 94:e2346–e2360.
Article67. Goebel J, Gaida BJ, Wanke I, Kleinschnitz C, Koehrmann M, Forsting M, et al. Is histologic thrombus composition in acute stroke linked to stroke etiology or to interventional parameters? AJNR Am J Neuroradiol. 2020; 41:650–657.
Article68. Sporns PB, Krähling H, Psychogios MN, Jeibmann A, Minnerup J, Broocks G, et al. Small thrombus size, thrombus composition, and poor collaterals predict pre-interventional thrombus migration. J Neurointerv Surg. 2021; 13:409–414.69. Sporns PB, Jeibmann A, Minnerup J, Broocks G, Nawabi J, Schön G, et al. Histological clot composition is associated with preinterventional clot migration in acute stroke patients. Stroke. 2019; 50:2065–2071.
Article70. Sporns PB, Hanning U, Schwindt W, Velasco A, Buerke B, Cnyrim C, et al. Ischemic stroke: histological thrombus composition and pre-interventional CT attenuation are associated with intervention time and rate of secondary embolism. Cerebrovasc Dis. 2017; 44:344–350.
Article71. Peña-Martínez C, Durán-Laforet V, García-Culebras A, Ostos F, Hernández-Jiménez M, Bravo-Ferrer I, et al. Pharmacological modulation of neutrophil extracellular traps reverses thrombotic stroke tPA (tissue-type plasminogen activator) resistance. Stroke. 2019; 50:3228–3237.
Article72. Kim SK, Yoon W, Kim TS, Kim HS, Heo TW, Park MS. Histologic analysis of retrieved clots in acute ischemic stroke: correlation with stroke etiology and gradient-echo MRI. AJNR Am J Neuroradiol. 2015; 36:1756–1762.
Article73. Nouh A, Mehta T, Hussain M, Song X, Ollenschleger M. Clot composition of embolic strokes of undetermined source: a feasibility study. BMC Neurol. 2020; 20:383.
Article74. López-Cancio E, Millán M, Pérez de la Ossa N, Dávalos A, Ribó M, Morancho A, et al. Immunohistochemical study of clot composition in thrombi retrieved from MCA with mechanical thrombectomy. Cerebrovasc Dis. 2013; 35:255.75. Elijovich L, Arthur A, Hoit D, Nickele C, Morris D, Vachhani J, et al. Thrombus composition is associated with endothelial injury and stroke etiology in patients undergoing mechanical thrombectomy for emergent large vessel occlusion. Stroke. 2018; 49(Suppl 1):A145.
Article76. Essig F, Kollikowski AM, Pham M, Solymosi L, Stoll G, Haeusler KG, et al. Immunohistological analysis of neutrophils and neutrophil extracellular traps in human thrombemboli causing acute ischemic stroke. Int J Mol Sci. 2020; 21:7387.
Article77. Gurkas E, Asif A, Akpinar CK, Shoukat M, Aytac E, Aydin MC, et al. Thrombus composition and success of thrombectomy in acute ischemic stroke patients: a histopathological analysis. Stroke. 2019; 50(Suppl 1):AWP36.
Article78. Hashimoto T, Hayakawa M, Funatsu N, Yamagami H, Satow T, Takahashi JC, et al. Histopathologic analysis of retrieved thrombi associated with successful reperfusion after acute stroke thrombectomy. Stroke. 2016; 47:3035–3037.
Article79. Liebeskind DS, Sanossian N, Yong WH, Starkman S, Tsang MP, Moya AL, et al. CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke. 2011; 42:1237–1243.
Article80. Liu M, Hao Z, Li R, Cai J, Jiang C, Li Y. Erythrocyte-rich thrombi related to serum iron contribute to single stent retrieval and favorable clinical outcomes in acute ischemic stroke by endovascular treatment. Thromb Res. 2020; 195:8–15.
Article81. Maegerlein C, Friedrich B, Berndt M, Lucia KE, Schirmer L, Poppert H, et al. Impact of histological thrombus composition on preinterventional thrombus migration in patients with acute occlusions of the middle cerebral artery. Interv Neuroradiol. 2018; 24:70–75.
Article82. Maekawa K, Shibata M, Nakajima H, Mizutani A, Kitano Y, Seguchi M, et al. Erythrocyte-rich thrombus is associated with reduced number of maneuvers and procedure time in patients with acute ischemic stroke undergoing mechanical thrombectomy. Cerebrovasc Dis Extra. 2018; 8:39–49.
Article83. Qureshi AI, Qureshi MH, Lobanova I, Bashir A, Khan AA, Bologna SM, et al. Histopathological characteristics of IV recombinant tissue plasminogen-resistant thrombi in patients with acute ischemic stroke. J Vasc Interv Neurol. 2016; 8:38–45.84. Shin JW, Jeong HS, Kwon HJ, Song KS, Kim J. High red blood cell composition in clots is associated with successful recanalization during intra-arterial thrombectomy. PLoS One. 2018; 13:e0197492.
Article85. Simons N, Mitchell P, Dowling R, Gonzales M, Yan B. Thrombus composition in acute ischemic stroke: a histopathological study of thrombus extracted by endovascular retrieval. J Neuroradiol. 2015; 42:86–92.
Article86. Singh P, Doostkam S, Reinhard M, Ivanovas V, Taschner CA. Immunohistochemical analysis of thrombi retrieved during treatment of acute ischemic stroke: does stent-retriever cause intimal damage? Stroke. 2013; 44:1720–1722.87. Darcourt J, Garcia C, Phuong DM, Michelozzi C, Bellanger G, Adam G, et al. Absence of susceptibility vessel sign is associated with aspiration-resistant fibrin/platelet-rich thrombi. Int J Stroke. 2021 Jan 12 [Epub]. https://doi.org/10.1177/1747493020986626.
Article88. Hanning U, Sporns PB, Psychogios MN, Jeibmann A, Minnerup J, Gelderblom M, et al. Imaging-based prediction of histological clot composition from admission CT imaging. J Neurointerv Surg. 2021 Jan 22 [Epub]. https://doi.org/10.1136/neurintsurg-2020-016774.
Article89. Boeckh-Behrens T, Schubert M, Förschler A, Prothmann S, Kreiser K, Zimmer C, et al. The impact of histological clot composition in embolic stroke. Clin Neuroradiol. 2016; 26:189–197.
Article90. Dargazanli C, Rigau V, Eker O, Riquelme Bareiro C, Machi P, Gascou G, et al. High CD3+ cells in intracranial thrombi represent a biomarker of atherothrombotic stroke. PLoS One. 2016; 11:e0154945.
Article91. Donnerstag F, Götz F, Dadak M, Raab P, Iglesias EC, Werlein C, et al. Interventional stroke treatment: is it also safe for arteries?: looking at thrombectomy wall damage through clot histology. Interv Neuroradiol. 2021; 27:404–410.92. Kaesmacher J, Boeckh-Behrens T, Simon S, Maegerlein C, Kleine JF, Zimmer C, et al. Risk of thrombus fragmentation during endovascular stroke treatment. AJNR Am J Neuroradiol. 2017; 38:991–998.
Article93. Laridan E, Denorme F, Desender L, François O, Andersson T, Deckmyn H, et al. Neutrophil extracellular traps in ischemic stroke thrombi. Ann Neurol. 2017; 82:223–232.
Article94. Deng J, Zhao F, Zhang Y, Zhou Y, Xu X, Zhang X, et al. Neutrophil extracellular traps increased by hyperglycemia exacerbate ischemic brain damage. Neurosci Lett. 2020; 738:135383.
Article95. Ducroux C, Di Meglio L, Loyau S, Delbosc S, Boisseau W, Deschildre C, et al. Thrombus neutrophil extracellular traps content impair tPA-induced thrombolysis in acute ischemic stroke. Stroke. 2018; 49:754–757.
Article96. Sporns PB, Hanning U, Schwindt W, Velasco A, Minnerup J, Zoubi T, et al. Ischemic stroke: what does the histological composition tell us about the origin of the thrombus? Stroke. 2017; 48:2206–2210.97. Prochazka V, Jonszta T, Czerny D, Krajca J, Roubec M, Macak J, et al. The role of von Willebrand factor, ADAMTS13, and cerebral artery thrombus composition in patient outcome following mechanical thrombectomy for acute ischemic stroke. Med Sci Monit. 2018; 24:3929–3945.
Article98. Krajíčková D, Krajina A, Šteiner I, Vyšata O, Herzig R, Lojík M, et al. Fibrin clot architecture in acute ischemic stroke treated with mechanical thrombectomy with stent-retrievers: cohort study. Circ J. 2018; 82:866–873.99. Chen SH, Scott XO, Ferrer Marcelo Y, Almeida VW, Blackwelder PL, Yavagal DR, et al. Netosis and inflammasomes in large vessel occlusion thrombi. Front Pharmacol. 2021; 11:607287.
Article100. Mereuta OM, Fitzgerald S, Abbasi M, Dai D, Kadirvel R, Kallmes DF, et al. Von Willebrand factor expression in various subtypes of acute ischemic stroke. Stroke. 2020; 51(Suppl 1):AWP268.
Article101. Funatsu N, Hayakawa M, Hashimoto T, Yamagami H, Satow T, Takahashi JC, et al. Vascular wall components in thrombi obtained by acute stroke thrombectomy: clinical significance and related factors. J Neurointerv Surg. 2019; 11:232–236.
Article102. Bhaskar S, Saab J, Cappelen-Smith C, Killingsworth M, Wu XJ, Cheung A, et al. Clot histopathology in ischemic stroke with infective endocarditis. Can J Neurol Sci. 2019; 46:331–336.
Article103. Mehta RI, Rai AT, Vos JA, Solis OE, Mehta RI. Intrathrombus polymer coating deposition: a pilot study of 91 patients undergoing endovascular therapy for acute large vessel stroke. Part I: Histologic frequency. J Neurointerv Surg. 2019; 11:1191–1196.
Article104. Hund HM, Taha A, Ramlal SA, Hansen D, Autar ASA, van de Lugt A, et al. Foreign bodies are present in thrombi mechanically extracted from patients suffering acute ischemic stroke and who underwent endovascular treatment. J Cereb Blood Flow Metab. 2019; 39:261.105. Sallustio F, Arnò N, Di Legge S, Koch G, Martorana A, Rossi C, et al. Histological features of intracranial thrombo-emboli predict response to endovascular therapy for acute ischemic stroke. J Neurol Disord Stroke. 2015; 3:1105.106. Cline B, Vos J, Carpenter J, Rai A. Pathological analysis of extracted clots in embolectomy patients with acute ischaemic stroke. J NeuroInterv Surg. 2013; 5(Suppl 2):A15–A16.107. Li Y, Wang H, Zhao L, Jian Y, Dang M, Jiang Y, et al. A case report of thrombolysis resistance: thrombus ultrastructure in an ischemic stroke patient. BMC Neurol. 2020; 20:135.
Article108. Khashim Z, Fitzgerald S, Kadirvel R, Dai D, Doyle KM, Brinjikji W, et al. Clots retrieved by mechanical thrombectomy from acute ischemic stroke patients show no evidence of bacteria. Interv Neuroradiol. 2019; 25:502–507.
Article109. Hernández-Fernández F, Rojas-Bartolomé L, García-García J, Ayo-Martín Ó, Molina-Nuevo JD, Barbella-Aponte RA, et al. Histopathological and bacteriological analysis of thrombus material extracted during mechanical thrombectomy in acute stroke patients. Cardiovasc Intervent Radiol. 2017; 40:1851–1860.
Article110. Patrakka O, Pienimäki JP, Tuomisto S, Ollikainen J, Lehtimäki T, Karhunen PJ, et al. Oral bacterial signatures in cerebral thrombi of patients with acute ischemic stroke treated with thrombectomy. J Am Heart Assoc. 2019; 8:e012330.
Article111. Vajpeyee A, Chauhan PS, Pandey S, Tiwari S, Yadav LB, Shroti AK, et al. Metagenomics analysis of thrombus samples retrieved from mechanical thrombectomy. Neurointervention. 2021; 16:39–45.
Article112. Baek BH, Kim HS, Yoon W, Lee YY, Baek JM, Kim EH, et al. Inflammatory mediator expression within retrieved clots in acute ischemic stroke. Ann Clin Transl Neurol. 2018; 5:273–279.
Article113. Rao NM, Capri J, Cohn W, Abdaljaleel M, Restrepo L, Gornbein JA, et al. Peptide composition of stroke causing emboli correlate with serum markers of atherosclerosis and inflammation. Front Neurol. 2017; 8:427.
Article114. Muñoz R, Santamaría E, Rubio I, Ausín K, Ostolaza A, Labarga A, et al. Mass spectrometry-based proteomic profiling of thrombotic material obtained by endovascular thrombectomy in patients with ischemic stroke. Int J Mol Sci. 2018; 19:498.
Article115. Dargazanli C, Zub E, Deverdun J, Decourcelle M, de Bock F, Labreuche J, et al. Machine learning analysis of the cerebrovascular thrombi proteome in human ischemic stroke: an exploratory study. Front Neurol. 2020; 11:575376.
Article116. Lopez-Pedrera C, Ibañez-Costa A, Perez-Sanchez C, Luque-Tevar M, Patiño-Trives AM, Abalos-Aguilera MDC, et al. Characterization of the protein profile in thrombi of patients with ischemic stroke and identification of potential biomarkers as predictors of negative clinical evolution. Res Pract Thromb Haemost. 2020; 4(Suppl 1):OC08.5.117. Suissa L, Guigonis JM, Graslin F, Doche E, Osman O, Chau Y, et al. Metabolome of cerebral thrombi reveals an association between high glycemia at stroke onset and good clinical outcome. Metabolites. 2020; 10:483.
Article118. Di Meglio L, Desilles JP, Solonomenjanahary M, Labreuche J, Ollivier V, Dupont S, et al. DNA content in ischemic stroke thrombi can help identify cardioembolic strokes among strokes of undetermined cause. Stroke. 2020; 51:2810–2816.
Article119. Di Meglio L, Derraz I, Solonomenjanahary M, Daly D, Chodraui Filho S, Ben Maacha M, et al. Two-layered susceptibility vessel sign is associated with biochemically quantified thrombus red blood cell content. Eur J Neurol. 2020; 27:1264–1271.
Article120. Juega J, Pagola J, Palacio C, Camacho J, Cardona P, Quesada H, et al. Etiology of stroke based on early analysis of clot cytometry obtained through first pass technique for mechanical thrombectomy. Stroke. 2019; 50(Suppl 1):AWMP70.
Article121. Itsekson Hayosh Z, Abu Bandora E, Shelestovich N, Nulman M, Bakon M, Yaniv G, et al. In-thrombus thrombin secretion: a new diagnostic marker of atrial fibrillation in cryptogenic stroke. J Neurointerv Surg. 2021; 13:799–804.
Article122. Boeckh-Behrens T, Kleine JF, Zimmer C, Neff F, Scheipl F, Pelisek J, et al. Thrombus histology suggests cardioembolic cause in cryptogenic stroke. Stroke. 2016; 47:1864–1871.
Article123. Liao Y, Guan M, Liang D, Shi Y, Liu J, Zeng X, et al. Differences in pathological composition among large artery occlusion cerebral thrombi, valvular heart disease atrial thrombi and carotid endarterectomy plaques. Front Neurol. 2020; 11:811.
Article124. Xue Y, Zhao Y, Cao J, Zhu XC, Shao HM, Chen RH, et al. Exploration of thrombus histological composition and clinical effect in mechanical thrombectomy of acute ischemic stroke. Zhonghua Yi Xue Za Zhi. 2018; 98:3697–3700.125. Gong L, Zheng X, Feng L, Zhang X, Dong Q, Zhou X, et al. Bridging therapy versus direct mechanical thrombectomy in patients with acute ischemic stroke due to middle cerebral artery occlusion: a clinical- histological analysis of retrieved thrombi. Cell Transplant. 2019; 28:684–690.
Article126. Berndt M, Prothmann S, Maegerlein C, Oberdieck P, Zimmer C, Hegge B, et al. Artificial stroke clots: how wide is the gap to the real world? World Neurosurg. 2018; 110:e90–e99.
Article127. Bhaskar S, Saab J, Cappelen-Smith C, Cordato D, Cheung A, Manning N, et al. Cryptogenic stroke is linked to cardioembolic aetiology: a histopathological study of thrombus retrieved after endovascular thrombectomy. Eur J Neurol. 2019; 26:20.128. Meng L, Wang H, Yang H, Zhang X, Zhang Q, Dong Q, et al. Nomogram to predict poor outcome after mechanical thrombectomy at older age and histological analysis of thrombus composition. Oxid Med Cell Longev. 2020; 2020:8823283.
Article129. Wolpert F, Kulcsár Z, Hänsel M, Rushing E, Seystahl K, Schweizer J, et al. Embolization of tumor cells is rare in patients with systemic cancer and cerebral large vessel occlusion. Eur J Neurol. 2020; 27:2041–2046.
Article130. Hinman JD, Rao NM, Yallapragada A, Capri J, Souda P, Whitelegge J, et al. Drip, ship, and grip, then slice and dice: comprehensive stroke center management of cervical and intracranial emboli. Front Neurol. 2013; 4:104.
Article131. Ambrosioni J, Urra X, Hernández-Meneses M, Almela M, Falces C, Tellez A, et al. Mechanical thrombectomy for acute ischemic stroke secondary to infective endocarditis. Clin Infect Dis. 2018; 66:1286–1289.
Article132. Bain MD, Hussain MS, Gonugunta V, Katzan I, Gupta R. Successful recanalization of a septic embolus with a balloon mounted stent after failed mechanical thrombectomy. J Neuroimaging. 2011; 21:170–172.
Article133. Distefano M, Calandrelli R, Arena V, Pedicelli A, Della Marca G, Pilato F. A puzzling case of cryptogenic stroke. J Stroke Cerebrovasc Dis. 2019; 28:e33–e35.
Article134. Nakanishi K, Kawano H, Amano T, Omori Y, Kanma H, Hirano T. Stroke due to infective endocarditis diagnosed by the retrieved thrombus: a case report. Rinsho Shinkeigaku. 2018; 58:35–40.
Article135. Sukumaran S, Jayadevan ER, Mandilya A, Sreedharan SE, Harikrishnan S, Radhakrishnan N, et al. Successful mechanical thrombectomy of acute middle cerebral artery occlusion due to vegetation from infective endocarditis. Neurol India. 2012; 60:239–240.
Article136. Sgreccia A, Carità G, Coskun O, Maria FD, Benamer H, Tisserand M, et al. Acute ischemic stroke treated with mechanical thrombectomy and fungal endocarditis: a case report and systematic review of the literature. J Neuroradiol. 2020; 47:386–392.
Article137. Katano T, Sakamoto Y, Kunugi S, Nishiyama Y, Shimizu A, Kimura K. A fungus in a thrombus by mechanical thrombectomy in acute cerebral infarction: a case report. Rinsho Shinkeigaku. 2020; 60:340–345.
Article138. Scharf EL, Cloft HJ, Wijdicks E. Mucor thrombus. Neurocrit Care. 2016; 24:268–272.
Article139. Matsumoto N, Takahashi M, Katano T, Kutsuna A, Kanamaru T, Sakamoto Y, et al. Cholesterol crystal in thrombus removed by mechanical thrombectomy should be a strong marker for aortogenic embolic stroke. J Stroke Cerebrovasc Dis. 2020; 29:105178.
Article140. Usui G, Hashimoto H, Sugiura Y, Nishi Y, Kusakabe M, Horiuchi H, et al. Aortogenic embolic stroke diagnosed by a pathological examination of endovascularly removed thrombus: an autopsy report. Intern Med. 2019; 58:2851–2855.
Article141. Koneru S, Nogueira RG, Osehobo E, Oprea-Ilies G, Al-Bayati AR, Brinjikji W, et al. Clot composition in retrieved thrombi after mechanical thrombectomy in strokes due to carotid web. J Neurointerv Surg. 2021; 13:530–533.
Article142. Mönch S, Boeckh-Behrens T, Berndt M, Maegerlein C, Wunderlich S, Zimmer C, et al. Angiographic baseline proximal thrombus appearance of M1/M2 occlusions in mechanical thrombectomy. Clin Neuroradiol. 2021; 31:189–196.
Article143. Wei L, Zhu Y, Deng J, Li Y, Li M, Lu H, et al. Visualization of thrombus enhancement on thin-slab maximum intensity projection of CT angiography: an imaging sign for predicting stroke source and thrombus compositions. Radiology. 2021; 298:374–381.144. Patel TR, Fricano S, Waqas M, Tso M, Dmytriw AA, Mokin M, et al. Increased perviousness on CT for acute ischemic stroke is associated with fibrin/platelet-rich clots. AJNR Am J Neuroradiol. 2021; 42:57–64.
Article145. Berndt M, Poppert H, Steiger K, Pelisek J, Oberdieck P, Maegerlein C, et al. Thrombus histology of basilar artery occlusions : are there differences to the anterior circulation? Clin Neuroradiol. 2021; 31:753–761.146. Berndt M, Friedrich B, Maegerlein C, Moench S, Hedderich D, Lehm M, et al. Thrombus permeability in admission computed tomographic imaging indicates stroke pathogenesis based on thrombus histology. Stroke. 2018; 49:2674–2682.
Article147. Brinjikji W, Nogueira RG, Kvamme P, Layton KF, Delgado Almandoz JE, Hanel RA, et al. Association between clot composition and stroke origin in mechanical thrombectomy patients: analysis of the Stroke Thromboembolism Registry of Imaging and Pathology. J Neurointerv Surg. 2021; 13:594–598.
Article148. Smith WS, Furlan AJ. Brief history of endovascular acute ischemic stroke treatment. Stroke. 2016; 47:e23–e26.
Article149. Saver JL. Clinical practice: cryptogenic stroke. N Engl J Med. 2016; 374:2065–2074.150. Roessler FC, Kalms N, Jann F, Kemmling A, Ribbat-Idel J, Stellmacher F, et al. First approach to distinguish between cardiac and arteriosclerotic emboli of individual stroke patients applying the histological THROMBEX-classification rule. Sci Rep. 2021; 11:8433.
Article151. Kim JM, Byun JS, Kim J, Park MS, Hong SA, Nam TK, et al. Analysis of microRNA signatures in ischemic stroke thrombus. J Neurointerv Surg. 2021 Jul 8 [Epub]. https://doi.org/10.1136/neurintsurg-2021-017597.
Article152. Abbasi M, Fitzgerald S, Ayers-Ringler J, Espina V, Mueller C, Rucker S, et al. Proteomic analysis of cardioembolic and large artery atherosclerotic clots using reverse phase protein array technology reveals key cellular interactions within clot microenvironments. Cureus. 2021; 13:e13499.
Article153. Suissa L, Guigonis JM, Graslin F, Robinet-Borgomano E, Chau Y, Sedat J, et al. Combined omic analyzes of cerebral thrombi: a new molecular approach to identify cardioembolic stroke origin. Stroke. 2021; 52:2892–2901.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk Factors and Biomarkers of Ischemic Stroke in Cancer Patients
- Application of Artificial Intelligence in Acute Ischemic Stroke: A Scoping Review
- Diagnosis of Cerebrovascular Disease
- The Aspirations of Direct Aspiration for Thrombectomy in Ischemic Stroke: A Critical Analysis
- Considerations When Subtyping Ischemic Stroke in Asian Patients